Introduction
Sepsis is one of the main causes of mortality in intensive care units (ICU) and affects 19 million patients worldwide1. To reduce mortality and morbidity2 due to sepsis, the rapid and early start of suitable antibiotic therapy within the first hour of a diagnosis of sepsis or septic shock is crucial. However, the best therapeutic approach for each patient is determined by his or her particular pathophysiology3.
The class of antibiotics most commonly used in ICUs are β-lactams (BLAs), which include penicillins, cephalosporins, and carbapenems. BLAs are particularly used to combat gram-negative infections. The Spanish National Study of the Surveillance of Nosocomial Infections in Intensive Care Medicine (ENVIN-HELICS) recently published its results on the development of nosocomial infections in 205 Spanish ICUs. This report confirmed the prevalence of gram-negative bacteria (GNB) and found that Escherichia coli (13%), Pseudomonas aeruginosa (13%), and Klebsiella pneumoniae (11%) were the most frequent GNBs in ICUs4.
BLAs are time-dependent antibiotics5 and their pharmacokinetic/pharmacodynamic (PK/PD) index for bactericidal efficiency is determined by the dosing interval percentage at which the free drug concentration (fCss) is kept above the minimum inhibitory concentration (MIC) of the microorganism or suspected microorganism causing the infection (%fT> MIC)6.
However, controversy remains on the optimal dosing interval percentage and how high the fCss should be above the MIC (i.e. fCss/MIC ratio)3. Initially, the % f T> MIC was established at 50% for penicillins and 40% for carbapenemics3. However, it has been argued that the target PK/PD index should be stricter in critical patients, and therefore, the fCss should be higher than the MIC over the entire (i.e. 100%) dosing interval. Other authors have proposed that the fCss should be up to four times higher than the MIC during the entire administration interval (100% f T≥ 4 x MIC), thus ensuring bactericidal activity and minimizing the emergence of antibiotic resistance7,8.
Although intermittent infusion (IIn) is the most widely used antibiotic administration method, its use could make it more difficult to attain the target PK/PD index9. Intermittent infusion necessarily entails plasma concentration fluctuations, which may lead to insufficient concentrations10. This risk is higher in critically ill patients, who normally have PK alterations (i.e. patients with increased renal function may have increased volume of distribution and drug clearance) and are at an increased risk of infection by microorganisms with high MICs11. Previous studies have proposed that continuous infusion (CI) may be a better alternative to IIn, because CI may ensure steady state concentrations (Css) above the MIC for longer periods, thus providing better clinical outcomes12 13-14.
This proposal supports the hypothesis that CI would keep the fCss above the MIC as well as constant over the entire dosing interval, thus achieving improved clinical benefit.
The main study aim was to determine the percentage of critical patients who would reach 100% fT≥ 4 MIC during CI with either piperacillin/ tazobactam (PTZ) or meropenem (MER). The secondary aims were as follows: 1) to determine the percentage of patients who would reach the less demanding PK/PD target of 100% fT≥ MIC; and 2) to assess possible differences in the PK/PD index reached in relation to renal function by group.
Methods
Design
A prospective PK study in adult patients admitted to the ICU of a tertiary hospital. The patients underwent empirical or targeted antibiotic treatment with BLAs due to suspected gram-negative infection. The BLAs under study were PTZ, MER, aztreonam, cefepime, and ceftazidime. This article only addresses PTZ and MER because these drugs were being used in more patients at the time of the interim analysis. The study is currently ongoing (i.e. in the recruitment, processing, and sample analysis phases). However, we present the preliminary results for the first 2 years (June 2015-May 2017).
The study protocol was approved by the local Ethics Committee in accordance with the Declaration of Helsinki. Informed consent was requested from patients or family members before inclusion in the study.
Study population
Inclusion criteria: i) patients admitted to the ICU; ii) treated with BLAs or able to receive them; iii) equal to or more than 18 years of age; and iv) preserved renal function defined as a glomerular filtration rate (GFR) ≥ 60 mL/min/1.73 m2 as estimated using the CKD-EPI equation15. Pregnant patients were excluded.
Data collection
Demographic, clinical, and analytical data were obtained from the electronic registry of the hospital. We also collected pharmacological data on the antibiotic administered, dose, dosage, infusion time, and sampling time.
Dose and drug administration
Standard doses of antibiotics were administered by CI. The patients received a loading dose followed by the total daily dose by CI; those already treated by IIn for more than 24 hours could be changed to CI without the need of a loading dose, because Css had already been reached. PTZ infusions were changed every 24 hours (concentration: 80 mg/mL in 0.9% saline; stability: 24 hours at 25 °C)16; and MER infusions were changed every 12 hours (concentration: 22 mg/mL in 0.9% saline; stability: 17 hours at 25 °C)16. The protocolized maximum dose was 12 g/1.5 g/d for PIP/ tazobactam and 6 g/d for MER.
