Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Psychosocial Intervention
versión On-line ISSN 2173-4712versión impresa ISSN 1132-0559
Psychosocial Intervention vol.23 no.3 Madrid dic. 2014
https://dx.doi.org/10.1016/j.psi.2014.07.010
Intimate partner violence during pregnancy: Women's narratives about their mothering experiences
Violencia contra la mujer durante el embarazo: Narraciones de mujeres sobre sus experiencias maternales
Ainhoa Izaguirre y Esther Calvete
University of Deusto, Spain
This research was funded by a doctoral grant from the University of Deusto and by a research grant from the Basque government, Ref. PI2011-46, and Bizkailab.
ABSTRACT
Intimate partner violence (IPV) is a significant public health issue and the most common form of violence against women worldwide. Pregnancy does not protect against this phenomenon, which may cause adverse health outcomes for both the mother and the newborn. The main aim of this study was to assess the impact of IPV on women's pregnancies. Thirty-five Spanish women (mean age = 44.23 years, SD = 10.30) who had suffered IPV were interviewed and asked to explain the violent incidents that they experienced, the mothering skills that they developed toward their children, and the difficulties that they experienced at delivery. The results showed that most of the participants continued to experience psychological and physical abuse during their pregnancy, whereas a few of the participants began to experience sexual abuse. As a consequence of IPV, some mothers suffered negative obstetrical outcomes at delivery. The negative effects of IPV on the women's mothering skills were especially remarkable.
Keywords: Pregnancy. Intimate partner violence. Difficulties at delivery. Mothering skills. Qualitative research
RESUMEN
La violencia contra la mujer es un problema de salud pública y la manera más común de violencia hacía la mujer a nivel mundial. El embarazo no es un factor de protección ante tal fenómeno, ya que ser víctima de violencia puede generar efectos negativos tanto en la madre como en el recién nacido. El objetivo principal de este estudio fue evaluar el impacto de la violencia en el embarazo de las mujeres. Se entrevistó a 35 mujeres (M =44.23 años, DT = 10.30) víctimas de violencia para que narraran los episodios de violencia que sufrieron durante el embarazo y las habilidades maternales que desarrollaron para con sus hijos e hijas y explicaran las posibles dificultades que padecieron durante el parto. Los resultados muestran que muchas de las participantes siguieron sufriendo violencia psicológica y física durante el embarazo, mientras que un número reducido de mujeres manifestó haber comenzado a experimentar también episodios de violencia sexual. Como consecuencia de la violencia, algunas mujeres padecieron consecuencias negativas al dar a luz. Es de destacar el impacto de la violencia en las habilidades maternales de las mujeres.
Palabras clave: Embarazo. Violencia contra la mujer. Dificultades durante el parto. Habilidades maternales. Estudio cualitativo
Intimate partner violence (IPV) is a significant social and public health problem that has a high prevalence in most societies. It represents a major threat to the health and well-being of women worldwide (García-Moreno, Heise, Jansen, Ellsberg, & Watts, 2005; Humphreys & Campbell, 2004) regardless of their ethnic origin, economic status, education, religion or profession (Jeanjot, Barlow, & Rozenberg, 2008). IPV includes physical, psychological, and sexual abuse (Heise, Ellsberg, & Gottemoeller, 1999; Krug, Dalhberg, Mercy, Zwi, & Lozano, 2002) and causes serious sequelae in affected women.
Pregnancy does not protect against this phenomenon. For more than two decades, it has been known that pregnant women are not immune to IPV. It is estimated that between 1.2% and 18.4% of pregnant women experience physical, psychological, and/or sexual abuse by a male partner (Bacchus, Mezey, & Bewley, 2006; Gazmararian et al., 1996; Janssen et al., 2003; Jeanjot et al., 2008; Martin, Mackie, Kupper, Buescher, & Moracco, 2001; Mattson & Rodriguez, 1999; Williams & Brackley, 2009). For example, Bacchus et al. (2006) found that the 16 women who participated in their qualitative research had been physically and psychologically assaulted during their pregnancy and that four had experienced sexual violence. Nevertheless, research has shown mixed findings concerning whether pregnancy is a risk factor for the onset of IPV and whether IPV increases in severity during pregnancy (Campbell, Poland, Waller, & Ager, 1992; Helto & Snodgrass, 1987; Hussain & Khan, 2008; McMahon & Armstrong, 2012). Although qualitative studies have suggested that pregnancy may contribute to the onset and/or the increase of IPV (Edin, Dahlgren, Lalos, & Hogberg, 2010; Hussain & Khan, 2008; Jeanjot et al., 2008; Williams & Brackley, 2009), other studies have suggested that IPV during pregnancy is a continuation of earlier violence and is likely to continue following the baby's birth (Campbell, Oliver, & Bullock, 1993; Edin et al., 2010; Heding, 2000; Martin et al., 2001).
When examining IPV during pregnancy, it is important to note that abuse against women can occur at the hands of not only the abusive partner but also in-laws or family members (Bacchus et al., 2006; Jeanjot, et al., 2008; Raj et al., 2011). For instance, Raj et al. (2011) found that more than 1 in 4 women in their study reported such abuse from their in-laws.
The consequences of IPV during pregnancy may be devastating. A growing body of research has documented that IPV heightens women's risk for maternal health problems, such as pregnancy complications and labor complications (Chambliss, 2008; Ellsberg, Janse, Heise, Watts, & García-Moreno, 2008; Leone et al., 2010; World Health Organization, 2005), increased risk for miscarriage (El Kady, Gilbert, Xing, & Smith, 2005; Lipsky, Holt, Easterling, & Critchlow, 2004), poor mental health (Ansara, Cohen, Gallop, Kung, & Schei, 2005; Campbell, Moracco, & Saltzman, 2000; Gottlieb, 2008), placental abruption (Leone et al., 2010; Lewis, 2007), increased rates of prematurity (Bailey, 2010), intrauterine growth restrictions (Janssen et al., 2003), low gestational weight gain (Moraes, Amorim, & Reichenheim, 2006), and infant and child mortality and morbidity, including low infant birth weight and poor infant health (Altarac & Strobimno, 2002; Bailey, 2010; Berenson, Wiemann, Wilkinson, Jones, & Anderson, 1994; Campbell & Lewandowski, 1997; Coker, Sanderson, & Dong, 2004; Gazmararian et al., 1996; Huth-Bocks, Levendosky, & Bogat, 2002; Lipsky, Holt, Easterling, & Critchlow, 2003; Sarkar, 2008; Shah & Shah, 2010; Yost, Bloom, McIntire, & Leveno, 2005). Coggins and Bullock's (2003) qualitative study indicated that 50% of the women in their study had suffered spontaneous abortions or miscarriage.
