Introduction
Soft tissue sarcoma (STS) tumours arise from the disordered uncontrolled growth of cells that form mesenchymal, connective, or supportive tissue, and occur in the soft parts of the body (i.e. without affecting bone and cartilage) including fat tissue, muscle, tendons, blood vessels, nerves, and deep skin tissue1. Soft tissue carcinoma comprises a large group of neoplasms, with more than 50 different histological subgroups1-3.
The incidence of soft tissue tumours has been estimated at around 300 cases/100,000 population per year, although practically all of the tumours are benign. Around 1% of these tumours are classified as STS because of their malignancy. It is a rare form of cancer, since its estimated incidence in Europe is around 4-5/100,000 population per year. It comprises about 1% of all malignant tumours and is responsible for around 2% of mortality due to cancer.
Soft tissue sarcomas are 20 percent more common in men than in women, and can appear at all ages, even in adolescents and children, where they can account for 21% of diagnosed solid tumours1,2,4-6.
Advanced STS is treated by surgery and chemotherapy. In 1975, Benjamin et al.7 described the use of classic drugs, which remain the most used today. Doxorubicin (i.e. adriamycin)5 and ifosfamide have been first-line treatments for almost 50 years. They can be administered in combination or sequentially: the first-line treatment is doxorubicin; however, if doxorubicin is contraindicated or fails, the second-line treatment is ifosfamide.
Recently, new active chemotherapeutic agents have been added to the list of agents used to treat STS. These new treatments are administered after doxorubicin and ifosfamide if STS becomes resistant and progresses. The new treatments include trabectedin, gemcitabine + dacarbazine or docetaxel, pazopanib, and eribulin8.
Nevertheless, new drug studies are needed to identify new active agents. Participation in clinical trials with new drugs is a valid alternative for patients with STS not amenable to available treatment.
The European Medicines Agency (EMA)9 and the Spanish Agency for Medicines and Medical Devices (Spanish acronym: AEMyPS)10 have authorized olaratumab in combination with doxorubicin for the treatment of adult patients with advanced STS not amenable to surgery or radiotherapy who have not been previously treated with doxorubicin. Olaratumab has been designated as an orphan medicine and has been given conditional approval for its use11.
Olaratumab is a targeted recombinant fully human immunoglobulin G subclass 1 (IgG1) monoclonal antibody that specifically binds platelet-derived growth-factor receptor (PDGFR-α), blocking PDGF AA, -BB, and -CC binding and receiver activation10.
This article provides an economic assessment of olaratumab in the treatment of STS using the MADRE 4.0 program of the GENESIS-SEFH report model12.
Methods
On February 25, 2017, a literature search was conducted of Medline-Pubmed Clinical Queries: (therapy/narrow (filter)) and (olaratumab) and (sarcoma). A single result was obtained: the pivotal clinical trial13 referred to in the European Public Assessment Report (EPAR) published by the EMA9.
For the purposes of the economic assessment, on November 11, 2017, a literature search was conducted of Medline-Pubmed using the descriptors “olaratumab” AND “incremental cost-effectiveness”. An article published in 2017 by Tikhonova et al.14 was obtained.
The data was analysed following the recommendations of the “Guía de Evaluación económica e impacto presupuestario en los informes de evaluación de medicamentos. Guía práctica asociada al programa MADRE 4.0. Noviembre 2016”12 (English translation “Guideline for economic assessment and budgetary impact in medication assessment reports. Practice guideline associated with the MADRE 4.0 program. November 2016”).
Results
Efficacy
The conditional approval of olaratumab was based on a phase Ib/ II clinical trial in patients with STS13. This multicentre open-label superiority study compared olaratumab + doxorubicin (OlaDox) vs doxorubicin alone (Dox) (current reference treatment). The experimental arm received olaratumab 15 mg/kg on day 1 and day 8 of each 21-day cycle plus doxorubicin 75 mg/m2 on day 1 of each cycle for up to 8 cycles. The control arm received doxorubicin 75 mg/m2 on day 1 of each cycle, also for up to 8 cycles.