Determination of plasma concentrations
Blood samples (5 mL) were taken 30 minutes after the loading dose or after at least four doses antibiotic IIn or 24 hours after starting CI (i.e. once the Css was reached). Total BLA concentrations were measured using a previously developed and validated UHPLC-MS/MS procedure17. This procedure involved the precipitation of sample proteins with acetonitrile and subsequent dilution with water. The eluates obtained were then introduced into a C18 reverse phase column using a water/ acetonitrile gradient with formic acid. Finally, BLAs were detected using a triple quadrupole mass spectrometer set up for electrospray in positive ion (ESI+) mode and multiple reaction monitoring (MRM) mode. Retention times were 1.08 minutes for MER and 1.91 minutes for PIP. Processing time per sample was 3.5 minutes. The limits of quantification were 0.58 mg/L and 0.54 mg/L for PIP and MER, respectively. The coefficients of variation and relative bias absolute values were less than 13.3% and 14.7%, respectively.
The target PK/PD index
The PK/PD index was calculated using the f Css/MIC ratio. The magnitude of the PK/PD index was the differentiating factor between the primary (100% fT≥ 4 x MIC ) and secondary (100% fT≥ MIC) objectives. Only Css were analysed. We assumed 30% plasma protein binding for PIP18 and 2% for MER18.
Based on the European Committee on Antimicrobial Susceptibility Testing (EUCAST)19, theoretical MIC values were used for the least sensitive bacteria: Pseudomonas aeruginosa (2 mg/L for MER and 16 mg/L for PTZ); and enterobacteriaceae (2 mg/L for MER and 8 mg/L for PTZ). We conducted a subanalysis of patients with microbiological isolation using the Epsilometer test with actual MIC values.
Statistical analysis
An anonymized database was used. The statistical analysis was performed using the SPSS v.22.0 software package (SPSS Inc., Chicago, IL). The data and results are expressed as median (IQR), continuous variables are expressed as means (SD), and categorical variables are expressed as rates and percentages. The chi-square test was used to analyse differences between GFR groups in reaching the target PK/ PD index.
Results
Demographic and clinical data
A total of 77 patients were recruited. Sixteen patients were excluded due to nonadherence to the protocol: 12, due to missing samples to determine Css; 2, due to missing sampling time data, and 2, due to sample extraction errors. The final sample comprised 61 patients (25 MER and 36 PTZ). Table 1 shows the baseline characteristics of the patients.
Table 1. Sociodemographic and clinical characteristics of the study population

APACHE: Acute Physiology and Chronic Health Evaluation; CNS: central nervous system; IQR: interquartile range; Md: median; MER: meropenem; MV: mechanical ventilation; PTZ: piperacillin/tazobactam; sd: standard desviation; SOFA: Sequential Organ Failure Assessment; x: median.
PK/PD data
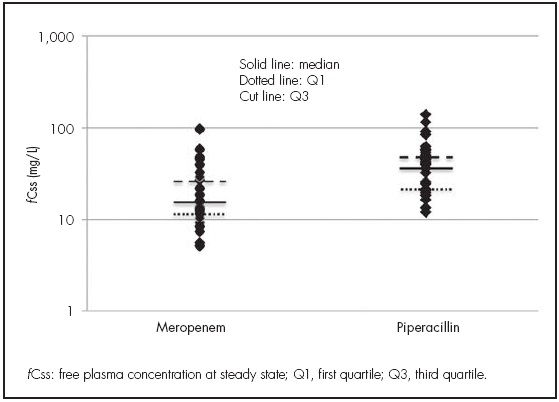
Although all the samples were analysed, fCss alone were used in this analysis. The median fCss was 16 mg/L (11-29) for MER and 40 mg/L (21-51) for PIP (see Figure 1).
Primary objective (100% f T≥ 4 x MIC)
Assuming theoretical MIC values for all patients, 43% (P. aeruginosa) and 72% (enterobacteriaceae) of them would reach the target PK/PD index. Overall, microbiological isolation was achieved in 36 patients and the exact MIC was determined in 35. More than 90% of these patients reached the primary PK/PD target index (95% with PTZ and 94% with MER) (see Table 2).
Table 2. Patient distribution according to the primary and secondary PK/PD targets and the calculated glomerular filtration ranges

MER: meropenem; PIP: piperacillin; MIC: minimum inhibitory concentration; GFR: glomerular filtration rate; fCss: plasma concentration of free drug at steady state.
*P value: chi-square.
¥The percentages of patients who reached the target in each GFR group were calculated using all the patients belonging to each GFR group.
°Microorganisms are listed in table 1.
Secondary objectives
Using either theoretical or real MIC values, more than 90% of patients would reach the PK/PD target of 100% fT≥ MIC (Table 2). No differences were detected between the GFR groups, although some patients with a GFR ≥ 120 mL/min did not reach the PK/PD target index. Figure 2 shows the fCss/MIC ratio by GFR group.