Furthermore, concerns have been raised regarding women's mothering under circumstances of IPV (Bhandari, Bullock, Anderson, Danis, & Sharps, 2011; Haight, Shim, Linn, & Swinford, 2007; Lapierre, 2010; Levendosky & Graham-Bermann, 2000; Levendosky, Lynch, & Graham-Bermann, 2000; Peled & Gil, 2011; Seeman, Jasinski, & Bubriski-McKenzie, 2013) as the quality of maternal care has been demonstrated to be an important factor that influences on how children are affected by the violence (Cox, Kotch, & Everson, 2003; Hazen, Connelly, Kelleher, Barth, & Landsverk, 2006; Levendosky & Graham-Bermann, 2001; Levendosky, Huth-Bocks, Shapiro, & Semel, 2003). IPV victims are less sensitive and responsive during interactions with their children, often due to psychological difficulties (Hay, Pawlby, Angold, Harold, & Sharp, 2003; Lyons-Ruth, Wolfe, Lyubehik, & Steingard, 2002; Pianta & Egeland, 1990). Nevertheless, little research has described the parenting abilities of IPV victims, and the available studies have found mixed results. Several studies have found that IPV victims' parenting capacities are as effective as non-victims' parenting abilities (Peled & Gil, 2011; Seeman et al., 2013; Whiteside-Mansell, Bradley, McKelvey, & Fussell, 2009) and that these parents may even compensate their children for the parents' IPV (Letourneau, Fedick, & Willms, 2007; Levendosky et al., 2003). However, other studies have shown that the stress that IPV causes to victims may lead to elevated physical and psychological symptoms and the reduced effectiveness of victims' mothering skills (Haight et al., 2007; Lapierre, 2010; Levendosky & Graham-Bermann, 2000). In extreme cases, abused mothers are more likely to be abusive toward their children than non-abused mothers (Huth-Bocks, Levendosky, Theran, & Bogat, 2004; Taylor, Guterman, Lee, & Rathouz, 2009). With regard to this last problem, Haight et al. (2007) found that mothers described their mothering skills as compromised due to IPV, especially during assaults by their abusive partners, when the mothers yelled at or even hit their children.
The Present Study
The literature review shows that pregnant women are not immune to IPV and may suffer various negative effects, such as obstetric risks and difficulties with their mothering skills. However, limited qualitative work has focused on women's experiences of IPV during pregnancy and mothering in the context of IPV (for exceptions, see Bacchus et al., 2006; Edin et al., 2010; Helton, McFarlane, & Anderson, 1987; Lapierre, 2010; Levendosky et al., 2000; Peled & Gil, 2011; Seeman et al., 2013). Furthermore, some findings regarding the trajectory of IPV during pregnancy and the impact of IPV on mothering skills remain inconclusive. Using semi-structured interviews, the current study explores 35 women's beliefs and perspectives concerning their experiences of IPV during pregnancy. The main aims of the current study are as follows: 1) to assess the trajectories of IPV during pregnancy by examining whether IPV changes during pregnancy or remains similar to IPV before the pregnancy, 2) to examine whether IPV episodes during pregnancy cause difficulties during labor, and 3) to determine whether IPV affects women's experiences of mothering.
Method
Study Design
The qualitative research design provides a space for women's voices to be articulated and heard (Bevan, 2014; Maynard, 1994; Reinharz, 1992; Skinner, Hester, & Malos, 2005) and has the potential to enable silenced women to tell their own stories in their own voices (Davis & Srinivasan, 1994). For this purpose, we followed Krueger's (1991, cited in Valles, 1997) classification and developed an interpretative research conducting 35 individual semi-structured interviews with female victims of IPV.
Participants
The participants were 35 women who were recruited from six different agencies for victims of violence, such as shelters, social services, associations, and support groups for women who had experienced IPV in Bilbao and San Sebastian (Basque Country, Spain). These agencies are responsible for individual and group interventions with women who were abused by their partners in both localities and aim to help women end their violent relations and heal from the effects of these relations.
This qualitative study included women who met the following criteria: at least 18 years old, suffered IPV in at least one prior relationship, and had children. At the time of the interviews, the interviewees ranged from 26 to 60 years old (mean age = 44.23 years, SD = 10.30) and had between one and five children, who were aged 1 to 39 years old (mean age = 16.45 years).
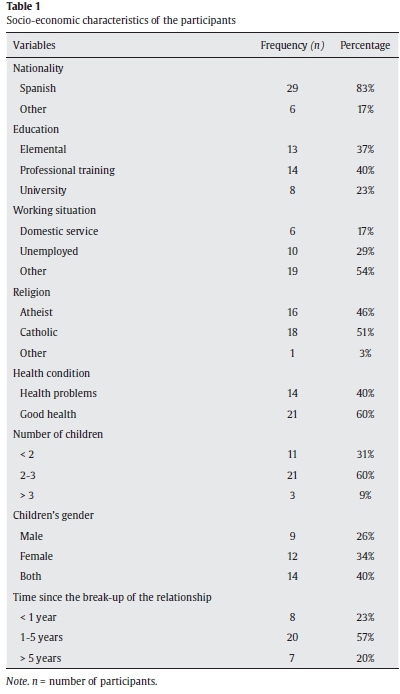
The participants were diverse in nationality, educational level, employment status, religion, and health conditions. Table 1 describes their socio-economic characteristics.
