Introduction
Pregnant women are especially vulnerable when it comes to mental health (Astbury, 2009; Martínez-Vázquez et al., 2023), such as problems related to stress, anxiety, and depression (Bennett et al., 2004; Farrell et al., 2020). Furthermore, during childbirth and postpartum, women are at risk of developing a mental disorder. Despite this, mental health is an aspect that often does not receive sufficient attention in the care provided during these periods (Flores-Ramos, 2013; World Health Organization [WHO, 2020]).
Psychological Symptoms
According to the World Health Organization, more than 1 in 10 women suffer from a mental health problem during pregnancy, mainly depression (WHO, 2020), which is the most common mental disorder among women in the perinatal stage, with a prevalence between 12% and 19% (Martínez-Vázquez et al., 2022).
Obstetric interventions, obstetric violence and previous mental illness are risk factors associated with these problems during and after childbirth, while multiparity, adherence to the mother's birth plan and skin-to-skin contact are protective factors. Maternal physical and psychological health, social support, and support networks are associated with the prevalence of mental health problems during and after childbirth (El Founti Khsim et al., 2022).
Pandemic Played a Role
This risk has been increased during the pandemic (Kovacheva et al., 2022; Motrico et al., 2020; Preis et al., 2020) as a result of the control measures imposed during its critical phases to control its spread (isolation, solitude, social distancing) or the fear of infection. The psychological effects of these measures were already present in the early pandemic phases (Pfefferbaum & North, 2020; Wang et al., 2020). Concerns and fears regarding infection, possible hospitalization, as well as morbidity and mortality, were associated with the pandemic (Ceulemans et al., 2021; Favre et al., 2020; Flores-Ramos, 2013; Westgren et al., 2020).
Another study in a university population reported a 0.9% prevalence of severe anxiety, 2.7% of moderate anxiety, and 21.3% of mild anxiety. Factors such as living in urban areas, social support, stable family income and living with parents were protective factors against anxiety. In addition, having family members or acquaintances infected with COVID-19 was a risk factor for increased anxiety in this population (Puertas-González, Mariño-Narvaez, Peralta-Ramirez, et al., 2021).
Pregnancy and Postpartum
Mental health problems during pregnancy can have negative effect on both mother and the baby, including increased risk of miscarriages, premature births, low birth weight, and higher rates of cesarean sections or instrument-assisted deliveries (Allotey et al., 2020; Kotlar et al., 2021). Postpartum mental health problems have also been described, including the development or worsening of disorders, such as depression, anxiety, and even postpartum post-traumatic stress disorder (Allotey et al., 2020; Ayaz et al., 2020; Ceulemans et al., 2021; Covid-19 and Pregnancy, 2020; Kotlar et al., 2021; Lebel et al., 2020; Mappa et al., 2020; Saccone et al., 2020; Stepowicz et al., 2020; Tariq et al., 2021).
Although there are already data in pandemic reporting an increase in the prevalence of psychological symptomatology in Spain in pregnant women before pandemic and pregnant women during pandemic (Ahmad & Vismara, 2021; Mariño-Narvaez et al., 2021; Miller et al., 2020), there are no studies to date assessing the prevalence of mental health during pregnancy and in the postpartum. Therefore, the objective of this study is to evaluate the psychological symptoms, specifically depression and anxiety, in pregnant women before and during the pandemic.
Method
Study Design
This is a cross-sectional study carried out to assessed psychological profile in a sample of pregnant women selected before the pandemic and a sample of women studied during the first wave of the pandemic.
A total of 122 women were selected prior to the pandemic and 181 women during the COVID-19 outbreak.
Participants and Procedure
Sample Assessed before the COVID-19 Pandemic
The inclusion and exclusion criteria of these women have been previously published. (Romero-González et al., 2018). One hundred and fifty four pregnant women from two health care centres and one general hospital – Góngora Health Center (Granada), Roquetas de Mar Health Center (Almería), and the Poniente Hospital in El Ejido (Almería) – in the south of Spain, voluntarily agreed to participate in the study. The assessment took place during a prenatal appointment with their midwives and obstetrician in the health centres and the hospital, respectively. The inclusion criteria were low-risk Spanish speaking pregnant women aged above 18 years old. Women suffering any pathology before or during pregnancy were excluded. Pregnancies with Cushing's disease, asthma, steroid medication, diabetes, and other conditions that affect cortisol levels were excluded. The study was approved by the Human Ethics Research Committee of the University of Granada, the Biomedical Ethics Research Committee, and the Ethics Research Committee of the Health Centres and the hospital where this study was conducted. Moreover, this study followed the guidelines of the Helsinki Declaration and the Good Clinical Practice Directive (Directive2005/28/EC) of the European Union. Participation was voluntary and an informed written consent document was read and signed by every participant. Participants assessed before the COVID-19 pandemic completed questionnaires at home during each trimester and returned them at their next antenatal appointment. Anxiety and depression symptoms were assessed again after delivery (M = 15.79 days after birth, SD = 9.78). A total of 122 women were included in the present study, as data on the presence of psychopathological symptoms during pregnancy and postpartum were available.
