Introduction
Peripartum depression (PPD) is a complex and prevalent condition, considered among the most common mental health problems during pregnancy and after childbirth (O'Hara & Wisner, 2014). Recent review papers have highlighted a global pooled prevalence of around 17% for elevated symptoms of PPD (Dadi et al., 2020; Shorey et al., 2018; Wang et al., 2021). However, significant cross-cultural variations in PPD prevalence are established, ranging from 15% to 65% during pregnancy (Dadi et al., 2020) and 3-38% postpartum (Hahn-Hoolbrook et al., 2018). Moreover, recent systematic reviews found a particularly high prevalence of PPD in low-income countries compared to high-income countries (Dadi et al., 2020; Wang et al., 2021). Also, levels of PPD symptoms show fluctuations over time rather than a stable trajectory, with the highest prevalence shown during pregnancy and a trend of symptom reduction after childbirth (Wilcox et al., 2021).
Since the edition of the DSM-5 (American Psychiatric Association [APA, 2013]), the time frame for the onset of postpartum depression broadened to include the entire peripartum period. Therefore, PPD is considered an episode of depression occurring during pregnancy or up to one month postpartum and characterised by symptoms such as depressed mood, diminished interest or pleasure, appetite and/or sleep changes, fatigue, excessive guilt, etc. (APA, 2013). As numerous studies have established that peripartum depression can occur even a year postpartum (Banti et al., 2011), the literature most often considers pregnancy and the entire year following childbirth as the framework for PPD onset.
PPD is associated with various adverse effects for the mother, child, and the entire family. Women with PPD tend to have a lower quality of life (J. Li et al., 2022), poorer pregnancy outcomes (Jahan et al., 2021), bonding difficulties, and weaker interactions with their children (Mantis et al., 2019; Tolja et al., 2020). Children, in turn, are at risk for developmental, behavioural, and mental health difficulties (Pawlby et al., 2009; Slomian et al., 2019). Recently, attention was drawn to PPD in fathers, demonstrating a positive relationship with maternal PPD (Ansari et al., 2021) and weaker father-infant interactions (Goodman et al., 2008), thus showing that PPD impacts the entire family. Additionally, since the COVID-19 outbreak, an increased prevalence of depression and anxiety among pregnant and postpartum women has been uncovered (Mateus et al., 2022).
Despite the available effective treatment options, PPD detection and treatment rates are low (Geier et al., 2015) and burdened by many challenges. Most European countries lack clinical practice guidelines for PPD, or the existing recommendations substantially vary, leading to diverse management of PPD across Europe (Motrico et al., 2022). In addition, women rarely seek help due to numerous obstacles, such as stigma and lack of knowledge or information about PPD (Jones, 2022).
Research is ambiguous about whether PPD is distinct from depression occurring outside the peripartum period. However, there is an inclination toward the distinctiveness of PPD in the early postpartum period due to symptom severity and hormonal, genetic, and epigenetic mechanisms that differ from non-peripartum depression (Batt et al., 2020). Moreover, PPD is specific as it is accompanied by significant biological changes that may also affect mood and potentially carries long-lasting adverse effects on both mother and children (Yim et al., 2015).
For decades, scientists have sought to disentangle the complexity of PPD. Evidence is now clear that PPD is a heterogenous disorder with variability in onset, severity, symptoms, and course (Kettunen et al., 2014). So far, a promising theoretical model to explain the pathogenesis of PPD is the general biopsychosocial model developed by George Engel in 1977. Engel's (1977) groundbreaking paper was a response to a widespread, reductionistic biomedicine model which assumed disease to be entirely accounted for by biological variables, neglecting social, behavioural, and psychological dimensions. Conversely, the biopsychosocial model is an integrative framework that equalises the relevance of biological, psychological, and social factors and proposes that all three domains inextricably contribute to health and disease (Engel, 1977). Only recently, the biopsychosocial approach within the perinatal research has gained more attention, covering various topics, such as high-risk pregnancy (Bera et al., 2019), perinatal suicidal ideation (Bright et al., 2022), obstetric outcomes (Meems et al., 2020), and other. Even though this model represents a more comprehensive view of health, advances away from the former biomedical approach are happening rather slowly (Havelka et al., 2009), which is also evident in studies of peripartum mental health.