Procedure
After the study was approved by the Basque government authorities, by the Ethics Committee at the University of Deusto and by the coordinators at the various IPV services, workers contacted the women who had received support from these agencies at some stage and who fit the profile. The first author and a psychologist in the sphere of violence against women telephoned the women and provided them with detailed information about the study. Prior to the interview, informed consent was obtained, and the women were handed a "participant's information letter" that outlined the scope, aims, duration of the study, and anonymity prior to the interview. To maintain confidentiality, identifying data were removed and all of the interviewees were given pseudonyms.
The first author and a psychologist in the sphere of violence against women conducted the interviews between February 2012 and June 2013. The interviews lasted between 20 and 150 minutes and were conducted in a university research office and in one agency office. All of the interviews were recorded and transcribed with the participants' permission. As is common practice in qualitative research (Thexton, 2003), remuneration of 20€ was provided to the interviewees for each completed qualitative interview.
Measure
Prior to the interview, a short questionnaire was used to collect sociodemographic data on the participants. The semi-structured interviews were conducted using an interview guide that was based on the specific aims of the study. The interview topics included the following: the prevalence of IPV, experiences of abuse during pregnancy, the difficulties that women suffered at delivery, and the women's perceived mothering skills. Annex I presents the interview question guide.

Analysis
The qualitative data analysis was based on the transcriptions of the semi-structured interviews. All of the interviews were transcribed using the Transana 2.40 program (Fassnacht & Woods, 2009). The text was analyzed using content analysis (Bowling, 1997; Burnard, 1998), and themes were clustered into categories that were identified through the semi-structured schedules that were used for the interviews (DeSantis & Ugarriza, 2000; Morse & Field, 1995). The goal of the thematic analysis was to describe and organize aspects of the phenomenon under study (Boyatzis, 1998). Each interview was reviewed for accuracy and completeness. Further analyses were conducted based on discussions with the co-author, who had access to all of the transcripts. After examining the interviews of the 35 women, we reached saturation in themes and categories (Suárez-Relinque, del Moral-Arroyo, & González-Fernández, 2013).
Results
The analysis of how mothers discussed the impact of IPV on their pregnancy and their mothering skills led to the identification of three main themes. The names of the participants have been changed to protect their identity.
Trajectories of IPV During Pregnancy
This theme describes the women's perceptions of their experiences of IPV before, during, and after pregnancy. The 35 participants suffered IPV at some or all of these three times, including psychological, physical, and sexual abuse. Interestingly, the women's stories showed different trends depending on the type of violence. According to the different narrations, the participants' answers were classified as follows.
Psychological violence. Psychological violence was the most common type of violence experienced by the victims and, in general, was present before pregnancy (n = 28 of 35) and during pregnancy (n = 26). More importantly, psychological abuse increased and was present in all the women after the baby's birth:
"During pregnancies, I suffered psychological violence. When you have them already... it was another story. Psychological violence has been present in my life always and during pregnancy also" (Carmen).
Interestingly, a few of the participants (n = 2) described that mothers-in-law also used psychological violence against them. They explained that they suffered verbal abuse by mothers-in-law in the form of threats and criticisms of their domestic skills. They felt that their husbands reinforced this abuse and therefore it represented an indirect way of abuse against the victims:
"I cried a lot when I was pregnant because my mother-in-law was very violent toward me. She used to threaten me by saying she was going to throw me out of the window" (Maria).
Physical violence. Physical violence appeared to carry over from physical abuse that occurred prior to pregnancy. Whereas psychological abuse was very frequent over the different stages, there was a tendency toward reduced physical violence during pregnancy (from 18 women reporting physical violence victimization before pregnancy to 11 during pregnancy) and increased violence after the baby's birth (27 women, 77.1%). Furthermore, some of the women described that physical violence not only was more frequent but also more severe after giving birth:
"I suffered violence during my two pregnancies. When the girls were born, it was worse. During pregnancy, it slowed a little" (Nerea).
Sexual abuse. The women did not generally report sexual abuse. However, a few of them (n = 3) indicated that they began to suffer sexual abuse in their last months of pregnancy. One of the women continued to experience sexual abuse after childbirth.
"During the pregnancy I was forced to have sex when I did not feel like it" (Leire).
Some women explained that batterers interpreted pregnancy and childbirth as a negative period of time and, as a consequence, they triggered abusive acts. As one mother shared:
"When I was pregnant of my first son I suffered violence (...) but this did not happen in the following pregnancies. Only happened with the first one because my husband felt that the first baby had broken his life" (Joana).
Difficulties at Delivery
This theme describes the negative consequences of IPV for delivery, including rates of prematurity, low infant birth weight, placental abruption, and cesarean delivery. Seven women stated that they had experienced these situations.
Premature labor and low birth weight. Two of the participants explained that their children were one month premature. In both cases, the infant's birth weight was low. One of these two women revealed that the stress that she had suffered could have been the main reason for the premature labor. The following quotation exemplifies these consequences:
"My youngest son was born in my 8th month of pregnancy. The stress I was suffering affected him because he was born with low birth weight" (Ángela).
Placental abruption. One participant specified that the violent incident that she suffered in her 8th month of pregnancy caused devastating consequences that nearly resulted in fetal mortality. The following comment demonstrates this mother's perspective:
"One day, when I was in my 8th month of pregnancy, my ex-husband beat me. I started bleeding, and we went to the hospital. The doctors told me I had suffered a placental abruption. If I had not gone to the hospital, my child would have died" (Lourdes).
Cesarean delivery. The qualitative data established that victims of IPV during pregnancy might have also suffered adverse outcomes such as cesarean delivery. For instance, one participant stated that due to the severe physical violence that she suffered during pregnancy, an urgent cesarean delivery was performed.
"I had a high-risk pregnancy. The doctors had to perform an urgent cesarean delivery" (Nuria).
Pregnancy trauma. Three women reported that the psychological violence that they experienced prevented them from cooperating during the delivery. As one participant commented:
"I was very affected psychologically. This made it very difficult for me to cooperate at delivery time. I could not do it" (Vanesa).