The gain in progression-free survival (PFS; main variable) in absolute terms was 2.5 months (hazard ratio (HR) 0.672; 95% confidence interval (95%CI) 0.442-1.021). The absolute gain in overall survival (OS; secondary variable) was 11.8 months (HR 0.463; 95%CI 0.301-0.710). Table 1 shows the main efficacy results.
Table 1 Efficacy Results of the Pivotal Clinical Trial13 and the OS, QALY, and Cost-utility Results From Tikhonova et al.14
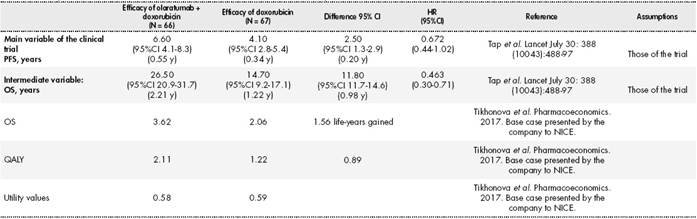
PFS, progression-free survival, defined as the period from the date of randomization to the earliest date of the documented tumour, progression, or all-cause death, whichever comes first. Tumours were assessed using the RECIST 1.1 criteria based on the researcher assessment; OS, overall survival, defined as the period from the date of randomization to the date of all-cause death; QALY, quality-adjusted life years; HR, hazard ratio; 95%CI, 95% confidence interval.
The patients could have received previous lines of treatment for advanced STS, provided they were not doxorubicin, daunorubicin, idarubicin, and other anthracyclines and anthraquinones, or previous therapy with any agent targeting the PDGF/PDGFR-α pathway. This could have compromised the interpretation of the results of the clinical trial because the patients received previous lines of treatment for advanced STS.
Safety
A total of 485 patients received olaratumab in 9 phase I and phase II clinical trials.
In the OlaDox arm, the most common severe adverse drug reactions (ADRs) (grade ≥3) were neutropenia (54.7%) and musculoskeletal pain (7.8%). The most common ADRs of any grade were nausea (73.4%), musculoskeletal pain (64.1%), neutropenia (59.4%), and mucositis (53.1%)9.
Olaratumab has the disadvantage that it has to be administered in chemotherapy unit which is also the case of doxorubicin. Olaratumab can cause infusion reactions in patients and so strict pre-medication monitoring is needed. Specifically, infusion-related reactions (IRR) were reported in 12.5% of patients and mainly manifested as chills, fever, or dyspnea. Severe IRRs, including 1 death, were reported in 3.1% of the patients and mainly manifested as shortness of breath, loss of consciousness, and hypotension. All severe IRRs occurred during or immediately following the first olaratumab administration9.
Economic assessment
An economic assessment was conducted following the recommendations of the “Guía de evaluación económica e impacto presupuestario en los informes de evaluación de medicamentos.. Guía práctica asociada al programa MADRE 4.0. Noviembre 2016”12 (English translation “Guideline for economic assessment and budgetary impact in medication assessment reports. Practice guideline associated with the MADRE 4.0 program. November 2016”).
The economic assessment took into account the following aspects:
Olaratumab was authorized for marketing in Spain on November 1, 2017. Its price was consulted in BOT PLUS15. The deduction described in Royal Decree Law (RDL) 8/201016 was applied as well as 4% VAT. Thus, the economic assessment was conducted using the following prices: The notified list prices of €1,531.15 and €581.84 for 500 mg/50 mL and 190 mg/19 mL vials of olaratumab, respectively. The list price of €14.20 for 50 mg/25 mL doxorubicin.
The cost per cycle was calculated in only 1 case:
With no vial sharing; it being understood that patients cannot be grouped in space and time and therefore any unused portion of the drug left in the vial should be discarded. The results of this analysis were used in subsequent calculations.
The total cost of the treatment was calculated following the same methodology described above, taking into account differences in the mean number of cycles received with OlaDox and Dox alone in the pivotal clinical trial.
The economic assessment was conducted using the mean number of cycles for each drug and group according to the EPAR of the EMA9. The quantities calculated for each item are shown.
Associated direct costs:
Dexrazoxane was used from the fifth cycle of doxorubicin onward to prevent the chronic cumulative cardiotoxicity associated with the use of this anthracycline. Cost of dexrazoxane per vial15: €74.47 List price-deduction RDL 8/2010 (15%) + 4% VAT.