Sample Assessed in 2020, during COVID-19 Lockdown
Eligible participants were European Spanish speaking pregnant women selected in Spain according to the definition established on the Pregnancy Health Document for a low-risk pregnancy and absence of medical and mental diseases. Inclusion criteria also required proficiency in the Spanish language and ≥ 18 years old. The study was approved by the Biomedical Ethics Research Committee of Andalusia (Spain), named PEIBA, Number 0904-N-20. This study also conformed to the guidelines of the Helsinki Declaration and the Good Clinical Practice Directive (Directive 2005/28/EC) of the European Union for human research. Participation was voluntary. An informed written consent document was signed by every participant. A total of 225 women were invited to participate while attending an antenatal appointment with a midwife in the South of Spain during the COVID-19 pandemic from April to June 2020. Participants were recruited from the Department of Obstetrics and Gynaecology of the Antequera Hospital through consecutive admissions. Forty-one women declined to participate due to lack of time, and 15 women were excluded from analyses due to not meeting inclusion criteria. After consent to participate in the study, 25 women were excluded since they did not provide psychological or obstetric information. The sample consisted of 181 pregnant women. Participants assessed during the COVID-19 pandemic completed questionnaires through a phone interview.
Sociodemographic Variables
The variables collected in both population samples were sociodemographic variables: age, marital status, educational level, employment status and country of origin, and other obstetric variables: number of previous abortions, gestational age, parity, whether the pregnancy was wanted, and type of pregnancy.
Instrument
Symptom Checklist-90 Revised (SCL-90-R)
The SCL-90-R was used to assess psychopathological symptomatology (Derogatis, 1983), specifically two symptomatic dimensions, since women from both samples provided this data to compare: depression and anxiety (Cronbach's alpha = .72 to .86 across subscales) (Caparrós Caparrós et al., 2007). It is an easy-to-administer inventory that can be self-reported on a wide age range (13 to 65 years), with 90 items, on a 5-point Likert scale of response from 1 = not at all to 5 = very much. It can be used in both the community and clinical settings.
Confounding Factors
All analyses were adjusted for confounding variables found in the literature as well as those variables that were significantly different between the two samples: marital status, employment status, and level of studies (Puertas-González, Mariño-Narvaez, Peralta-Ramirez, et al., 2021).
Statistical Analysis
Sociodemographic variables, obstetric variables and psychopathological symptomatology scores were compared between two samples of women using Student's t-test, for numerical variables, and Pearson's chi-square, for categorical variables. Adjusted logistic regression was performed to analyse the variables associated with the presence of depression and anxiety during pregnancy, and the occurrence of postpartum depression and anxiety. Finally, binary logistic regression was performed to analyse the variables related to the manifestation of depression and anxiety during and after pregnancy, dichotomizing these variables according to the score equal to 75 on the SCL-90 test (Karlsson et al., 2021). Data were analyzed with SPSS Version 22.0.
Results
Socio-demographic and obstetric variables of the two samples of pregnant women before and during the pandemic are presented in Table 1. As shown, the majority of women in both samples were married or cohabiting. However, in the sample collected during the pandemic there was a higher percentage of women who were divorced or single mothers (2.5 vs. 8.3%, p = .027). The number of unemployed women was significantly higher in the sample collected during the pandemic (17.2 before vs. 29.8% during, p = .008). No significant differences were found in nationality or primiparity between the two samples. However, the percentage of female university students collected before the pandemic was significantly higher than in the sample collected during the pandemic (76.2 vs. 44.8%, p < .01). Most pregnancies were planned, although the number of unwanted pregnancies was slightly higher in the sample collected during COVID-19.