Mothering Skills
The stories provided highlight the effects of IPV on the participants' parenting skills. Women stated being concerned about the impact that IPV could have on their children and also reported an increased sense of responsibility in regard to them. The research findings revealed that IPV created a context that complicated the women's mothering. The participants' responses to this topic were classified into the following three categories.
Effects on parenting. As noted, the common thread in the stories of 28 women was that IPV negatively affected their parenting. Some of the interviewees emphasized their reduced time and energy to dedicate to their children, the increased feelings of concern that they had to address and their increased anger toward their children. One mother stated the following:
"It does affect me because I do not feel good and I cannot behave correctly with my kids. I shout at them, I ask them for too much… yes, it has affected me. When I feel good, they are also fine. They do notice when I am not feeling well because their behavior changes and they act more aggressively" (Raquel).
Positive effects on parenting. Only two of the participants stated that their experiences of IPV had positive effects on their parenting. These women specified that their empathy and caring toward their children increased due to IPV. In addition, they stated that they constantly attempted to protect their children from the potential effects of IPV. The following example demonstrates this perspective:
"IPV has not affected me in a negative way; I think it has been just the opposite. I have always tried to protect my daughters" (Ane).
No Influence on parenting. Three of the participants viewed themselves as good and competent mothers, explaining that their partner's violence did not affect their parenting skills. These participants did not appear to view IPV as a major problem in terms of their parenting skills. As one IPV victim stated:
"As a mother, it hasn't affected me, and this is what I have always tried to do so they could be safe" (Marisa).
Discussion
The present research provides a glimpse into women's IPV experiences during pregnancy and the consequences of IPV. The results of this study reinforce previous studies' findings that IPV victims are not protected during pregnancy (e.g., Bacchus et al., 2006; Janssen et al., 2003; Jeanjot et al., 2008).
The following three main issues emerged from the data: the trajectories of IPV during pregnancy, difficulties at delivery, and the women's experiences of mothering.
Trajectories of IPV during Pregnancy
Most of the women in the current study continued to experience psychological abuse, and many were subjected to physical attacks that jeopardized their safety and the safety of the fetus. In addition, some of the victims began to experience sexual abuse during pregnancy, which is consistent with the data reported by Martin et al. (2004).
The women's narratives also identified the postnatal period as a time of particular risk. In the current sample, the number of women who suffered physical violence increased after childbirth, and several women who previously experienced violence indicated that the violence intensified after childbirth. This increase in physical violence, combined with the fact that 100% of the women reported psychological violence after their child's birth, may be influenced by the distress that family members experience as a consequence of the birth of a child (Cooper, McLanahan, Meadows, & Brooks-Gunn, 2009). Additionally, this finding may be interpreted according to attachment theory (Bowlby, 1977) as the batterer may perceive that the bond with his partner is threatened by the arrival of the new member of the family. This is consistent with several studies that have found that batterers often present negative attachement styles (Holtzworth-Munroe, Meehan, Herron, Rehman, & Stuart, 2000 Holtzworth-Munroe, Stuart, & Hutchinson, 1997). For instance, Holtzworth-Munroe et al. (1997) compared three groups of men: men who were violent against their partners, men who had conflicts with their partners but were not violent, and men without problems with their partners. They found that the violent men scored higher on insecure and anxious attachment style. The insecure attachment style involves an elevated need of closeness and possesivity regarding the partner. As mentioned above, this need can be threatened by the childbirth so that the batterer experiences intense jealousy and anger, traits that are particularly characteristics of the disphoric/ borderline batterers (Amor, Echeburúa, & Loinaz, 2009; Calvete, 2008; Holtzworth-Munroe et al., 2000; Holtzworth-Munroe, 2000). Furthermore, jealousy and possesivity have been identified as key risk factors for violence against intimate partners (Echeburúa, Fernández-Montalvo, de Corral & López-Goñi, 2009). Finally, the increased violence after childbirth may be also due to the mothers' increased vulnerability to coercion because the batterer can employ threats that involve the children as has been suggested by previous studies (Dutton & Goodman, 2005).
Difficulties at Delivery
According to the literature, IPV during pregnancy may result in controversial obstetrical consequences. As previously noted, 20% (n = 7) of the women indicated that they suffered negative outcomes at delivery. Specifically, the consequences that the mothers mentioned included premature and low birth weight (n = 2), placental abruption (n = 1), cesarean delivery (n = 1), and pregnancy trauma (n = 3). These findings are similar to the results obtained in Coggins and Bullock's (2003) qualitative study. In that study's sample of 10 female victims of IPV, 7 suffered negative effects at delivery, such as spontaneous abortions, miscarriage, prematurity and delivery of a large baby.
Although only three of the interviewed women mentioned having suffered pregnancy trauma at delivery, psychological abuse during pregnancy may also lead to poor maternal health and increased psychological distress (Beydoun, Al-Sahab, Beydoun, & Tamin, 2010; Blabey, Locke, Goldsmith, & Perham-Hester, 2009; Ludermir, Lewis, Valongueiro, de Araujo, & Araya, 2010; Tiwari et al., 2008; Yost et al., 1999), which may be associated with several adverse outcomes for the children, such as maladaptive fetal growth and development (Weinber & Tronick, 1998), poor cognitive development and behavior during childhood and adolescence, and negative nutritional and health effects. For instance, the results obtained in the study of Hutch-Bocks et al. (2002) revealed that children of women that have suffered IPV during pregnancy show more indicators of health problems during the first 2 months post-partum compared to children born to women with no IPV experiences. Further research is needed to verify this information as insufficient data was obtained when asking the mothers whether their children had suffered any difficulties at delivery due to IPV.
Women's Experiences of Mothering
Recent studies have suggested that the devastating effects of IPV on the mental health of the women may affect their parenting capacity. This point was verified with the information obtained in the current research as 74% of the participants in this study noted that their mothering skills were negatively influenced. These results are consistent with those of similar qualitative studies that examined battered women's experiences of mothering (Haight et al., 2007; Levendosky et al., 2000).
