Introduction
Pharmaceutical Care (PhC) for outpatients in the Pharmacy Departments of Spanish hospitals has increased since 1992, after a change in regulations that requires that certain medications (“hospital diagnosis-HD” or “hospital use-H”) should be dispensed at hospital1. This care activity justified opening general pharmaceutical care hospital outpatient clinics, managed by Pharmacists specialized in Hospital Pharmacy. In the majority of hospitals, one or more Pharmacists will be in full-time charge of seeing patients with different conditions such as arthropathy, cardiopathy, renal impairment, leukemia, multiple sclerosis, etc.
A good-quality PhC for outpatients, providing added value and promoting health outcomes, must be focused on patients, manage their chronicity, be orientated by healthcare processes, guarantee continuity of care, and be supported by those criteria established by the scientific societies of reference2-9. Therefore, it is desirable that outpatients are seen in hospital outpatient clinics by pharmacists extremely specialized in specific conditions and treatment areas, integrated and coordinated with the healthcare team, and who will promote continuity of care within and outside hospital. This pharmaceutical care model focused on patients with certain conditions, and in collaboration with the rest of the healthcare team, has already demonstrated very good clinical, economic and humanistic outcomes in studies with maximum scientific evidence, both in Primary Care (PC) and Specialized Care10-19, but there has been limited assessment from the perspective of outpatient clinics at the Pharmacy Department.
Until 2010, the Hospital Pharmacy Department (HPhD) had three general outpatient clinics and 6 specialized outpatient clinics. But based on the above, a strategic and organizational restructuration by processes was conducted, in order to provide continuous PhC under the responsibility of pharmacists with great specialization in clinical or pharmacotherapeutical areas. This strategic change led to strengthening Specialized PhC Hospital Outpatients Clinics (SPhCHOCs) with the objective of improving pharmaceutical care for outpatients, both from the healthcare perspective of the Pharmacy Department and from the patient perspective.
Given that no outcomes have been published so far in this setting, this study has been conducted with the objective of describing the organizational model, assessing the quality of care, and understanding the satisfaction perceived by outpatients with the implementation of SPhCHOCs.
Method
SPhCHOCs are integrated in the HPhD of a High-level hospital of reference with 1,500 beds, for a healthcare area of 550,000 inhabitants; it provides PhC every year to 45,000 hospitalized patients, 2,500 Day Hospital patients, and 9,000 outpatients, which represents 45,000 consultations in total approximately.
The model of care, at pharmaceutical care level, consisted in each pharmacist being responsible for the patients of a specific clinical-therapeutic area, either hospitalized, at Day Hospital or outpatient clinics, spending part of their daily time at work in each setting of care. At patient care level, the model of outpatient care was based on opening SPhCHOCs in charge of each pharmacist, and implementing a series of organizational improvements which are described below.
In the first phase, there was an assessment of the activity foreseen for each SPhCHOC, in order to design the schedule for opening each of the clinics, and the material and human resources required; this was based on historical data about the activity of the overall original outpatient clinics, obtained from the HPhD scorecard, the information system for prescription and dispensing medication to outpatients, and the foreseen time required for each consultation. This allowed to define the number of hours/week and days/week for each SPhCHOC.
The next step was managing with the Hospital Admission Department the coding for each SPhCHOC agenda, pharmacist in charge, opening hours, number of appointments/day, opening days, services offered (type of activity), and opening day. Five basic services were defined: first visit, subsequent visit, teleconsultation, clinical trial, and Recipe visa.
Table 1 shows the coding, opening schedule, main diagnoses of patients, and time of weekly care for each one of them.
Table 1 Description of Specialized Clinics and time spent in patient care.

1: Until April, 2015 (opening date for AFR13), HBV and HCV patients were included. 2: Until July, 2015 (opening date for AFR14), hematological patients were included. MS: Multiple Sclerosis; ALS: amyotrophic lateral sclerosis; IBD: intestinal bowel disease; CF: Cystic Fibrosis; PPH: Primary Pulmonary Hypertension; HCC: hepatocarcinoma; BMT: bone marrow transplant.
Unless there is an urgent need for PhC, patients are seen with a previous appointment, both in first and subsequent visits, and they are entered into the corporate information system Sigha©. Patients confirm their presence in the waiting room by introducing their healthcare card in an “ATM” (Chronos © information system), and the Pharmacist will then call the patient to the consultation room through an acoustic signal and an image on a screen, through the information system. Finally, the pharmacist will enter into Chronos© the patients seen with an appointment as well as no-shows (and the predefined justification for not seeing these).