Discussion
The present study confirmed the results reported by other authors9,20,21, who found that drug under-exposure in critically ill patients could be avoided by the administration of antibiotics by CI, which is a simple alternative to classic administration. Dulhunty et al.9 and Abdul-Aziz et al.20,21 studied patients receiving BLAs by IIn or CI and analysed differences in the PK/PD index between groups. Their patients and our patients had similar characteristics. Dulhunty et al. used the same doses of antibiotics as those used in the present study. They found that 82% of patients in the CI group reached Css above the MIC for P. aeruginosa (100% with MER and 75% with PIP)9. Abdul-Aziz et al. analysed exposure after the administration of 18 g/d PTZ, 3 g/d MER, and 6 g/d cefepime. They found that 97% of the f Css in the CI group reached the target of 100% fT> MIC. It is noteworthy that the use of higher PTZ doses reached a median f Css of 4 MICs in 100% of patients, in contrast to the results obtained in our study. The differences in exposure obtained with PTZ and MER could be explained by differences between the median GFR in our study population (95 mL/min/1.73 m2) and that in the population (64 mL/min) studied by Abdul-Aziz et al.20. The results of the present study (43% patients reached fCss> 4 x MIC) were better than those obtained in another study by Abdul-Aziz et al.21, in which only 31% of the patients in the CI group reached this target.
Regarding the debate on the fCss/MIC ratio and the dosing interval percentage3,7, some in vitro and animal model studies have suggested that Css should be maintained at four to five times above the MIC to achieve an acceptable cure rate using CI regimens. The majority of these studies were conducted using resistant GNB (MIC of 64 mg/L for ceftazidime)22. For this reason, the secondary objective addressed 100% of the dosing interval instead of the 40% to 50% described in previous studies3. It is commonly argued that the higher the dosing interval percentage with Css > MIC in critical patients, the higher the probability of survival (odds ratios, 1.02 (95% CI, 1.01-1.04) for 50% fT> MIC and 1.56 (95% CI, 1.15-2.13) for 100% fT> MIC)6.
A potential limitation of this study was the use of the CKD-EPI formula to determine renal function. This method was used because it was impossible to conduct 8- to 24-hour urine collection to directly measure creatinine13,23. However, the CKD-EPI was considered to provide a more accurate calculation and prevent underestimation in those with GFR ≥ 60 mL/min15. One study24 has shown that patients with increased renal function are less likely to reach the target PK/PD index. In the present study, no statistical significance was observed in relation to PK/PD target attainment in patients with a high GFR, but this result could be explained by the small sample size. Future analyses will include more patients to obtain more robust results and to be able to compare them to those of previous studies.
In this study, two analyses were performed according to the MIC value. Given that in 50% of cases no microorganism was isolated, the main and secondary objectives were analysed assuming theoretical MICs based on the breakpoint provided by EUCAST. This aspect may be another limitation, because it overestimated the number of patients who did not reach the target PK/PD index. Nevertheless, the estimation is representative of actual clinical settings, in which the MIC is rarely available at the time of antibiotic treatment. Pharmacokinetics are affected by another relevant factor, hypoalbuminemia, which is found in 40% of critical patients25. Since the percentage of free drug is responsible for the bactericidal effect, measuring total plasma concentrations can lead to the under- or overestimation of the fCss. This situation applies to BLAs due to their high protein binding (more than 70% in ceftriaxone or ertapenem)26, but is not considered a limitation of MER or PIP, which have very low and moderate protein binding, respectively27. Nevertheless, to increase the accuracy of the results, unbound concentrations were also analysed. Finally, it should be noted that therapeutic ranges cannot be defined, because they depend on the MIC of the microorganism, the patient’s clinical/toxicity status, and pathophysiology, all of which may compromise drug exposure (i.e., high distribution volume or hyperfiltration)24,28. Given that there is no established range for these types of antibiotics, the concentration thresholds considered to be toxic were taken as the reference maximum values: 150 mg/L for PIP (fCss 105 mg/L)29 and 64 mg/L for MER (fCss 62 mg/L)30.
More clinical trials are needed to establish therapeutic targets and assess their clinical impact on critical patients.
Conventional doses of MER by CI were sufficient to reach the two PK/ PD targets to treat suspected infections by microorganisms with high MICs, such as Pseudomonas aeruginosa or enterobacteriaceae, which are common in ICUs. Nevertheless, higher doses of PTZ were required to achieve a 100% fT≥ 4 x MIC. However, when microbiological isolation was achieved (i.e. the MIC was known), standard doses of MER and PTZ were sufficient to obtain both target PK/PD indices. The present study found that in patients with elevated renal function there was a slight, but non significant, trend towards subtherapeutic concentrations. Pharmacotherapeutic monitoring is highly recommended to optimize treatment in critically ill patients.











 texto en
texto en