Nevertheless, in the current study, some women reported that their mothering skills were not affected or were positively impacted. This is consistent with the results of various qualitative investigations (Bhandari et al., 2011; Lapierre, 2010; Peled & Gil, 2011; Rose et al., 2010; Seeman et al., 2013) that found that many of the studied women who were not severely impacted by IPV, spoke positively about their mothering practices, and described themselves as good mothers. These results are very similar to those obtained by Levendosky et al. (2000), in which 20% of the mothers described positive effects on their parenting.
As expected, findings of this study indicate that women, besides the IPV adversities, tried to be protective towards their children and expressed a strong desire for developing good mothering practices. This is consistent with a substantial body of literature that shows that mothers put their children first, regardless of the circumstances (Lapierre, 2010).
Limitations of the Study and Future Lines of Research
This study presents some limitations that should be considered when interpreting the results. The first limitation involves the sample, which only included IPV victims who sought shelter support. Thus, the sample did not represent the broader population of IPV victims. Future research should include victims who have not attended women's shelters. A second important limitation involves the study methodology. The results of qualitative techniques cannot be generalized to the population of women who have suffered IPV (Rolfe, 2006).
Conclusions
The current study contributes new data on the prevalence of IPV before, during, and after pregnancy and the consequences of IPV for delivery and women's mothering skills. The findings indicate that victims of IPV and their children are not protected against violence during pregnancy. Furthermore, the postnatal period seems to be critical for victims' safety as violence often increased after childbirth. Thus, professionals should be particularly vigilant during this period.
Although the majority of the interviewees reported that they suffered IPV in at least one of the three studied moments, a small sample of the participants experienced negative outcomes at the time of delivery. Another noteworthy aspect of the study is that a high percentage of the women reported that IPV affected their mothering skills. However, the variety of responses on this topic suggests that future research should consider all aspects that may influence women's mothering skills. Professionals who work with pregnant women should be vigilant about detecting IPV and helping victims learn to protect themselves and their children.
Conflict of Interest
The authors of this article declare no conflict of interest.
Acknowledgment
The authors wish to express their gratitude to all those who participated in this research and, especially, to the 35 women who shared their personal stories. They also thank Iratxe López for her help conducting some of the interviews.
References
Altarac, M., & Strobimno, D. (2002). Abuse during pregnancy and stress because of abuse during pregnancy and birthweight. Journal of the American Medical Women's Association, 57, 208-214. [ Links ]
Amor, P. J., Echeburúa, E., & Loinaz, I. (2009). ¿Se puede establecer una clasificación tipológica de los hombres violentos contra su pareja? International Journal of Clinical Health & Psychology, 9, 519-539. [ Links ]
Ansara, D., Cohen, M., Gallop, R., Kung, R., & Schei, B. (2005). Predictors of women's physical health problems after childbirth. Journal of Psychosomatic Obstetrics and Gynecology, 26, 115-125. doi: 10.1080/01443610400023064 [ Links ]
Bacchus, L., Mezey, G., & Bewley, S. (2006). A qualitative exploration of the nature of domestic violence in pregnancy. Violence Against Women, 12, 588-604. doi: 10.1177/1077801206289131 [ Links ]
Bailey, B.A. (2010). Partner violence during pregnancy: Prevalence, effects, screening, and management. International Journal of Women's Health, 2, 183-197. [ Links ]
Berenson, A., Wiemann, C., Wilkinson, G., Jones, W., & Anderson, G. (1994). Perinatal morbidity associated with violence experienced by pregnant woman. American Journal of Obstetrics and Gynecology, 170, 1760-1769. doi: 10.1016/S0002-9378(94)70352-3 [ Links ]
Bevan, M. T. (2014). A method of phenomenological interviewing. Qualitative Health Research, 24, 136-144. doi: 10.1177/1049732313519710. [ Links ]
Beydoun, A., Al-Sahab, B., Beydoun, M., & Tamin, H. (2010). Intimate partner violence as a risk factor for postpartum depression among Canadian women in the maternity experience survey. Public Health, 20, 575-583. doi: 10.1016/j.annepidem.2010.05.011 [ Links ]
Bhandari, S., Bullock, L. F. C., Anderson, K. M., Danis, F. S., & Sharps, P. W. (2011). Pregnancy and intimate partner violence: How do rural, low-income women cope? Health Care for Women International, 32, 833-854. doi: 10.1080/07399332.2011.585532 [ Links ]
Blabey, M., Locke, E. R., Goldsmith, Y. W., & Perham-Hester, K. A. (2009). Experience of a controlling or threatening partner among mothers with persistent symptoms of depression. American Journal of Obstetrics & Gynecology, 201, 1-9. doi:10.1016/j. ajog.2009.04.025 [ Links ]
Boyatzis, R. E. (1998). Transforming qualitative data: Thematic analysis and code development. Thousand Oaks, CA: Sage. [ Links ]