An automated dispensing system (ADS) called Rowa® was installed for outpatients, and integrated with the electronic prescription system and the HPhD management system, which dispenses the medication/s in the consultation room through a conveyor belt from the automated warehouse, and generates the discount of the dispensed units from the stock. A radio-frequency identification system (RFID) was implemented, which identifies the patient and the medication by the labelling of each package with RFID or DataMatrix and through a label reader, with lot and use-by date, and enters this information into an information system, thus improving the safety of the dispensing act.
PhC was conducted in SPhCHOCs following a standard operating procedure (SOP) including, among other aspects, the basic activities that pharmacists should carry out in the outpatient clinic: prescription validation, analysis of interactions and potential adverse events, information on medication, promotion and assessment of patient adherence, PhC documentation, and coordination with the specialist and the PC Pharmacist. PhC provided in SPhCHOCs by the Pharmacist was documented in the electronic clinical record Ianus®, through “clinical course”. Besides, the HPhD, in collaboration with the Hospital Information Department and the relevant hospital departments, developed monitoring systems (SiMON) for the follow-up of HIV and/or HCV patients in the relevant SPhCHOCs.
A teleconsultation system was established, with or without medication home delivery, as well as a protocol for coordination among hospitals for subsequent visits of stable patients, approved by the Hospital Medical Director, and based in current legislation. Patients must meet the inclusion and exclusion criteria agreed with the clinical team responsible for them, and they must sign an Informed Consent.
On June, 2015, a computer platform of interconsultation (IT) was implemented for bidirectional consultation between PC and Hospital Care (HC) Pharmacists in the healthcare area. This platform channels consultations to the pharmacist responsible, it codifies patients anonymously, features a system of transmission alerts, and standardizes the reason for consultation and its outcome.
The development of SPhCHOCs in charge of highly specialized pharmacists, in parallel with their responsibility in specific clinical-therapeutical areas, required continuous post-specialization training, with the objective of acquiring the specific skills to manage outpatients; among other training activities, there was a promotion of the BPS qualification (Board Pharmacy Specialities), university master’s degrees, and courses on clinical interview.
The assessment of the quality of care of this SPhCHOC model was conducted through a retrospective analysis of healthcare activity in three periods: 2010, 2013 and 2016; this is justified by the fact that these years represent the stage previous to promoting this model, the intermediate stage, and the current stage (based on the percentage of consultations conducted in SPhCHOCs in relation to the total number of consultations conducted). Healthcare activity in terms of number of patients managed, first visits, subsequent visits, and patients in teleconsultations, has been extracted from the information systems described. Three variables of healthcare quality have been assessed: percentage of compliance with previous appointments, waiting time for patients, and percentage of PhC documentation in clinical records. The descriptive statistical analysis shows percentages and mean values with standard deviations; the inference on the parameters of two populations with independent mean values was conducted with Studen’t t test, while Pearson’s Chi Square test was used for the inference on the parameters of two populations with independent percentages, for a 95% confidence level. The Epidat 4.2 statistical program was used.
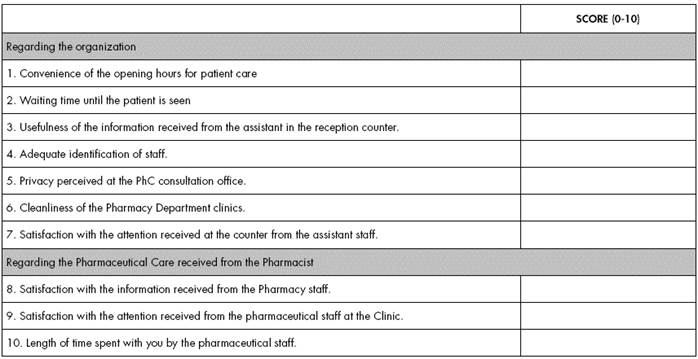
Quality perceived by outpatients in the SPhCHOC was evaluated every year of the study through a satisfaction survey (Figure 1). Through stratified random sampling, the necessary sample size was calculated with 95% certainty, a 30% loss rate, and ±6% accuracy for the entire hospital. A comparison of mean values was conducted for each year, in the variables of organization, pharmaceutical care, and overall satisfaction level of the outpatient during the years of the survey, through Student’s t statistics, with a 95% confidence interval and for equal variances, using descriptive statistics calculation with the Epidat 4.2 computer program.