Evidence suggests that the biological and psychosocial mechanisms of PPD are not distinct; instead, they interact together (Guintivano et al., 2018; Yim et al., 2015), thus supporting fundamental postulates of a biopsychosocial framework. Specifically, the risk for PPD is shaped by various biological factors – e.g., (epi)genetic factors, inflammatory markers – that are moderated or mediated by psychosocial settings (e.g. high stress, low income), which directs towards an integrative, biopsychosocial approach in examining the complexity of PPD (Yim & Dunkel Schetter, 2019). Over the years, several proposed biopsychosocial models emerged from the literature focusing on depression during pregnancy (Naja et al., 2021), postpartum (Halbreich, 2005; Lara-Cinisomo et al., 2016), or both (English et al., 2018; Ross et al., 2004). For example, a more recent model by English et al. (2018) suggested that various antenatal stressors, personal resources, and certain predisposing factors predict PPD depending on symptom onset and persistence. However, the biopsychosocial models of PPD have divergent conceptualisations and propose different causal pathways and risk factors contributing to PPD vulnerability. Integrative studies of PPD are emerging (Yim & Dunkel Schetter, 2019), yet they are still scarce and marked by methodological heterogeneity, resulting in an insufficient understanding of this disorder. Other review papers have critically assessed integrative PPD research (Yim & Dunkel Schetter, 2019; Yim et al., 2015), but none so far has systematised existing biopsychosocial models of PPD.
The aim of this narrative review is to: (1) provide an overview of the current state of the science on PPD risk factors and biopsychosocial theoretical models, (2) highlight the main challenges and perspectives of biopsychosocial research, and (3) identify gaps in the literature and outline directions for future research and clinical practice.
Method
A literature search was performed on several electronic databases (e.g., PubMed/Medline, PsychInfo). Broad search terms were peripartum depression (e.g., peripartum depression OR perinatal depression OR antenatal depression OR postnatal depression OR postpartum depression), risk factors (e.g., risk factors OR determinants OR predictors OR biological risk factors OR psychosocial risk factors OR psychological risk factors OR social risk factors), and biopsychosocial model (e.g., biopsychosocial model OR biopsychosocial framework OR biopsychosocial approach OR biopsychosocial theory OR integrative model OR integrative approach). Inclusion criteria were studies in peer-reviewed journals written in English and focusing on the risk factors or biopsychosocial models of depression during the perinatal period. Recent systematic reviews, meta-analyses and umbrella reviews on the risk factors of PPD and papers conceptualising biopsychosocial models of PPD were prioritised. Newer and more recent studies were included. The narrative review summarised and critically overviewed the current body of relevant literature on the state of the science on risk factors and biopsychosocial models of PPD and outlined the main directions for future integrative studies and clinical practice.
Results
Findings from most recent reviews regarding biological and psychosocial risk factors were summarised, and integrative studies that investigated the interrelationships between PPD risk factors were discussed. Proposed biopsychosocial models of PPD were outlined and critically overviewed.
Biological Risk Factors of PPD
Given that significant hormonal fluctuations and physiological adaptations underline the peripartum period, it is assumed that sensitivity to hormonal changes (e.g., reproductive hormones), hypothalamic-pituitary-adrenocortical (HPA) dysregulation, inflammatory processes, estrogen signalling, and genetic vulnerabilities are critical elements of biological vulnerability to PPD (Payne & Maguire, 2018; Yim et al., 2015). A recent umbrella review of over 3 million women found that premenstrual syndrome (PMS) was the most robust factor, doubling the risk for PPD in the postpartum period (Gastaldon et al., 2022). Such findings align with other recent reviews (Amiel Castro et al., 2019; Kim et al., 2022) and support the hypothesis that a certain affective sensitivity to hormonal changes underlies both conditions. Similarly, one finding showed that affective but not psychosomatic symptoms of PMS strongly predict depression symptoms during pregnancy (Abe et al., 2023). Other proposed biological commonalities associated with PMS and PPD are genetic factors, the immune-inflammatory response, and the imbalance in the serotonergic system (Amiel Castro et al., 2019).
The genetic heritability of PPD is around 50% and one-third of the genetic contribution is unique to PPD and not shared with non-perinatal depression (Viktorin et al., 2016). Potential candidate gene biomarkers of depression in the postpartum are serotonin transporter, tryptophan hydroxylase (TPH), catechol-o-methyl transferase (COMT), monoamine oxidase (MAO), brain-derived neurotrophic factor (BDNF), and their polymorphisms (e.g., serotonin-transporter-linked polymorphic region polymorphism) (Gastaldon et al., 2022; Payne & Maguire, 2018). Epigenetic studies primarily focus on DNA methylation and are showing promising results (Yu et al., 2021).
Regarding health-related factors, there is evidence linking inflammatory processes and PPD (e.g., interleukin-6), suggesting that they share some molecular mechanisms (Guintivano et al., 2016; Serati et al., 2016). Next, systematic reviews and meta-analyses found evidence supporting a history of mental illness as a risk factor (Biaggi et al., 2016; Dadi et al., 2020; Guintivano et al., 2018; Yang et al., 2022) or, more specifically, a history of depression (Zhao & Zhang, 2020). Considering metabolic health, gestational diabetes was identified as a risk factor in more recent reviews (Gastaldon et al., 2022; Zhao & Zhang, 2020). Few studies identified anthropometric risk factors of PPD, such as maternal pre-pregnancy obesity or overweight status (Zhao & Zhang, 2020), and higher gestational weight gain (Žuti et al., 2023).