Bowlby, J. (1977). The making and breaking of affectional bonds. I. Aetiology and psychopathology in the light of attachment theory. An expanded version of the Fiftieth Maudsley Lecture, delivered before the Royal College of Psychiatrists, 19 November 1976. The British Journal of Psychiatry, 130, 201-210. [ Links ]
Bowling, A. (1997). Research methods in health: Investigating health and health services. Buckingham, UK: Open University Press. [ Links ]
Burnard, P. (1998). Qualitative data analysis: Using a word processor to categorize qualitative data in social science research. Social Sciences in Health, 4, 55-61. [ Links ]
Calvete, E. (2008). Características de salud mental de los hombres que maltratan a su pareja. Revista Española de Sanidad Penitenciaria, 10(2), 26-33. doi:10.4321/S1575-06202008000200004 [ Links ]
Campbell, J. C., & Lewandowski, L. (1997). Mental and physical health effects of intimate violence on women and their children. Psychiatric Clinics of North America, 20, 353-374. [ Links ]
Campbell, J. C., Moracco, K. E., & Saltzman, L. E. (2000). Future directions for violence against women and reproductive health: Science, prevention and action. Maternal and Child Health Journal, 4, 149-154. [ Links ]
Campbell, J. C., Oliver, C., & Bullock, L. (1993). Why battering during pregnancy? AWHONN'S Clinical Issues in Perinatal and Women's Health Nursing, 4, 343-349. [ Links ]
Campbell, J. C., Polland, M., Waller, J., & Ager, J. (1992). Correlates of battering during pregnancy. Research in Nursing & Health, 15, 219-226. doi:10.1002/nur.4770150308 [ Links ]
Chambliss, L. R. (2008). Intimate partner violence and its implications for pregnancy. Clinical Obstetrics & Gynecology, 51, 385-397. doi: 10.1097/GRF.0b013e31816f29ce [ Links ]
Coggins, M., & Bullock, L. F. C. (2003). The wavering line in the sand: The effects of domestic violence and sexual coercion. Mental Health Nursing, 24, 723-738. doi: 10.1080/01612840390219211 [ Links ]
Coker, A. L., Sanderson, M., & Dong, B. (2004). Partner violence during pregnancy and risk of adverse pregnancy outcomes. Paediatric and Perinatal Epidemiology, 18, 260-269. [ Links ]
Cooper, C. E., McLanahan, S. S., Meadows, S. O., & Brooks-Gunn, J. (2009). Family structure transitions and maternal parenting stress. Journal of Marriage and Family, 71, 558-574. doi: 10.1111/j.1741-3737.2009.00619.x [ Links ]
Cox, C., Kotch, J., & Everson, M. (2003). A longitudinal study of modifying influences in the relationship between domestic violence and child maltreatment. Journal of Family Violence, 18, 5-17. doi: 10.1023/A:1021497213505 [ Links ]
Davis, L. V., & Srinivasan, M. (1994). Feminist Research within a battered women's shelter. In E. Sherman & W. J. Reid (Eds.), Qualitative Research in Social Work (pp. 347-357). London: Columbia University Press. [ Links ]
DeSantis, L., & Ugarriza, D. N. (2000). The concept of theme as used in qualitative nursing research. Western Journal of Nursing Research, 22, 351-372. doi: 10.1177/019394590002200308 [ Links ]
Dutton, M. A., & Goodman, L. A. (2005). Coercion in intimate partner violence: Toward a new conceptualization. Sex Roles, 52, 743-756. doi: 10.1007/s11199-005-4196-6 [ Links ]
Echeburúa, E., Fernández-Montalvo, J., de Corral, P., & López-Goñi, J. J. (2009). Assessing risk markers in intimate partner femicide and severe violence: A new assessment instrument. Journal of Interpersonal Violence, 24, 925-939. doi:0.1177/0886260508319370 [ Links ]
Edin, K. E., Dahlgren, L., Lalos, A., & Hogberg, U. (2010). "Keeping up a front": Narratives about IPV, pregnancy, and antenatal care. Violence Against Women, 16, 189-206. doi: 10.1177/1077801209355703 [ Links ]
El Kady, D., Gilbert, W., Xing, G., & Smith, L. (2005). Maternal and neonatal outcomes of assaults during pregnancy. Obstetrics and Gynecology, 105, 357-363. doi: 10.1097/01.AOG0000151109.46641.03 [ Links ]
Ellsberg, M., Janse, H., Heise, L., Watts, C.H., & García-Moreno, C. (2008). Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: An observational study. Lancet, 317, 1165-1172. doi: 10.1016/S0140-6736(08)60522-X [ Links ]
Faasnacht, C., & Woods, D. (2009). Transana 2.40. University of Wisconsin System: Wisconsin Center for Education Research. [ Links ]
García-Moreno, C., Heise, L., Jansen, H. A., Ellsberg, M., & Watts, C. (2005, November). Public health. Violence Against Women. Science, 310, 1282-1283. [ Links ]
Gazmararian, J. A., Lazorick, S., Spitz, A. M., Ballard, T. J., Saltzman, L. E., & Marks, J. S. (1996). Prevalence of violence against pregnant women. Journal of the American Medical Association, 275, 1915-1920. doi: 10.1001/jama.275.24.1915 [ Links ]
Gottlieb, A. S. (2008). Intimate partner violence: A clinical review of screening and intervention. Journal of Women's Health, 4, 529-539. doi: 10.2217/17455057.4.5.529 [ Links ]
Haight, W. L., Shim, W. S., Linn, L. M., & Swinford, L. (2007). Mothers' strategies for protecting children from batterers: The perspectives of battered women involved in child protective services. Child Welfare, 86(4), 41-61. [ Links ]
Hay, D. F., Pawlby, S., Angold, A., Harold, G. T., & Sharp, D. (2003). Pathways to violence in the children of mothers who were depressed postpartum. Developmental Psychology, 39, 1083-1094. doi: 10.1037/0012-1649.39.6.1083 [ Links ]
Hazen, A. L., Connelly, C. D., Kelleher, K. J, Barth, R. P., & Landsverk, J. A. (2006). Female caregivers experiences with intimate partner violence and behavior problems in children investigated as victims of maltreatment. Pediatrics, 117, 99-109. [ Links ]
Heding, L. W. (2000). Postpartum, also a risk period for domestic violence. European Journal of Obstetrics and Gynecology and Reproductive Biology, 89, 41-45. [ Links ]