Calculated cost of use of a day hospital: €292.86; cost consulted on the www.esalud.oblikue.com17.
Calculated cost of treatment of drug-induced neutropenia, taking into account that the OlaDox combination and Dox alone caused neutropenia in 59.40% and 35.4% of patients, respectively. Cost of neutropenia treatment: €4,383.16; Cost consulted on the www. esalud.oblikue.com17. Cost of treatment with OlaDox and Dox per group: €2,603.6 and €1,551.63, respectively.
Calculated cost of mucositis treatment; in the treatment arm and control arm 53.10% and 35.40% of patients developed mucositis, respectively. Cost of mucositis treatment: €3,429.05; cost consulted on the www.esalud.oblikue.com17. Cost of treatment with OlaDox and Dox per group: €1,820.83 and €1,213.88, respectively.
The doses were calculated assuming a body surface area (BSA) of 1.7 m2 and a body weight of 70 kg12.
The authors warned that, depending on the decimals considered, these calculations could vary.
OlaDox would cost €81,581.12, which is much higher than the current therapeutic alternative. The incremental cost of OlaDox vs Dox would be €79,974.40 (See Table 2).
Table 2 Treatment Costs of “OlaDox” vs “Dox”

*The deduction described in Royal Decree Law 8/201016 was applied as well as 4% VAT for all medications in the analysis. LP, list price; VAT, value added tax.
A cost-effectiveness analysis was selected because the only available efficacy data was that of the pivotal study. Subsequently, a cost-utility analysis was published, which will be discussed later. A cost minimization analysis was ruled out, because the results of the clinical trial showed that the efficacy of Olaratumab was superior to the comparator.
Cost-effectiveness analysis
Next, we show the cost-effectiveness data using the efficacy data from the pivotal clinical trial13 (Table 1), and the costs of OlaDox and Dox (Table 2).
Two scenarios were considered:
Scenario 1: Calculate incremental cost-effectiveness based on the acquisition costs of the drugs with no vial sharing and with the efficacy data from the pivotal clinical trial. According to the efficacy data of the clinical trial and the difference in costs between treatments, if patients were treated with OlaDox instead of Dox alone, the incremental cost-effectiveness ratio (ICER) would be €28,443.81 per month gained in PFS and €72,560.74 per life-year gained (LYG).
Scenario 2: Calculate incremental cost effectiveness based on the acquisition costs of the drugs with no vial sharing, with all the associated direct costs (day hospital visits, mucositis, neutropenia, and dexrazoxane use), and with the efficacy data of the pivotal clinical trial. According to the efficacy data of the clinical trial and the difference in costs between treatments, if patients were treated with OlaDox instead of Dox alone, the ICER would be €30,879.79 per month gained in PFS and €78,774.99 per LYG.
Published cost-utility analysis
Recently, Tikhonova et al. (2017)14 published a critical review conducted by the Evidence Review Group (ERG) of the evidence submitted by the pharmaceutical manufacturer Eli Lilly & Company Limited to the National Institute for Health and Care Excellence (NICE), which had invited the company to deliver a review of the evidence and a cost-effectiveness analysis of olaratumab plus doxorubicin for the treatment of STS not amenable to surgery or radiotherapy. The company assessed the clinical and cost effectiveness of OlaDox vs Dox alone and ifosfamide plus doxorubicin (IfoDox). Given that IfoDox is rarely used to treat STS in the United Kingdom, the NICE Appraisal Committee concluded that the most relevant comparator for OlaDox was doxorubicin alone, discarding IfoDox as a comparator in the final assessment.
According to the final documentation provided by the company, olaratumab could be considered as an alternative to doxorubicin, which has been used as first-line treatment for advanced STS for more than 3 decades.
The company argued that since the maximum cumulative lifetime dose of doxorubicin allowed in UK clinical practice is 450 mg/m2 (equal to 6 treatment cycles at a dose of 75 mg/m2), patients who have already received doxorubicin as first-line treatment would not be able to receive OlaDox in subsequent treatment lines.