Results
In total, 15 SPhCHOCs were opened up to 2016, managed by 18 pharmacists working part-time; the number of general OUs for low-prevalence conditions or stable patients referred from SPhCHOCs was reduced to 2. Six consultation rooms guarantee privacy and confidentiality, and there is access to all hospital information systems. The total time of PhC in SPhCHOCs has been increasing based on new openings; in 2016, it was 161 hours/week, which represents approximately 26% of the mean daily time of pharmacists. The number of patients seen in outpatient clinics was 7,750 in 2010, 7,261 in 2013 and 9,690 in 2016, and the number of consultations conducted was 33,641, 32,926 and 45,129 respectively. The proportion of consultations managed at SPhCHOCs in relation with the total number of consultations conducted has increased significantly between these years: 9.4% in 2010, 27.6% in 2013 and 72.7% in 2016 (p<0.0001). Table 2 shows the data updated in 2016 regarding total number of consultations per agenda, time of consultation scheduled for first and subsequent visits, relation between number of subsequent / first visits, proportion of compliance with previous appointments, and mean waiting time from the hour of the appointment. There have been 475 teleconsultations during 2016, by 60 patients in the AFR6 and AFR13 SPhCHOCs (9.6% of the total number of subsequent consultations), and 33 patients have been included in the program for coordination between hospitals (these programs were not active in 2010 and 2013), which represents 85% of candidates. The degree of use of the ADS reaches 75.6% of SPhCHOCs.
Table 2 Consultations per year, time of consultation per service, subsequent / first visits ratio, compliance with previous appointment, and waiting time per SPhCHOC. Year 2016.

Regarding the use of the information systems of the hospital and the HPhD, the PhC documentation provided in the clinical course of the computerized clinical record by the pharmacist in charge was 2.3% in 2010, 3.8% in 2013 and 9.81% in 2016 (p<0.0001). During 2016, 335 patients with 1,433 follow-ups have been included in SiMON-VC; these have generated 1,825 events (637 for efficacy, 886 for safety, and 302 for clinically significant interactions). During the first year of implementation, there were 321 e-consultations in total, 110 referred from SPhCHOCs to PC, mostly due to the need of pharmacotherapeutical monitoring of the patient (65%), incorrect dosing (10%) and treatment compliance (10%).
The rates for compliance with previous appointments were 61.3% in 2010, 78.2% in 2013 and 88.8% in 2016 (p<0.0001). The mean waiting time of patients from the time of appointment to the time they were called to the consultation room was 27.6±12.1 minutes in 2010, 12.7±8.1 minutes in 2013 and 12.1±5.4 minutes in 2016 (p<0.0001).
The specific training for pharmacists responsible for SPhCHOCs has been completed through three BPS (two in Onco-Haematology and one in Hospital Nutrition) and two university master’s degrees (viral conditions). Besides, the continuous training activities by the Pharmacy Department for healthcare professionals have received credits since 2105.
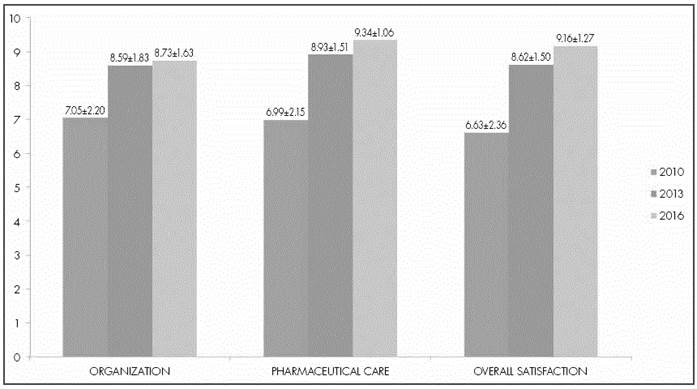
Figure 2 shows the results of quality perceived by outpatients, with statistically significant differences between all the years and variables (p<0.01), except in overall satisfaction between the years 2013 and 2016 (p=0.54).
Discussion
PhC in a specialized Pharmaceutical care hospital outpatient clinics has experienced a major development in recent years in our Pharmacy Department both qualitative and quantitatively, because it requires a significant proportion of pharmaceutical care time, with a high level of implementation in relation with the total number of consultations. PhC for oncological patients, pediatric-obstetrics, HIV, domicile enteral nutrition, and patients with arthropathy / inflammatory bowel disease on biologics treatments, represent almost half of the consultations, and the overall number of consultations conducted in SPhCHOCs already represents three quarters of the total number of consultations.