Considering pregnancy-related factors, in a review by Gastaldon et al. (2022) moderate evidence for PPD risk was found for emergency caesarean section and weak evidence for preterm delivery, vitamin D deficiency, and anaemia during pregnancy and postpartum. Pregnancy complications were identified as a risk factor, as well (Biaggi et al., 2016; Dadi et al., 2020). Findings on parity were inconsistent, with some reviews identifying multiparity (Yang et al., 2022; Zhao & Zhang, 2020), primiparity (Kim et al., 2022), or no association with postpartum depression (Gastaldon et al., 2022).
Studies combining multi-omics technologies, a novel, cutting-edge approaches to identifying PPD biomarkers, including genomics, epigenomics, transcriptomics, proteomics, metabolomics, and lipidomics show great potential for unravelling biological pathways of PPD (Yu et al., 2021). A recent review summarised metabolic alterations related to PPD, such as kynurenine, kynurenic acid, eicosapentaenoic acid, and dysregulations in steroid metabolism or amino and fatty acids metabolism (S. Li et al., 2022).
Although the exact biological underpinnings of PPD are yet to be established (Guintivano et al., 2018), in-depth analyses of the interplay of biological risk factors for PPD could provide a basis for a more accurate risk assessment. Furthermore, advances in biomarker research and biological psychiatry can facilitate the evolution of biopsychosocial models in reproductive and infant psychology (Curran & Alderdice, 2016).
Psychosocial Risk Factors of PPD
Literature on psychosocial or environmental factors of PPD is better established and more conclusive (Yim et al., 2015). As the whole peripartum period is demanding and stressful, stress was often a topic of interest within perinatal research. Stressful life events and perceived stress are considered integral factors shaping the vulnerability to PPD (Biaggi et al., 2016; Guintivano et al., 2018; Hutchens & Kearney, 2020; Lancaster et al., 2010). Similarly, evidence was also found for symptoms of anxiety robustly associated with PPD either during pregnancy (Lancaster et al., 2010) or postpartum (Kim et al., 2022).
A substantial body of systematic literature revealed that current or past violent experiences of abuse and domestic or intimate partner violence are among the strongest and most prominent risk factors for PPD (Biaggi et al., 2016; Dadi et al., 2020; Gastaldon et al., 2022; Hutchens & Kearney, 2020; Kim et al., 2022; Yang et al., 2022; Zhao & Zhang, 2020). In addition, low social support or relationship quality is a well-established risk factor for PPD (Dadi et al., 2020; Lancaster et al., 2010; Yim et al., 2015; Zhao & Zhang, 2020), confirming that quality support is particularly important for maternal mental health during the sensitive peripartum period.
Some personal resources and personality characteristics are also implicated in PPD vulnerability, such as neuroticism, vulnerable personality style (e.g., frequent worry, sensitivity, unassertiveness, etc.), trait anxiety (Puyané et al., 2022), and perfectionism (Bull et al., 2022). Maternal lifestyle and behaviour, such as smoking or alcohol use, are also associated with PPD (Dadi et al., 2020; Kim et al., 2022; Yang et al., 2022). One review identified two protective behavioural factors, skin-to-skin contact, and certain healthy dietary habits (seafood consumption and multivitamin supplementation) (Zhao & Zhang, 2020).
Related to pregnancy and childbirth, risk factors for PPD were a traumatic childbirth experience (Zhao & Zhang, 2020) and an unintended or unwanted pregnancy (Gastaldon et al., 2022; Qiu et al., 2020) with higher risk detected among primiparous women (Dadi et al., 2020).
Socioeconomic (SES) factors relate to a person's position compared to others in terms of education, income, employment, and insurance status (Guintivano et al., 2018). Lower educational level, poor economic status (Dadi et al., 2020; Kim et al., 2022; Lancaster et al., 2010; Yang et al., 2022), and immigrant status (Zhao & Zhang, 2020) are some SES factors related to exacerbated risk for PPD. The importance of cultural context is additionally confirmed by substantial cross-cultural variations in PPD prevalence across the entire perinatal period in favour of developed or high-income countries (Dadi et al., 2020; Halbreich & Karkun, 2006; Wang et al., 2021). PPD epidemiology is, therefore, partly shaped by income inequalities and geographic development (Wang et al., 2021). Moreover, global PPD variations could be explained by immigrant status or experienced discrimination in some ethnic/racial groups that represent forms of chronic stress (Guintivano et al., 2018). On the other hand, cultural rituals that women perceive as helpful, such as resting after childbirth and support from extended family, have a positive impact on their postpartum mood (Bina, 2008).