Table 1. Descriptive Data of Women Included in the Comparison Study between Pre-pandemic and COVID-19 Pandemic Period.
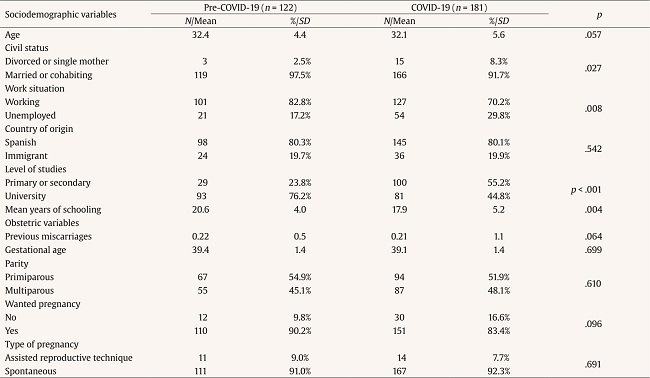
Note.SD = Standard deviation.
Pearson's χ²-squared test for categorical variables and Mann-Whitney's U-test for numerical variables.
When depressive and anxious symptomatology scores during and after pregnancy were compared using SCL-90 tests during pregnancy, significantly higher scores were observed in women studied during the pandemic in all cases (Figure 1 and Table 2). Women interviewed during the pandemic showed higher levels of anxiety and depression scores than women assessed before the pandemic (M = 42.6 vs. 54.6 and M = 51.7 vs. 62.6, respectively). Regarding the depression and anxiety postpartum scores, these were lower than during pregnancy, but still higher in the sample of women assessed during the pandemic (M = 35.0 vs. 50.2 and 36.02 vs. 51.3 respectively).

Figure 1. Psychopathological Symptoms and Psychological Stress Comparison between pre- and COVID-19 Pandemic Periods in Pregnant Women.
Table 2. Logistic Regression of Factors Associated with Psychopathological Symptoms and Psychological Stress.

Note.CI = confidence interval; OR = odds ratio.
Anxiety and depression during pregnancy and in postpartum were assessed with SCL-90-R. Table 2 shows the logistic regression of factors associated with psychopathological symptoms and psychological stress in pregnant women. Being a pregnant women surveyed during the covid pandemic outbreak was directly associated with > 70 depression symptoms score on the SCL-90 scale, adjusting for covariates (aOR = 8.67, 95% CI [3.26, 23.02], p < .001; Nagelkerke's R2 = .244). Anxiety during pregnancy was higher in the group of women interviewed before the pandemic (aOR = 5.1, 95% CI [2.53, 10.44], p < .001; Nagelkerke R2 = .207). Postpartum depression was associated with the pandemic stage and with higher maternal age (aOR = 7.61, 95% CI [2.7, 21.47], p < .001; ) and (aOR = 1.09, 95% CI [1.0, 1.2], p < .001 respectively; Nagelkerke's R2 = .205). None of the variables in the model were significantly associated with postpartum anxiety.
Discussion
The main objective of this study was to evaluate the presence of psychological symptoms, specifically depression and anxiety, in two samples of pregnant women assessed before and after the outbreak of the COVID-19 pandemic. The sample formed by the 122 women that participated belonged to the sample before the pandemic and 181 women were part of the sample during the pandemic. During pregnancy, the presence of anxiety and depression were mostly observed in pregnant women during the pandemic, as well as postpartum disorders such as anxiety and depression. Regarding the factors that were associated with psychopathological symptoms in pregnant women, being pregnant during the pandemic was also associated with a risk of depressive symptoms. In addition, women who were pregnant during the pandemic had increased anxiety during pregnancy. One of the main factors associated with postpartum depression is age. Ceulemans et al. (2021) found in their study that psychopathological problems and general mental health status are worse in women who had unplanned pregnancies, with stress, anxiety, and depressive disorders being predominant. Although in our study there was a majority of unplanned pregnancies during the pandemic, we cannot conclude that it acted as a factor influencing anxiety or depressive disorders since no statistically significant differences were observed.