The following aspects were taken into account in this cost-utility analysis:
Total costs were expressed in pounds sterling (2015).
Total costs included the costs of drug acquisition and administration, disease management, the costs of treating adverse events, and cardiac monitoring costs. Colony-stimulating factors were administered according to the weight of the patient, whereas other drugs were administered according to the BSA. The company assumed a mean weight of 77.3 kg and a BSA of 1.91 m2.
In the UK, an accumulated dose of anthracycline of more than 450 mg/m2 is not administered in clinical practice because of the potential risk of cardiotoxicity. Thus, the company presented a UK practice scenario analysis of a maximum of 6 cycles instead of 8 cycles of OlaDox.
The company assumed that 2 types of vials of olaratumab were available: 500 mg and 190 mg. No vial sharing was assumed.
The costing of drug administration was based on the assumption that OlaDox administration (with premedication for both drugs) can take up to 2 hours, and administration of Dox (including premedication) can take up to 60 minutes.
In the pivotal trial13, patients with advanced STS received up to 4 lines of systemic cancer therapy after the experimental treatments under study. In the base case, the company assumed that the total cost of treatment in disease progression was independent of post-progression survival; that is, the cost of post-progression treatment was the same in both treatment arms.
In the base case analysis, the cost of treating adverse events equal to or higher than grade 3 was calculated by combining the proportion of events likely to require hospitalization according to the pivotal trial data13 and the estimated costs per event obtained from the UK National Health Service (NHS) reference costs. The costs of managing adverse events were accounted for in the first year of the model presented.
Regarding utilities, the pivotal trial13 did not collect or analyse any quality of life data, so the company conducted a literature review to identify published health-state utility estimates. The utility values of 0.72 and 0.56 were taken from Reichardt et al.18.
Table 3 summarizes the cost-utility analysis presented by the company to the NICE.
Table 3 Cost-utility Analysis Presented by Eli Lilly & Company Limited and Reviewed by the ERG of the NICE

Exchange rate used in the table. 1 Pound = €1.126 (November 2017). LYG, life-years gained; QALY, quality-adjusted life years; OS, overall survival; PFS, progression-free survival; ERG, European Regulatory Group; NICE, National Institute for Health and Care Excellence.
Cost-utility analysis (own work)
We conducted our own cost-utility analysis using the data on quality-adjusted life years (QALYs) obtained with treatment with OlaDox vs Dox (Tikhonova et al.14) and their difference in costs according to the list price in Spain. Thus, if patients were treated with OlaDox instead of Dox, each additional QALY gained per patient would cost €86,449.59/QALY (Table 4).
Table 4 Own Cost-utility Analysis Using QALY Data From Tikhonova et al. (2017)14 and the Incremental Cost Obtained in the Present Study

QALY, quality-adjusted life years; A, OlaDox scenario; B, Dox scenario; ICER, incremental cost-efficiency ratio; PFS, progression-free survival; OS, overall survival.
If we use the QALYs calculated with the median PFS, OS, and the utility values of 0.72 for PFS and 0.56 for OS reported by Reichardt et al.18, each additional QALY would cost €132,198.11/QALY.
Sensitivity analysis
Four sensitivity analyses were conducted based on the following aspects (Table 5):
Table 5 Incremental Cost-Effectiveness Ratio. Sensitivity analysis with assumptions other than base conditions of use
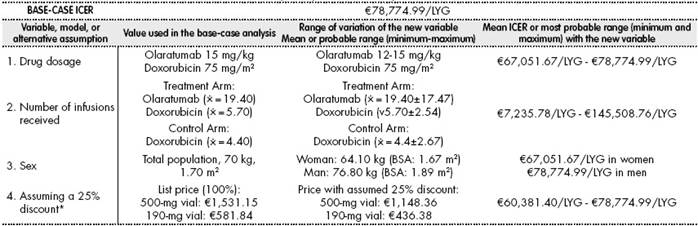
*The deduction described in Royal Decree Law 8/201016 was applied as well as 4% VAT for all medications in the analysis. In all cases, we maintained the assumption of no vial sharing, as in the base case. ⨰: arithmetic mean; BSA, body surface area; LYG, life-years gained; ICER, incremental-cost effectiveness ratio.