It is shown that some environmental risk factors (e.g., adverse life events, lower socioeconomic status) share together that they elevate stress levels and alter the HPA axis, which might exacerbate the underlying genetic predisposition to PPD (Guintivano et al., 2018). However, most current umbrella and systematic reviews focus only on postpartum depression and demonstrate a relatively low to intermediate quality of reviewed studies which hinders conclusion (Gastaldon et al., 2022; Hutchens & Kearney, 2020).
Biopsychosocial Models of PPD
Lacking to explain the majority of variance in PPD throughout research, it became evident that PPD vulnerability derives from the complex interrelation of predisposing factors embedded into a psychosocial context. Based on this knowledge, studies attempted to address the growing need for a unified biopsychosocial framework in PPD research. Several studies that proposed the biopsychosocial model of PPD are outlined chronologically.
Among the first that followed Engel's framework in PPD research were Ross et al. (2004), who developed a “biopsychosocial model of perinatal mood changes”, which showed that the relationship between biological factors (plasma progesterone, personal and family history of depression) and PPD is partially mediated through psychosocial stressors and anxiety symptoms. No direct effects were found, demonstrating that the relationship between biological factors and PPD can only be elucidated in the context of relevant psychosocial factors (Ross et al., 2004). Interestingly, the model had a good fit for pregnancy but not postpartum data, suggesting different causal pathways for antenatal and postpartum depression symptoms.
Halbreich (2005) proposed a “bio-psychosocial-cultural model of the processes leading to postpartum disorders” that suggests that the main etiological factor for postpartum disorders (PPD or other reproductive-related disorders) is a genetic predisposition to reproductive-related disorders, a dynamic vulnerability that is shaped throughout an individual's life. Responding to biological and social triggers and depending on the perinatal environment, perception, and coping mechanisms, symptoms of the postpartum disorder can occur. The model represents a broad and complex conceptualisation of traits (e.g., predisposition to reproductive-related disorders), states (e.g., dysphoria), environment (e.g., negative and positive life experiences), and cultural mechanisms (e.g., family support system, healthcare utilisation, attitudes about motherhood) underpinning postpartum disorders. It also emphasises that cultural aspects require more attention, specifically to provide a distinction between universal and culturally-specific processes. This model was praised for its biological sophistication and for including cultural aspects as important moderators (Yim et al., 2015); however, it relates to both PPD and other reproductive-related disorders, which needs empirical support.
Lara-Cinisomo et al. (2016) proposed a “biopsychosocial conceptual model of postpartum depression risk”, specifically for immigrant and U.S.-born Latina women in the U.S. Authors argue for developing an integrated model designed to assess psychosocial and physiological risk factors in a high-risk population. The model accounts for culturally- and contextually-relevant psychosocial stressors (e.g., lifetime poverty and trauma, immigrant status, acculturative stress, discrimination) and neurobiological factors (dysregulation in the HPA axis, lower levels of oxytocin) related to PPD after childbirth. They propose that psychosocial stressors relate to PPD both directly and indirectly, through neurobiological factors. This model contributed to the current body of literature on integrative PPD theory by including the role of neuroendocrine function and specific chronic stressors that immigrant women can experience.
Deriving from previous models, English et al. (2018) proposed the “biopsychosocial model of perinatal depression”, a modified version of the “psychosocial model” conceptualised by Leigh and Milgrom (2008). This model proposes that antenatal stressors (antenatal anxiety, major life events), personal resources (low self-esteem, negative cognitive style and low social support), and predisposing factors (low SES, unhealthy lifestyle, young age, lower education, history of anxiety or depression, and family history of PPD) predict antenatal and postpartum depression (English et al., 2018). The authors also suggested that the predictive power of sociodemographic and lifestyle factors for PPD decreases and that of personal or family history of depression or PPD increases from pregnancy to postpartum. The model included various confounders in regression analyses and demonstrated the fluctuation in the relevance of different risk factors moving from the antenatal to the postpartum period. However, it did not consider biological factors in greater depth, interaction effects, nor did it include some factors (e.g., violent experiences) that showed a strong relationship with PPD across the literature (Biaggi et al., 2016; Dadi et al., 2020).