Heise, L., Ellsberg, M., & Gottemoeller, M. (1999). Ending violence against women. Baltimore: John Hopkins University School of Public Health, Population Information Program. [ Links ]
Helto, A., & Snodgrass, F. (1987). Battering during pregnancy: intervention strategies. Birth, 14, 142-147. doi: 10.1111/j.1523-536X.1987.tb01476.x [ Links ]
Helton, A. S., McFarlane, J., & Anderson, E. T. (1987). Battered and pregnant: a prevalence study. American Journal of Public Health, 77, 1337-1339. doi: 10.2105/ AJPH.77.10.1337 [ Links ]
Holtzworth-Munroe, A. (2000). A typology of men who are violent toward their female partners: Making sense of the heterogeneity in husband violence. Current Directions in Psychological Science, 9, 140-143. doi: 10.1111/1467-8721.00079 [ Links ]
Holtzworth-Munroe, A., Meehan, J. C., Herron, K., Rehman, U., & Stuart, G. L. (2000). [ Links ]
Testing the Holtzworth-munroe and Stuart (1994) batterer typology. Journal of Consulting and Clinical Psychology, 68, 1000-1019. doi:10.1037/0022-006X.68.6.1000 [ Links ]
Holtzworth-Munroe, A., Stuart, G. L., & Hutchinson, G. (1997). Violent versus non violent husbands: Differences in attachment patterns, dependency, and jealousy. Journal of Family Psychology, 11, 314-331. [ Links ]
Humphreys, J., & Campbell, J. C. (2004). Family violence and nursing practice. Philadelphia, PA: Lippincott Williams & Wilkins. [ Links ]
Hussain, R., & Khan, A. (2008). Women's perceptions and experiences of sexual violence in marital relationships and its effects on reproductive health. Health Care for Women International, 29, 468-483. doi: 10.1080/07399330801949541 [ Links ]
Huth-Bocks, A. C., Levendosky, A. A., & Bogat, G. A. (2002). The effects of domestic violence during pregnancy on maternal and infant health. Violence and Victims, 17, 169-185. [ Links ]
Huth-Bocks, A. C., Levendosky, A. A., Theran, S. A., & Bogat, G. A. (2004). The impact of domestic violence on mother's prenatal representations of their infants. Infant Mental Health Journal, 25, 79-89. doi: 10.1002/imhj.10094 [ Links ]
Janssen, P. A., Holt, V. L., Sugg, N. K., Emanuel, I., Critchlow, C. M., & Henderson, A. D. (2003). Intimate partner violence and adverse pregnancy outcomes: A population-bases study. American Journal of Obstetrics & Gynecology, 188, 1341-1347. doi: 10.1067/mob.2003.274 [ Links ]
Jeanjot, I., Barlow, P., & Rozenberg, S. (2008). Domestic violence during pregnancy: Survey of patients and healthcare providers. Journal of Women's Health, 17, 557-567. doi: 10.1089/jwh.2007.0639 [ Links ]
Krug, E., Dalhberg, L., Mercy, J., Zwi, A., & Lozano, R. (2002). Word report on violence and health. Geneva: World Health Organization. [ Links ]
Lapierre, S. (2010). Striving to be "good" mothers: Abused women's experiences of mothering. Child Abuse Review, 19, 342-357. doi: 10.1002/car.1113 [ Links ]
Leone, J. M., Lane, S. D., Koumans, E. H., DeMott, K., Wojtowycz, M. A., Jensen, J., & Aubry, R. H. (2010). Effects of Intimate Partner Violence on Pregnancy Trauma and Placental Abruption. Journal of Women's Health, 19, 1501-1509. doi: 10.1089/ jwh.2009.1716 [ Links ]
Letourneau, N. L., Fedick, C. B., & Willms, J. D. (2007). Mothering and domestic violence: A longitudinal analysis. Journal of Family Violence, 22, 649-659. doi: 10.1007/s10896-007-9099-6 [ Links ]
Levendosky, A. A., & Graham-Bermann, S. A. (2000). Behavioral observations of parenting in battered women. Journal of Family Psychology, 14, 80-94. doi: 10.1037/0893-3200.14.1.80 [ Links ]
Levendosky, A. A., Huth-Bocks, A., Shapiro, D., & Semel, M. (2003). The impact of domestic violence on the maternal-child relationship and preschool age children's functioning. Journal of Family Psychology, 17, 275-287. [ Links ]
Levendosky, A. A., Lynch, S. M., & Graham-Bermann, S. A. (2000). Mother's perceptions of the impact of women abuse on their parenting. Violence Against Women, 6, 247-271. doi: 10.1177/10778010022181831 [ Links ]
Lewis, G. (Ed.) (2007). Saving Mothers' Lives: reviewing maternal deaths to make to make motherhood safer 2004-2005. The Seventh Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. Confidential Enquiry into Maternal and Child Health (CEMACH). London: CEMACH. [ Links ]
Lipsky, S., Holt, V. L., Easterling, T. R., & Critchlow, C. W. (2003). Impact of police-reported intimate partner violence during pregnancy on birth outcomes. Obstetrics and Gynecology, 102, 557-564. doi: 10.1016/S0029-7844(03)00573-8 [ Links ]
Lipsky, S., Holt, V. L., Easterling, T. R., & Critchlow, C. W. (2004). Police-reported intimate partner violence during pregnancy and risk of antenatal hospitalization. Maternal and Child Health Journal, 8, 55-63. doi: 10.1023/B:MACI.0000025727.68281. aa [ Links ]
Ludermir, A., Lewis, G., Valongueiro, S., de Araujo, & Araya, (2010). Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. Lancet, 376, 903-910. doi: 10.1016/S0140-6736(10)60887-2 [ Links ]
Lyons-Ruth, K., Wolfe, R., Lyubehik, A., & Steingard, R. (2002). Depressive symptoms in parents of children under age 3: Sociodemographic predictors, current correlates, and associated parenting behaviors. In N. Halton, K.T. McLarn, & M.A. Schuster (Eds.), Child rearing in America: Challenges facing parents with young children (pp. 217-259). New York: Cambridge University Press. [ Links ]
Martin, S. L., Harris-Britt, A., Li, Y., Moracco, K. E., Kupper, L. L., & Campbell, J. C. (2004). Changes in intimate partner violence during pregnancy. Journal of Family Violence, 19, 201-210. doi: 10.1023/B:JOFV.0000032630.50593.93 [ Links ]