Pregnancy and Postpartum during Pandemic
During pregnancy, the presence of distress, anxiety, and depression was mainly observed in the sample during the pandemic, as were postpartum disorders such as anxiety and depression. This finding is consistent with previous studies conducted by various authors (Allotey et al., 2020; Ayaz et al., 2020; Ceulemans et al., 2021; Covid-19 and Pregnancy, 2020; Kotlar et al., 2021; Lebel et al., 2020; Mappa et al., 2020; Saccone et al., 2020; Stepowicz et al., 2020; Tariq et al., 2021). Our study also adds to the available evidence the possibility of comparing two very similar samples and examining the effect of the pandemic and confinement on their psychological health and mental well-being (Ahmad & Vismara, 2021; Manchia et al., 2022; Tomfohr-Madsen et al., 2021). Ahmad & Vismara (2021) highlight the importance of carrying out subsequent follow-ups to assess the long-term effects. Being pregnant during the pandemic was associated with greater anxiety during pregnancy as well as a higher risk of developing depressive symptoms during and after it, which is consistent with other findings (Manchia et al., 2022; Tomfohr-Madsen et al., 2021). In a meta-analysis, Manchia et al. (2022) evaluated a sample of more than 40,000 people with increases in anxiety and prevalence figures due to the pandemic, both in the general population and in pregnant women. However, Zhou et al. (2020) state that being pregnant during the pandemic reduces the risk of depressive symptoms, anxiety or post-traumatic stress disorder. These authors consider pregnancy as a protective factor for mental health that may give pregnant women an advantage over non-pregnant women during the pandemic, which may be due to the accessibility to health resources, which is prioritized for pregnant women due to their vulnerability state. Other authors also argue that pregnancy is a period that favors the reduction of anxiety, possibly due to physiological changes (Lübke et al., 2017).
Age Appears as Decisive Factor
Our result revealed that age is one of the main factors associated with postpartum depression, which contrasts with previous studies. For instance, Tariq et al. (2021) found that maternal depression is associated with a lower age at conception or pregnancy, but the risk does not increase at an older age. However, other authors do not find the presence of this association and conclude that maternal age does not interact with the development of postpartum depression (Hartmann et al., 2017; Upadhyay et al., 2017). In contrast, there are studies that report similar results to ours (Oyetunji & Chandra, 2020). Oyetunji and Chandra (2020) conducted a systematic review of publications between 1995 and 2019 including a total of 74 articles that were reviewed and summarized. The authors found a relation between increased maternal age and postpartum depression, thus concluding more research is needed as age is not a modifiable factor. This seems to indicate that maternal age may act as both a risk and even protective factor for the appearance of postpartum depression. Therefore, future research should continue to investigate the role of maternal age in postpartum depression and study its long-term effects. In addition, given the controversial results regarding age as protective or risk factor found in different studies, healthcare professionals must take appropriate measure with these women, especially in those cases of young women or older women.
Strengths and Limitations
Nevertheless, the present study has some limitations. Selection bias was considered, existing a difference in educational level between the two samples of women included in the study, which could have affected our results. Among women assessed during the pandemic, a higher percentage of unemployed women were observed. This was due to the severe social crisis caused by the restrictive measures implemented to curb the spread of the virus. Concerning housing, the sample before the pandemic was mostly married or cohabiting women, while the sample during the pandemic was mostly divorced, or single mothers. Regarding pregnancy, although they were mostly sought, in the sample during the pandemic we found most unplanned pregnancies. Another limitation of the study is the absence of information on a history of psychopathological symptoms in the sample which could potentially have acted as cofounding bias. However, it should be mentioned as strengths of the present study that all the scales used in the study have been validated in populations similar to the research sample (Caparrós Caparrós et al., 2007; Cohen et al., 1983; Derogatis, 1983; Remor, 2006). In addition, it should be noticed that all the participants were pregnant women over 18 years of age, who spoke Spanish, and were users of the regional health system of Andalusia and could not have had a history of psychopathological problems and may have developed them during the pandemic, since mental health problems that affect pregnancy, childbirth, and the postpartum period could arise spontaneously (Stranges et al., 2014). The results showed the importance of giving healthcare professionals strategies or protocols based on prevention (Kovacheva et al., 2022) to care for those women affected. An appropriate technique claimed by other researchers appears to be the cognitive behavioural therapy, even if this technique is used online (Puertas-González, Mariño-Narvaez, Romero-González, et al., 2021; Puertas-González et al., 2022).
Conclusion
Being pregnant during the pandemic increased the risk of anxiety and depression, as well as postpartum disorders such as anxiety and depression. The main factor associated with postpartum depression was maternal age which, in turn, generated the most controversy, which highlights the importance of studying the long-term effects of the pandemic on the mental health of pregnant women.