Next, Naja et al. (2021) proposed the expanded “comprehensive biopsychosocial model of antenatal depression”, built upon prior models (English et al., 2018; Leigh & Milgrom, 2008; Ross et al., 2004) which acknowledges the role of sociodemographic factors, psychosocial indicators, and individual biology but expands the model with modifiable factors such as negative psychosocial-behavioural interaction and resilience as risk factors for antenatal depression. The model consists of predisposing factors on three dimensions: sociodemographic factors (e.g., low income, young age), biological factors (personal or family history of mental health problems), and pregnancy-related health factors (e.g., gestational diabetes, acute, and chronic diseases, or unwanted pregnancy). The next dimension is negative psychosocial-behavioural factors that include psychosocial stresses (e.g., intimate partner violence, low social support, life events), unhealthy behavioural factors (e.g., low physical activity, smoking or alcohol use), and pregnancy-related anxiety (e.g., fear of giving birth, concerns about appearance), which interact and shape low resilience, contributing to PPD. Their study on women in Qatar revealed that prior use of mental health medications, gestational diabetes, pregnancy-related anxiety, low social support, and low resilience were associated with antenatal depression. The model discriminated between depressed and non-depressed women with 89% accuracy. As in most previous models, biological measurements seem underrepresented, though an interesting novelty is greater attention to a variety of pregnancy-related health and anxiety factors, as well as resilience in shaping PPD risk.
Integrative Studies on PPD
Two different bulks of literature on PPD exist, a biological and psychosocial one, both of which evolved separately and remained largely distinct (Yim et al., 2015). Integrative, biopsychosocial studies on PPD are emerging, but rather slowly, as is evident from a recent review that identified only 15 integrative studies (Yim & Dunkel Schetter, 2019). The summary of these integrative studies in greater depth is elsewhere (Yim & Dunkel Schetter, 2019; Yim et al., 2015), and a synthesis of some recent findings and reviews is outlined below.
Many integrative studies found a positive relationship between the observed biological variables and PPD only under certain psychological contexts (Figueiredo et al., 2015; Yim & Dunkel Schetter, 2019), confirming the gene x environment interaction hypothesis, which postulates that genetic vulnerabilities interact with environmental factors in shaping PPD risk (Zhang et al., 2014). A review by Yim and Dunkel Schetter (2019) showed that recent integrative studies focused on oxytocin, inflammatory markers, HPA axis function, adiponectin, and cortisol as biological factors, and stress, childhood abuse, neuroticism, attachment style, perceived support, and marital status were some psychosocial moderators or mediators.
As the role of stress in PPD risk is extensive, it is proposed that the negative effect of stress on PPD occurs through several biological processes, such as neuroendocrine function (e.g., dysregulation in the HPA axis) and interaction with genetic and epigenetic mechanisms (Elwood et al., 2019; Lara-Cinisomo et al., 2016; Payne & Maguire, 2018). For example, the interaction between environmental factors and 5-HTTLPR polymorphism for PPD during the postpartum was found in several papers (Figueiredo et al., 2015). Recent studies found that the postpartum depression risk was associated with interactions between the glucocorticoid receptor gene and a negative birth experience (Plieger et al., 2023) and a higher postpartum placental corticotropin-releasing hormone interacting with the mineralocorticoid receptor genotype (Gutiérrez-Zotes et al., 2020). A systematic review by Elwood et al. (2019) found that genetic factors, including polymorphisms in several genes (e.g., HMNC1, COMT, MAOT, PRKCB, ESR1, and SLC6A4) in the presence of stressful life events, were associated with depression symptoms in the postpartum period. Interestingly, if the postnatal period occurred during autumn and winter, PPD showed positive associations with polymorphisms in the BDNF gene and with OXT and OXTR genes if women experienced childhood adversity. Epigenetic interactions (mostly in DNA methylation studies) were identified with genotype, estrogen, and childhood adversity (Elwood et al., 2019), highlighting the inseparable role of both (epi)genetic and environmental influences for PPD.
To summarise, gene x environment studies provide insight into the complexity of PPD, but the influence of genetic factors (e.g., serotonin transporter gene) was more profound when methodological heterogeneity was taken into consideration, such as the timepoint of assessment (e.g., early vs late postpartum), the relationship with environmental factors (e.g., stress, socioeconomic status), and measuring instruments for PPD (Figueiredo et al., 2015). Moreover, existing studies are focused on diverse biological factors and methodologies that resulted in difficult replications and between-study comparisons. Adding to the complexity of the topic, different characteristics related to five PPD trajectory groups were found (Wikman et al., 2020), which might explain the inconsistent results among studies. However, childbirth is a well-defined environmental factor enabling a relatively homogeneous sample (Costas et al., 2010), and the peripartum period can be considered as a standardised stressful period suitable for the gene x environment interaction studies (Doornbos et al., 2009).
Discussion
This narrative review aimed to summarise the current state of the science regarding biological and psychosocial risk factors of PPD and provide an overview of biopsychosocial models of PPD. In general, many studies focused only on several risk indicators and did not test interaction effects or the interrelationships between the biological and psychosocial factors per se. Furthermore, gene x environment interactions were consistently observed but greatly dependent upon the timing of the assessments (Figueiredo et al., 2015; Yim et al., 2015). The main biopsychosocial theories of PPD in the literature are the biopsychosocial model of perinatal mood changes (Ross et al., 2004), the bio-psychosocial-cultural model of the processes leading to postpartum disorders (Halbreich, 2005), the biopsychosocial conceptual framework of postpartum depression risk (Lara-Cinisomo et al., 2016), the biopsychosocial model of perinatal depression (English et al., 2018), and the comprehensive biopsychosocial model of antenatal depression (Naja et al., 2021).