An essential aspect in SPhCHOC development has been their integration in the hospital information systems from the Admission Department; besides facilitating all the organizational and healthcare management, it has allowed to obtain the indicators for activity and quality of care. Previous appointment has enabled pharmacists to know which patients are scheduled to attend their clinic every day (particularly for first visits), and therefore prepare before the opening hours those PhC activities required for each patient; moreover, this has allowed to identify those patients not attending their previous appointments, arrange a new appointment in order to minimize therapeutic non-compliance, and inform and coordinate with the medical team those measures adequate for each case. According to the results seen, the subsequent implementation of SPhCHOC has led to a significant improvement in this quality of care indicator during the years analyzed. Few studies have assessed this variable applied to PhC in HPhD20,21, and there are no validated quality indicators to measure it; therefore, it is difficult to conduct an assessment of these outcomes by establishing comparisons; however, the results obtained are considered highly satisfactory. Regarding waiting time, it is extremely inferior to the objective of quality proposed since 2012 in the HPhD (25 minutes). In any case, the excellent results obtained in the outpatient survey for 2016 in terms or organization (items 1-7), show a high level of satisfaction with SPhCHOC planning and organization.
SPhCHOC implementation has strengthened significantly PhC documentation; however, this is an aspect with clear room for improvement in the HPhD, because its compliance rate is low. Therefore, it will be a strategic goal in the HPhD for the next years.
Continuity of care and access to pharmacological treatment have been gradually driven from SPhCHOCs, through the implementation of the e-consultation platform 22, teleconsultation, and protocols of coordination between hospitals. A significant number of patients are already benefiting from these programs, which allow providing PhC equal to face-to-face, with the obvious advantages for patients in terms of work and family life conciliation, as well as saving in travelling costs23-26. It is necessary to conduct a specific survey with this group of patients, in order to measure their level of satisfaction.
The results for quality perceived by outpatients in terms of SPhCHOC development are very satisfactory. At organizational level, as well as for pharmaceutical care and overall satisfaction, very high rates are obtained as the percentage of specialized consultations increases; therefore, we consider that the structure and procedures established are very adequate; besides, a relationship of continuous visibility with patients leads to a better perception of PhC in the out-patient clinic.
The main limitation of this study is that there is no assessment of the impact of SPhCHOCs on health outcomes, which is an objective explicitly sought by hospital pharmacists in order to demonstrate the additional value of their patient care activity for different patient groups or on specific conditions27,28. But at the same time this is an opportunity for those pharmacists in charge of each specialized clinic to suggest studies in order to measure the impact of their work on the health of the population managed, through prospective clinical trials.
As future lines, besides research on health outcomes, SPhCHOCs are in a good position to develop the Strategic Map of Pharmacy Care for Outpatients by the SEFH-Mapex29, which intends to determine the setting and actions that will allow pharmacists specialized in Hospital Pharmacy to stay ahead of the needs for these patients, with the ultimate objective of contributing in an effective way to achieving health outcomes and system sustainability. And within this strategic plan, to integrate in PhC the Model for Selection and Pharmaceutical Care for Chronic Patients30, with the objective of identifying those chronic patients that can benefit more from certain PhC interventions, in order to obtain better health outcomes, and establish interventions orientated to the specific characteristics of each patient. Furthermore, the model presented can be used as the basis for the development of the AMO model (Ability, Motivation, Opportunity), recently put forward to contribute value from our professional activity both to patients, according to their needs, and to the healthcare system31.
As a final conclusion, we consider that the development of Specialized Pharmaceutical Care Clinics for Outpatients in a Hospital Pharmacy Department, based on the integration in the hospital information systems, in education and training for pharmacists, their healthcare partnership in multidisciplinary teams, and in the orientation of a continuous pharmaceutical care, leads to an improvement in organizational outcomes, as well as in the quality perceived for outpatients; and that with the strategic lines stated, their contribution must be demonstrated in terms of patient health outcomes, through better quality, safety and efficiency of pharmacotherapy.
Contribution to scientific literature
This paper presents the structure and procedures, analyzes the quality of healthcare, and evaluates the perceived quality of a new organizational model of specialized Pharmaceutical care hospital outpatient clinics in a Hospital Pharmacy Department, focused on patients and continuity of care. This model demonstrates an improvement in health-care quality and the overall satisfaction of outpatients, through care by pharmacists highly specialized in specific conditions and treatments, coordination with the rest of the team, integration in hospital information systems, following standard operating procedures, telepharmacy, automation, and documentation of pharmaceutical care.
The results show the feasibility of performing a reorganization of care that will allow those pharmacists with specific knowledge in a specific treatment area to conduct a continuous pharmaceutical care from hospital admission to the outpatient clinic or day hospital. At research level, this model can be considered the basis for understanding the impact of specialized pharmaceutical care on health outcomes. And at the level of health policy, it raises the possibility of continuous patient care from a pharmacotherapeutical point of view, that should be completed with an adequate follow-up by Primary Care or community pharmacists.











 texto em
texto em