Martin, S. L., Mackie, L., Kupper, L. L., Buescher, P. A., & Moracco, K. E. (2001). Physical abuse of women before, during, and after pregnancy. Journal of American Medical Association, 285, 1581-1584. doi:10.1001/jama.285.12.1581 [ Links ]
Mattson, S., & Rodriguez, E. (1999). Battering in pregnant Latinas. Mental Health Nursing, 20, 405-422. doi:10.1080/016128499248565 [ Links ]
Maynard, M. (1994). Methods, practice and epistemology: The debate about feminism and research. In M. Maynard & J. Purvis (Eds.), Researching Women's Lives from a Feminist Perspective (pp. 10-26). London: Taylor and Francis. [ Links ]
McMahon, S., & Armstrong, D. Y. (2012). Intimate partner during pregnancy: Best practices for social workers. Health & Social Work, 37, 9-17. doi: 10.1093/hsw/hls004 [ Links ]
Moraes, C. L., Amorim, A. R., & Reichenheim, M. E. (2006). Gestational weight gain differentials in the presence of intimate partner violence. International Journal of Gynaecology and Obstetrics, 95, 254-260. doi: 10.1016/j.ijgo.2006.08.015 [ Links ]
Morse, J. M., & Field, P. A. (1995). Qualitative research methods for health professionals. Thousand Oaks, CA: Sage. [ Links ]
Peled, E. & Gil, B. (2011). The mothering perceptions of women abused by their partner. Violence Against Women, 17, 457-479. doi: 10.1177/1077801211404676 [ Links ]
Pianta, R. C., & Egeland, B. (1990). Life stress and parenting outcomes in a disadvantage sample: Results of the mother-child interaction project. Journal of Clinical Child Psychology, 19, 329-336. doi: 10.1207/s15374424jccp1904_4 [ Links ]
Raj, A., Sabarwal, S., Decker, M. R., Nair, S., Jethva, M., Krishnan, S., … Silverman, J. G. (2011). Abuse from in-laws during pregnancy and post-partum: Qualitative and quantitative findings from low-income mothers of infants in Mumbay, India. Maternal and Child Health Journal, 15, 700-712. doi: 10.1007/s10995-010-0651-2 [ Links ]
Reinharz, S. (1992). Feminist Methods in Social Research. New York: Oxford University Press. [ Links ]
Rolfe, G. (2006). Validity, trustworthiness and rigour: Quality and the idea of qualitative research. Journal of Advanced Nursing, 53, 304-310. [ Links ]
Rose, L., Alhusen, J., Bhandari, S., Soeken, K., Marcantonio, K., Bullock, L., & Sharps, P. (2010). Impact of intimate partner violence on pregnant women's mental health: Mental distress and mental strength. Issues in Mental Health Nursing, 31, 103-111. doi: 10.3109/01612840903254834 [ Links ]
Sarkar, N. N. (2008). The impact of intimate partner violence on women's reproductive health and pregnancy outcome. Journal of Obstetrics and Gynaecology, 28, 266-271. doi: 10.1080/01443610802042415 [ Links ]
Seeman, I., Jasinski, J. L., & Bubriski-McKenzie, A. (2013). Subjection, subjectivity, and agency: The power, meaning, and practice of mothering among women experiencing intimate partner abuse. Violence Against Women, 19, 69-88. doi: 10.1177/1077801212475335 [ Links ]
Shah, P. S., & Shah, J. (2010). Maternal exposure to domestic violence and pregnancy and birth outcomes: a systematic review and meta-analyses. Journal of Women's Health, 19, 2017-2031. doi: 10.1089/jwh.2010.2051 [ Links ]
Skinner, T., Hester, M., & Malos, E. (2005). Methodology, feminism and gender violence. In T. Skinner, M. Hester, & E. Malos (Eds.), Researching Gender Violence. Feminist Methodology in Action (pp. 1-22). Willem: Cullompton. [ Links ]
Suárez-Relinque, C., del Moral-Arroyo, G., & González-Fernández, M. T. (2013). Consejos prácticos para escribir un artículo cualitativo publicable en Psicología. Psychosocial Intervention, 22, 71-79. doi: 10.5093/in2013a9 [ Links ]
Taylor, C. A., Guterman, N. B., Lee, S. J., & Rathouz, P. J. (2009). Intimate partner violence, maternal stress, nativity, and risk for maternal maltreatment of young children. American Journal of Public Health, 99(1), 175-183. [ Links ]
Thexton, W. (2003). Introducing qualitative research in psychology. Maidenhead, UK: McGraw-Hill. [ Links ]
Tiwari, A., Chan, K. L., Leung, W., Brownridge, D., Lam, H., Wong, B., … Ho, P. C. (2008). The impact of psychological abuse by an intimate partner on the mental health of pregnant women. Psychosexual Health, 115, 377-384. doi: 10.1111/j.1471-0528.2007.01593.x [ Links ]
Valles, M. S. (1997). Técnicas cualitativas de investigación social: Reflexión metodológica y práctica profesional. Madrid: Síntesis. [ Links ]
Weinber, M. K., & Tronick, E. Z. (1998). Emotional characteristics of infants associated with maternal depression and anxiety. Pediatrics, 102, 1298-1304. [ Links ]
Whiteside-Mansell, L., Bradley, R. H., McKelvey, L., & Fussell, J. J. (2009). Parenting: Linking impacts of interpartner conflict to preschool children's social behavior. Journal of Pediatric Nursing, 24, 389-400. doi: 10.1016/j.pedn.2007.08.017 [ Links ]
Williams, G. B., & Brackley, M. H. (2009). Intimate partner violence, pregnancy and the decision for abortion. Mental Health Nursing, 30, 272-278. doi: 10.1080/01612840802710902 [ Links ]
World Health Organization (2005). World report on violence and health: Summary. Geneva. [ Links ]
Yost, N. P., Bloom, S. L., McIntire, D. D., & Leveno, K. J. (2005). A prospective observational study of domestic violence during pregnancy. Obstetrics & Gynecology, 106, 61-65. doi: 10.1097/01.AOG.0000164468.06070.2a [ Links ]
 Correspondence:
Correspondence:
e-mail: ainhoa.izagirre@deusto.es
Manuscript received: 20/06/2014
Accepted: 01/08/2014