The chronological development of complexity and specificity among the biopsychosocial models of PPD is apparent, displaying the evolution of the biopsychosocial paradigm in PPD research. In general, integrative theoretical models and studies provide an exceptional opportunity for a deeper understanding of PPD and give promising directions for future studies. However, some challenges still exist, for example, models theorised on depression symptoms in pregnancy, postpartum, or both, thus pointing to possible distinct underlying mechanisms. A review by Figueiredo et al. (2015) suggested that the distinction between antenatal and postnatal depression can still be useful for understanding the pathophysiology of PPD, especially when focusing on genetic factors. A diverse conceptualisation of PPD aetiology and causal pathways and a lack of replication or empirical support for the models are noticed. Notably, the variables constituting a biological dimension of PPD differed the most across the models and are represented to varying degrees. Furthermore, some models neglected biological variables or more specific contextual and cultural factors that have robust support from the literature.
The Biopsychosocial Model of Peripartum Depression
Based on the most recent systematic evidence in the field, we categorised risk factors for PPD within the broad “biopsychosocial model of peripartum depression”, deriving from Engel's (1977) general “biopsychosocial model”, as presented in Figure 1. The most prominent biological factors for PPD are physical and mental health history (e.g., PMS, personal or family history of mental illness) and endocrine (e.g., reproductive hormones), metabolic (e.g., gestational diabetes), obstetric (e.g., emergency caesarean section, pregnancy complications), genetic and epigenetic (e.g., serotonin transporter gene, glucocorticoid receptor gene), immunological (e.g., interleukin-6), and biochemical (e.g., anaemia, vitamin D deficiency) factors. Psychological factors are related to stress, unplanned or unwanted pregnancy, anxiety, personal resources (e.g., personality traits), and an unhealthy lifestyle (e.g., smoking or alcohol use). Social factors include past or current violent experiences, social support, relationship quality with the partner, socioeconomic status, cultural context (e.g., racial or ethnic minority, immigrant status), and demographic characteristics (e.g., lower education). The interrelationship between these three dimensions contributes to antenatal or postpartum depression vulnerability; therefore, delineating the interplay among them is essential, as indicated by the literature (Figueiredo et al., 2015; Yim & Dunkel Schetter, 2019; Yim et al., 2015).
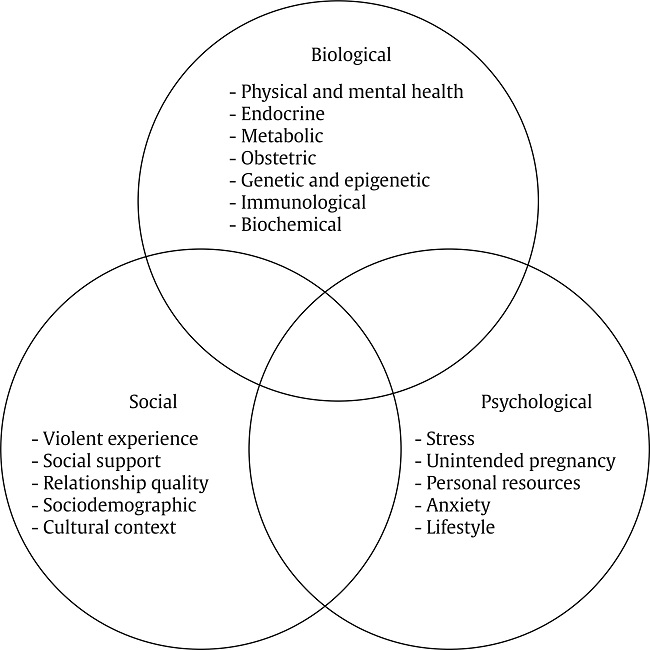
Figure 1. The Biopsychosocial Model of Peripartum Depression, Based on Engel's (1977) Conceptual Framework.
Biopsychosocial Integration – Challenges and Perspectives
Even though various underlying mechanisms of PPD have been proposed, the level of evidence is unclear due to the predominant focus on the postpartum period and on a single aspect of the PPD risk, either biological or psychosocial dimension, and represented by a narrow set of risk indicators. Moreover, varying research designs, small observed effects, and extensive methodological differences among studies limit conclusions. Nevertheless, interdisciplinary studies of a biopsychosocial nature hold promise to uncover the pathogenesis of PPD. However, they are lacking due to a multitude of barriers to implementing high-quality integrative studies. Typically they are more challenging to conduct than discipline-specific research (Yim et al., 2015) and require more resources (e.g., financial, logistical, and time demands). Moreover, it is more strenuous to bridge various disciplines due to different methodological obstacles, such as defining the timing of measurements, inclusion and exclusion criteria, relevant covariates, sampling methods, and statistical analyses while ensuring adequate statistical power.
