Introduction
Virtual reality (VR) technology delivers sensory stimuli to generate a perceptual and interactive experience of a realistic and immersive environment (Rizzo et al., 2019). VR is defined as a computer generated, three-dimensional environment that is viewed using dual-display stereoscopic technology such as head mounted displays (HMDs) (Clough & Casey, 2011; Riva et al., 2016; Turner & Casey, 2014). The past decade has seen unprecedented industrial developments and advancements in the technological specifications of VR. Improvements in computing power, graphics, advanced processing speed, and greater internet connectivity has resulted in increased access and consumer demand for VR (Rizzo et al., 2019). VR is now widely and easily available in the home, resulting in greater potential reach and accessibility for VR interventions (VRIs) for mental health. However, despite earlier predictions that VR would revolutionise mental health care (Newman et al., 2011), many VRIs are yet to reach their full potential (Botella et al., 2017; Serrano et al., 2019).
Research is increasingly demonstrating the therapeutic benefits of VRIs for various mental health conditions, though interventions rarely translate from research to application in clinical settings (Cipresso et al., 2018; Mishkind et al., 2017). Establishing efficacy does not guarantee uptake and routine use, with only 50% of clinical innovations translating to routine care (Bauer & Kirchner, 2019; Kirchner et al., 2020; Wiederhold & Riva, 2019). VRIs offer great promise for overcoming barriers to care, reducing unmet client need, enhancing existing preventative approaches, and improving service delivery (Clough & Casey, 2011; Clough, Eigeland, et al., 2019). A lack of commercially available VRIs highlights the need for a better understanding of the clinical features associated with translation and uptake. The current review provides a synthesis of research in this field, particularly regarding clinical features of VRIs for emotional disorders (EDs).
Virtual Reality Interventions for Mental Health
VRIs apply VR technology to promote psychological and/or behavioural change to achieve symptom reduction in clinical, subclinical, and non-clinical populations (Turner & Casey, 2014). VRIs can create environments suitable for training and treatment in both controlled and multi-sensory environments where dynamic clinical presentations can be observed and recorded (Rizzo et al., 2019). Like many digital interventions for mental health, VRIs can be used for promotion, case management, coaching, symptom-focused treatment, and comprehensive therapy (Reynolds et al., 2015). VRIs vary across theoretical orientation (e.g., cognitive behavioural therapy, dialectical behaviour therapy etc.), dosage (e.g., number of sessions), duration (e.g., time), and degree of therapist involvement (e.g., completely involved to no involvement). Some VRIs are deployed in traditional face-to-face therapy as an adjunct to existing treatment while others may be designed to be self-guided or therapist assisted. Yet despite this variability across VRIs, one commonality can be seen in the frequent application of VRIs for disorders with strong cue-exposure components such as anxiety disorders (Mishkind et al., 2017).
Features of Virtual Reality Interventions
Key features of VR include immersion, presence, and simulator sickness. Immersion refers to the stimulation of senses within a virtual environment that mimics interactions and experiences in reality (Cipresso et al., 2018). Immersion is the extent to which experiences in virtual environments achieve realism. The more extensive, surrounding, inclusive, vivid, and matching reality the virtual environment, the higher the degree of immersion (Slater et al., 1995). In this way, immersion can be considered as the objective level of sensory fidelity that a VR system can provide through its virtual environment (Bowman & McMahan, 2007). Presence is a complex state of feeling that is elicited by a virtual environment, and is described as a state of feeling that is ‘life-like' or ‘being there' (Cipresso et al., 2018). Previous research has attempted to examine the relationship between presence and cybersickness (Weech et al., 2019). Cybersickness is an adverse physiological response to a virtual environment that results in bodily discomfort (i.e., nausea, vertigo, dizziness, etc.) (Weech et al., 2019). Presence and cybersickness are negatively related in that virtual environments that are more realistic tend to elicit a greater sense of presence and immersion, which corresponds with fewer reports of cybersickness (Weech et al., 2019). Intrusive factors that decrease presence and increase the likelihood of cybersickness include sensory mismatch, VR display factors (i.e., less than 20 frames per second, low field-of-view, etc.), vection (i.e., the illusion of self-motion in relation to the brain's sensorimotor control system), intuitiveness of interactivity with the virtual environment, navigation control, and gaming experience. Immersion, presence, and cybersickness appear to be important components that influence engagement (Ling et al., 2014; Weech et al., 2019), but how these influence various clinical outcomes remain poorly understood.
Efficacy of Virtual Reality Interventions
The capacity to create tailored, stepped, and safe environments through VR has resulted in substantial evidence focussing on the use of this technology for the treatment of anxiety, phobias, and PTSD (Arroll et al., 2017; Botella et al., 2017; Carl et al., 2019; Fodor et al., 2018; Goncalves et al., 2012; Valmaggia et al., 2016). A number of comprehensive reviews (Clough & Casey, 2011; Clough & Casey, 2015b), systematic reviews (Botella et al., 2017; Goncalves et al., 2012; Valmaggia et al., 2016), and meta-analyses (Carl et al., 2019; Fodor et al., 2018) have demonstrated the clinical efficacy of VRIs for many psychopathologies (Carl et al., 2019; Valmaggia et al., 2016; Wiederhold & Riva, 2019). However, these have mainly been for the treatment of unidimensional disorders (e.g., anxiety disorders), as opposed to related disorders of emotion (Arroll et al., 2017; Botella et al., 2017; Carl et al., 2019; Fodor et al., 2018). The potential of VRIs to be utilised in the treatment of emotional disorders (e.g., anxiety, anxiety related, and unipolar mood disorders) remains a sparsely researched area.