ANALYSIS 1: We decided to perform a sensitivity analysis, because olaratumab can cause grade 3 adverse reactions at the gastrointestinal and musculoskeletal level, in addition to those that originate at the haematological level, and in these cases the dose of olaratumab should be discontinued until toxicity is less than or equal to grade 1 or has returned to baseline level prior to treatment. In subsequent infusions, the dose should be reduced to 12 mg/kg in the case of severe (grade 3) toxicities. Therefore, we conducted a sensitivity analysis with doses of 12 mg/kg olaratumab. We did not include a dose reduction in the case of doxorubicin. The maximum ICER was estimated taking into account the costs of neutropenia, mucositis, and so on. The ICER was estimated to be between €67,051.67/LYG and €78,774.99/ LYG (base-case ICER).
ANALYSIS 2: Given that the number of olaratumab cycles received can vary between 1 and 83, we decided to perform another analysis based on the mean and standard deviation of olaratumab infusions received ( = 19.4
± 17.47) and doxorubicin infusions received ( = 5.7 ± 2.54), assuming a maximum of 8 infusions. The analysis was conducted using the lower and upper limits of the doxorubicin and olaratumab infusions received and the consequent use of the day hospital. To obtain and compare the ICER, the same procedure was performed for the doxorubicin infusions in the control arm ( = 4.4 ± 2.67). Because there were insufficient doxorubicin cycles, the cost of dexrazoxan at the lower limits was discarded. The remaining variables remained constant. In this case, and given the wide variation in the number of infusions, the ICER varied between €7,235.78/LYG and €145,508.76/LYG.
ANALYSIS 3: Given that the dose of olaratumab is calculated by weight, the ICER is expected to differ between men and women, because, according to the Spanish Institute of Statistics (Spanish acronym: INE)19, the average weights of Spanish women and men are 64.1 kg (BSA = 1.675 m2) and 76.8 kg (BSA = 1.89 m2), respectively. Given these considerations, and with all other variables held constant, including efficacy (HR = 0.55 in men and 0.53 women), the ICER ranged between €67,051.67/LYG in women and € 78,774.99/LYG (base-case ICER) in men, thus coinciding with the results of Analysis 1. This difference is relevant because 60% of patients with STS are men.
ANALYSIS 4: Given that the list price and actual price of the vials can differ, we assumed a random discount of 25% on the list price (only for vials of olaratumab). In this case, the ICER would range between €60,381.4/ LYG and €78,774.99/LYG (base-case ICER).
No particular subgroups were identified in which the treatment could have led to statistically significant results, and therefore no sensitivity analyses by subgroup were performed.
Estimated budgetary impact and estimated health benefits
According to the INE19, as of January 1, 2017, the Spanish population was 46,528,966 and the Spanish population equal to or more than 18 years was 38,400,583. We estimate that in Spain there would be 1,800 patients with metastatic STS per year. If we take into account restrictions of age, morbidity, and indication (i.e. mainly cardiac toxicity caused by doxorubicin), there would be between 800 and 1,200 candidates per year for the administration of olaratumab. If we assume an incidence of 8 cases of STS per 100,000 population per year, metastasis would occur in 20% of cases and there would be a risk of recurrence in 35% of cases20.
Given the average of treatment cycles received (9.7), we only considered treatment of limited duration (<1 year).
Estimation of the target population in treatments of limited duration (Table 6)
Table 6 Estimation of the target population amenable to treatment. Data obtained from the SEOM Olaratumab report20

Observations: All data on the target population referred to was extracted from the SEOM Olaratumab assessment report20. References: Informe de Evaluación SEOM de Olaratumab (Lartruvo®) en combinación con doxorubicina en sarcomas de partes blandas avanzados del adulto. (Consulta Enero 2017).20 (English translation: “SEOM Assessment Report of Olaratumab (Lartruvo®) in combination with doxorubicin in advanced adult soft tissue sarcomas (accessed January 2017). SEOM: Spanish Society of Medical Oncology.