Biopsychosocial research usually has more homogeneous and smaller samples, possibly due to higher costs and invasive data collection (Yim et al., 2015). Also, integrative models are rare, often burdened by convenient, under-representative samples (Kuhlman et al., 2019) or a lack of control (Yu et al., 2021). Next, recruitment and study participation is more difficult as participants might be less inclined toward research that includes biological sampling, particularly if involving invasive methods (e.g., blood draws or tissue sampling). Consequently, participation in biological studies might require transportation of the participant to the research site or a laboratory to donate the sample, which might be challenging for pregnant women, mothers with small children, or even marginalised populations, which are especially underrepresented among studies.
Furthermore, the timing of measurements has been a topic of debate in PPD research, as considerable differences in the influence of genetic factors depend upon the exact time of measurement in the peripartum period (Guintivano et al., 2018). For example, some postulate that due to major biological changes, early pregnancy and early postpartum are periods when the relationship between biological factors and PPD is more likely to be detected (Yim et al., 2015). In contrast, some genetic and epigenetic studies show positive associations only for PPD in late pregnancy and early postpartum and null findings for measures taken in early pregnancy (Figueiredo et al., 2015).
However, to ensure empirical progress and discoveries, scientists should aim to overcome the barriers to multidisciplinarity. Peripartum mental health researchers should broaden their network with researchers from other disciplines and countries and promote data-sharing and pooling on a larger scale. To maximise sampling, some studies on pregnant women are exploring self-sampling techniques (Curran & Alderdice, 2016), which might be a promising way of collecting biological measurements on the perinatal population. Recruitment and retention in studies can also be supported by dispensing vouchers or reimbursements for participants' transportation costs to the study site, providing on-site childcare or child educational programs for mothers with children, or even using mobile laboratories (Kuhlman et al., 2019). Ultimately, by working on removing the barriers to multidisciplinary research, progress toward essential discoveries and a higher-level science can be achieved.
Biopsychosocial Framework in Clinical Practice
Evidence suggests that the biopsychosocial paradigm should be applied in clinical settings, as well. Based on the findings of biopsychosocial-originated research, it seems integral to establish close multidisciplinary cooperation in perinatal clinical settings. The recommendation for clinical practice is to follow a holistic and individualised, person-centred approach, taking into account the most recent scientific discoveries in the field as part of evidence-based medical practice. Theoretical lenses through which clinicians view PPD have important ramifications on the treatment and management (Beck, 2002). Therefore, healthcare providers should be familiarised with theoretical models that best describe PPD alongside the most salient risk factors for PPD. As PPD is often overlooked and underdiagnosed (Geier et al., 2015), routine screening for mental health issues and accessible psychological support should become part of the standard perinatal care. When assessing PPD and tailoring treatment, a broad range of biological, psychological, and cultural contexts should be carefully considered. Healthcare providers should aim to acknowledge and validate women's needs, experiences, and expectations in the perinatal period, especially when addressing sensitive topics such as suicidality (Bright et al., 2022). Providing a safe and caring environment for pregnant and postpartum women could minimise the stigma and contribute to a quality dialogue with women during the sensitive perinatal period. Moreover, optimal PPD management can be formed through an evidence-based, biopsychosocial approach tailored to the specific needs of every woman. Besides accessible psychological support, steps should be taken towards psychoeducational programs targeted at women and their partners to improve mental health literacy, foster social support, and reduce the stigma surrounding help-seeking for perinatal mental health issues.
Directions for Future Studies
Translating well-characterised biopsychosocial models requires the generalizability of knowledge (Kuhlman et al., 2019). However, studies in the area are of low to moderate quality and with considerable heterogeneity in methodology, which lowers the reliability of the conclusions, as highlighted by recent umbrella reviews (Gastaldon et al., 2022; Hutchens & Kearney, 2020). A particularly high methodological discrepancy among the biology-originated studies (e.g., small, highly selected samples, underpowered studies, and different target tissues, statistical procedures, research designs, the timing of measurements, or exclusion criteria) prevents closer comparisons. Future studies should address these issues, adopt a more rigorous methodology, enhance the sample representativeness, and employ open science practices, as it becomes evident that a certain level of unity within research designs is paramount. For example, genetic studies should approach genetic variation by accounting for population differences deriving from genetic ancestry (e.g., European, African), which is often not the case (Guintivano et al., 2018). Also, adopting a multi-systems approach, and sharing methodology and data, especially in novel fields like epigenetics, could facilitate cross-study comparisons and maximise dataset utility (Braun et al., 2019).