In Spain, the annual target population of patients with metastatic STS who are candidates for treatment with olaratumab as first-line treatment under the established conditions of use is estimated to be between 800 and 1,200 patients.
We have no reason to expect that there will be changes in the natural evolution of the disease or greater variations in the incidence and prevalence of the disease.
Sensitivity analyses were conducted in which the 2 main aspects for assessment would be the different acquisition costs of the drug and variations in the size of the target population according to alternative plausible scenarios.
Sensitivity analysis based on the acquisition costs of the assessed drug
SCENARIO 1. The incremental cost per patient would be €79,974.40 according to the price consulted on the BOT- PLUS website15. The discount of RD 8/201016 and 4% VAT were applied. The list prices of €1,531.15 and €581.84 of 500 mg/50 mL and 190 mg/19 mL vials olaratumab, respectively.
SCENARIO 2. If we have an available €21,000/QALY, the cost of a 500-mg vial olaratumab should be €314.87 and a 190-mg vial should be €121.45 if OS is taken into account.
SCENARIO 3. If we have an available €30,000/QALY, the cost of a 500-mg vial olaratumab should be €506.54 and a 190-mg vial should be €195.37 if OS taken into account.
As mentioned, the estimated size of the target population in Spain would be between 800 and 1,200 patients. Therefore, the national economic impact would be between €61,759,592 and €92,639,388, entailing between 166.66 and 250 years of PFS gained, between 784 and 1,176 years of OS gained, and between 714.4 and 1,071.6 QALYs gained (QALY data obtained from Tikhonova et al. 201714).
In 2016, Andalusia (an autonomous region of Spain) had a population of around 6,766,814 inhabitants older than 18 years. If the data from Spain is extrapolated to Andalusia, in this region there would be between 141 and 212 new cases per year of STS amenable to olaratumab treatment. The economic impact at the regional level would be between €10,885,136 and €16,366,291, entailing between 29.38 and 44.16 years of PFS gained, between 138.18 and 207.76 years of OS gained, and between 125.91 and 189.32 QALYs gained (QALY data obtained from Tikhonova et al. 201714).
Thus, this drug would be placed in the quadrant of medicines with an ICER clearly above the threshold and with a high budgetary impact.
Assuming the list price and a theoretical €21,000/QALY and €30,000/ QALY, the analysis showed that the ICER and the estimated budgetary impact are well above optimal values.
Although Tap et al. (2016)13 found that olaratumab with doxorubicin was more effective than doxorubicin alone, no subgroup was identified. Thus, we can only recommend a significant reduction in the list price of up to €314.87 per 500-mg vial and of €121.45 per 190-mg vial.
If we consider the threshold of €21,000/QALY, the cost of a 500-mg vial olaratumab should be €314.87 per 500-mg vial and €121.45 per 190-mg vial, if OS is taken into account. The total incremental cost per 0.98 years gained would be €20,580. Using these criteria, and assuming between 800 and 1,200 patients, the national economic impact would be between €16,464,000 and €24,696,000.
If we consider the €30,000/QALY threshold, the cost of a 500-mg olaratumab vial should be €506.54 and the price of a 190 mg/19 mL vial should be €195.37, if OS is taken into account. The total incremental cost for 0.98 years gained would be €29,400. Using these criteria, and assuming between 800 and 1,200 patients, the national economic impact would be between €23,520,000 and €35,280,000.
If we consider the threshold of €11,000/QALY, the cost of a 500-mg vial olaratumab should be €101.91 and the price of a 190 mg/19 mL vial should be €39.31, if OS is taken into account. The total incremental cost for 0.98 years gained would be €10,780. Using these criteria, and assuming between 800 and 1200 patients, the national economic impact would be between €8,624,000 and €12,936,000.
Discussion
The number of doxorubicin cycles received could be a point of contention regarding a clinical trial in a hospital, since in experimental and control arms doxorubicin is administered for a maximum of 8 cycles at 75 mg/m2 (total cumulative dose of 600 mg/m2). Because of the toxicity of anthracyclines, this dose is not commonly reached in routine clinical practice, and in general the cumulative dose received is limited to between 450 and 500 mg/m2 with a median of 4 cycles21,22. Thus, the use of dexrazoxane as a cardioprotective agent against anthracycline cardiotoxicity in settings of between 5 and 8 cycles would also lead to a relevant increase in the total cost of treatment.