Biopsychosocial models should be further tested and refined, fostering innovative translational research that bridges diverse areas of expertise and guides perinatal mental health care. Given that the timing of assessment (e.g., early vs. late postpartum) is important for delineating the relationship between genetic vulnerability factors and environmental context for PPD (Figueiredo et al., 2015; Gastaldon et al., 2022), prospective studies should be thoughtfully designed to capture and identify the optimal time window for investigating PPD. Identifying key biological and psychosocial predictors, trajectories, interrelations, and most vulnerable periods when factors most exacerbate PPD risk is an essential next step. As numerous sub-categories of biological, psychological, and social risk dimensions are identified, a wider range of risk indicators ought to be investigated simultaneously. Moreover, a prospective examination of more specific topics is warranted, such as causal mechanisms and outcomes among various PPD subtypes or PPD in women with physiological or medical characteristics that share similar biological underpinnings with PPD (e.g., premenstrual syndrome, gestational diabetes). Genetic, epigenetic, and immunological factors implicated in PPD pathogenesis warrant robust and detailed inspection, with gene x environment interaction models yet to be empirically established. Furthermore, studies combining multi-omics technologies are expected to become a major direction for future PPD research (Yu et al., 2021).
Even though the literature on psychological underpinnings is extensive, delineating the type of stressors or life events related to the greatest vulnerability to PPD and the mechanisms through which stress effects are moderated is warranted (Yim et al., 2015). Similarly, due to the predominant focus on PPD on a symptom level and in the postpartum period, studies covering the entire peripartum period using clinical interviews to diagnose PPD might convey different pathophysiological processes. If using screening instruments, a threshold model may be superior for understanding PPD aetiology (Yim et al., 2015). Additionally, considering the current global health and economic situation and the war-related burden, socioculturally sensitive studies are urgently needed. Specific, culturally- and contextually-relevant stressors conceptualised within the “biopsychosocial conceptual model of PPD risk” by Lara-Cinisomo et al. (2016) call for a detailed investigation among other marginalised or disadvantaged groups of women. In general, research should be alert to larger-scale societal changes and flexible enough to incorporate them into study designs and tested models.
Stakeholders' perspectives on peripartum biopsychosocial research warrant examination through qualitative designs or community-based participatory research (CBPR) to bridge the gap between the desired study design and feasibility from the participants' perspectives. CBPR develops strategies for research procedures in collaboration with stakeholders, and its key strength is the researcher-participant partnership combining researchers' scientific expertise with participants' real-world knowledge (Cargo & Mercer, 2008). CBPR studies could be particularly useful for sensitive and complex topics, such as PPD.
Given the complexity of PPD, more scrutinous methodological models testing possible non-linear relationships in larger cohorts and advanced multivariate techniques, like structural equation modelling or survival models, should be utilized across the entire peripartum period. Recent technological advances have led to the development of novel, relatively accurate machine-learning models for predicting PPD that advance early identification of women at-risk (Andersson et al., 2021; Zhang et al., 2021). Machine learning models and other innovative prediction algorithms require further testing and could serve as fruitful avenues for future PPD research. Considering the current state of the science on PPD, prospective, larger-scale biopsychosocial research is of exceptional scientific and clinical relevance and imperative for a more comprehensive understanding of PPD. Integrative studies should be prioritised for the benefit of better theory formation, improved prediction accuracy and timely action in managing PPD, ultimately moving towards reducing the personal and global burden of this debilitating disorder.
Conclusion
Given the high prevalence and severity of PPD, developing a theoretical model that most accurately and comprehensively explains PPD is essential to accelerate discoveries and foster quality perinatal mental health care. Empirical evidence strongly points to the heterogeneous nature of PPD and complex underlying aetiological processes. Biological predispositions are inseparable from psychological and social contexts, altogether shaping individual PPD risk. Nevertheless, PPD has often been investigated unilaterally, focusing on biological or psychosocial aspects separately. Responding to these shortcomings, several biopsychosocial models of PPD emerged, theorising on depression during pregnancy, postpartum or the entire peripartum period. The models have evolved and expanded over time, although limitations exist, such as a diverse conceptualisation of PPD aetiology and causal pathways, unequal representation of risk factor dimensions, and a lack of empirical support for the proposed models. Although warranting further evaluation and adjustments, integrative models provide a valuable framework for investigating PPD.
Research designs and clinical practice guided by a biopsychosocial theory and multidisciplinary cooperation are integral for a comprehensive understanding of PPD aetiology. Translational research following open science practices and a person-centred clinical approach should be prioritised in perinatal settings. Special effort should be put into overcoming the barriers to integrative research of PPD to progress towards essential discoveries and a higher-level science. Biopsychosocial principles should be applied throughout the perinatal research and healthcare provision as a necessary landmark towards guiding future theory, improving maternal mental health care, and ensuring better outcomes for mothers and children.