Furthermore, patients could have received previous lines for their advanced disease provided they were not doxorubicin, daunorubicin, idarubicin, or other anthracyclines and anthraquinones, or previous therapy with any agent targeting the PDGF/PDGFR-α pathway. This could have compromised the interpretation of the results of the clinical trial because the patients received previous lines of treatment for advanced STS.
Moreover, in the pivotal trial, patients with an Eastern Cooperative Oncology Group (ECOG) performance status score of more than 2 were not included, and only 27.3% (n = 18) of the patients in the treatment group were more than 65 years, which casts doubt on the results of the OlaDox combination in these patients9.
The disparity between the gain in PFS (2.5 months) and the gain in OS (11.8 months) is striking. This disparity cannot be explained by the natural course of the disease and is a point of debate in some opinion articles23. They suggest that olaratumab may have an immunological effect because its response is reminiscent of that of certain antibodies used in immunotherapy, such as ipilimumab in melanoma. This possibility should be investigated in future phase III studies.
The higher OS rate obtained in the experimental arm was associated with a modest delay in tumour progression. No difference was observed between patients with positive or negative PDGFR-α expression, so the correlation between this receptor and improvements or otherwise in OS cannot be explained. An explanation remains pending of the biological basis of the disease and the good results obtained in OS, although it should be noted that the experimental arm were switched to olaratumab monotherapy and that the control arm were switched to olaratumab monotherapy after progression. The number of patients who received olaratumab monotherapy in both arms was very small (approximately 30 in each treatment arm)9.
The METASURV24 calculator was used to calculate the probability of interaction between each subgroup described in the pivotal trial. It was found that no subgroup would benefit from the treatment. Given that the therapeutic target of olaratumab is PDGFR-α, it is striking that its expression was not relevant to treatment efficacy, especially as the HR was lower (although without reaching statistical significance) in the group that did not express the target. To date, no predictive biomarker is available. Protein expression with the proven PDGFR-α antibody was not predictive of metastasis or survival in patients treated with olaratumab.
In November 2017, the Therapeutic Positioning Report for olaratumab25 was published on the website of the Spanish Agency for Medicines and Health Products, which provided the following conclusion: Olaratumab plus doxorubicin followed by maintenance therapy with olaratumab is recommended vs doxorubicin alone in patients with advanced STS not amenable to treatment with surgery or radiotherapy and who have not been previously treated with anthracyclines as first-and successive line therapy according to the preliminary results of the Tap WD et al.13. Finally, this drug was authorized on the basis of the high clinical relevance of the results, although approval is conditional on the final results of the ongoing phase III trial.
In view of the efficacy and safety results of the phase Ib/II trial and the necessity for and cost of the economic analyses, the authors of the report concluded that olaratumab provides significant benefit to OS, although not to PFS.
However, its usefulness as first-line treatment remains unclear, given that patients could have received previous lines for their advanced disease provided they were not doxorubicin, daunorubicin, idarubicin, and other anthracyclines and anthraquinones, or previous therapy with any agent targeting the PDGF/PDGFR-α pathway. There are very little data available on patients more than 65 years and with an ECOG score ≥2.
To be cost-effective in the setting of STS, the acquisition cost of a 500-mg vial and a 190-mg vial should be between €101.91 and €506.54 and between €39.31 and €195.37, respectively. In addition, when data from the phase III clinical trial become available, the drug will have to be reassessed and repositioned.
Contribution to the scientific literature
This article provides the results of a pharmacoeconomic analysis of olaratumab for the treatment of STS and an updated position statement on the drug based on efficacy, safety, and efficiency criteria, with the aim of assisting decision makers on hospital pharmaceutical and therapeutic committees at the national and regional level. It also provided a justified budgetary impact analysis and the estimated cost of the treatment according to the reference thresholds. This article is the first GENESIS-SEFH report to use the most recent update of the economic section of the MADRE 4.0 program12, which may be of assistance in the preparation of future reports on other therapies.











 text in
text in 