Novel Virtual Reality Interventions
Single-disorder treatment protocols often lack external validity, do not provide guidance on how to address co-occurring disorders, and require clinicians to demonstrate expertise in administering various manual-based protocols (Cassiello-Robbins et al., 2020). Transdiagnostic treatment protocols are increasingly being adopted in clinical research and have translated into clinical practice (Cassiello-Robbins et al., 2020), but whether this has also occurred in VRIs is unknown. VRIs have the capacity to target core processes that are relevant across a variety of clinical domains (Rizzo et al., 2019). VRIs can be tailored to higher order dimensions of similar disorders, making it an efficacious modality that may achieve improvements in translation efforts. Indeed, in the broader digital mental health field, it has been identified that translation and long-term consumer use of mental health technologies, such as mobile applications, may only be achieved if a transdiagnostic approach is utilised (Chandrashekar, 2018).
Novel elements such as transdiagnostic VRIs, remote, or self-guided VRIs are some ways in which this modality of treatment can be optimised to achieve greater translation from research to clinical practice. Transdiagnostic VRIs could meet clients' needs in co-morbid populations, whilst remote or self-guided VRIs can overcome access barriers and increase the capacity of this technology to be used outside of the laboratory. Indeed, the technological advancements observed in untethered HMDs, such as the Oculus Quest, make this a particularly important time to review the evidence base and clinical features of VRIs for EDs.
Emotional Disorders
Consistent with previous research (Barlow et al., 2004; Brown & Barlow, 2009; Bullis et al., 2019), EDs are defined as a psychological disorder that is associated with the experience of frequent and intense negative emotions, elicits an aversive reaction to the negative emotional experience that is driven by the individual's diminished sense of control and negative appraisal of the emotion, and results in the individual avoiding or lessening their emotional experience in reaction to the onset of a negative emotion state (Bullis et al., 2019; Cassiello-Robbins et al., 2020). It has been argued that such disorders share common aetiology and maintaining mechanisms, and as such may be treated via the same approaches (Barlow, 2004). EDs included in the current review were: anxiety disorders, such as generalised anxiety, panic disorder, social anxiety; specific phobias; agoraphobia; obsessive-compulsive disorders; unipolar depressive disorders; mood disorders; and PTSD. Emerging research suggests the inclusion of related disorders in the classification of EDs (i.e., insomnia, eating disorders, and borderline personality disorders) (Bullis et al., 2019); however, more research examining the relationships between higher order dimensions of these related disorders is needed. Therefore, insomnia, eating disorders, and associated disorders of emotion are not included in this review. Within the face-to-face psychological literature, considerable focus has been given in recent years to understanding treatment response across the emotional disorders, with two recent systematic reviews focussing on these issues (Gonzalez-Robles et al., 2018; Sakiris & Berle, 2019). However, the extent to which VR may be a useful treatment approach across the emotional disorders remains unknown.
Study Aim
The current review set out to provide an updated synthesis of research within this field. To date, systematic reviews and meta-analytic studies have focussed on the efficacy of VRIs for unidimensional classifications of disorders as opposed to broader disorders of emotion (Botella et al., 2017; Carl et al., 2019; Fodor et al., 2018). In addition, reviews to date have primarily focussed on the efficacy of VRIs, with only limited attention given to factors related to translation. As such, the primary aim of this systematic review was to concurrently examine the efficacy of VRIs for EDs and investigate select clinical and technological features (such as dosage, degree of therapist guidance, treatment approach, VR specifications) that may influence translation of treatments from research to clinical practice. It is anticipated that examining these issues concurrently will provide a discussion for improving uptake and implementation of efficacious VRIs for EDs.
Method
The systematic review was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Moher et al., 2010) guidelines. The protocol for the review was pre-registered with PROSPERO (CRD42019135795).
Literature Search and Search Strategy
Studies were sourced by conducting a comprehensive systematic literature search in the electronic databases of Medline, PsycINFO, Embase, and Cumulative Index of Nursing and Allied Health Literature (CINAHL). The search strategy consisted of the following search terms:
“virtual reality” OR “virtual” OR “VR” OR “augmented reality” OR “AR” OR “altered reality”
“anxiety disorder*” OR “depressive disorder*” OR “mood disorder*” OR “generalised anxiety disorder*” OR “social anxiety disorder*” OR “panic disorder*” OR “obsessive compulsive disorder*” OR “OCD” OR “post-traumatic stress disorder*” OR “PTSD” OR “major depressive disorder*”
Exploded and mesh terms for (i)
Exploded and mesh terms for “anxiety disorder*” AND “depressive disorder*” AND “mood disorder*”
i OR iii
ii OR iv
v AND vi
The peer review of electronic search strategies guidelines and checklist for systematic reviews (McGowan et al., 2016) was applied to the search strategy, and appraised by independent reviewers before conducting the final search.
Inclusion and Exclusion Criteria
A comprehensive search was conducted to obtain articles published from 1989 to 2019. Experimental studies were deemed eligible for inclusion based on the following criteria: a treatment study that included participants over the age of 18, with a primary diagnosis of an ED, that was confirmed using validated self-report or clinician rated measure/s or by way of diagnostic interviewing. Full text studies needed to be available in English and published in the most recent decade (2010-2019). Publication date was kept as the last step in the exclusion of studies so that the authors could better understand advancements in VR technology, contextualise historical trends of research within this field, and source studies for preliminary checks in consistency of raters (see Risk of Bias and Quality Assessment section below).
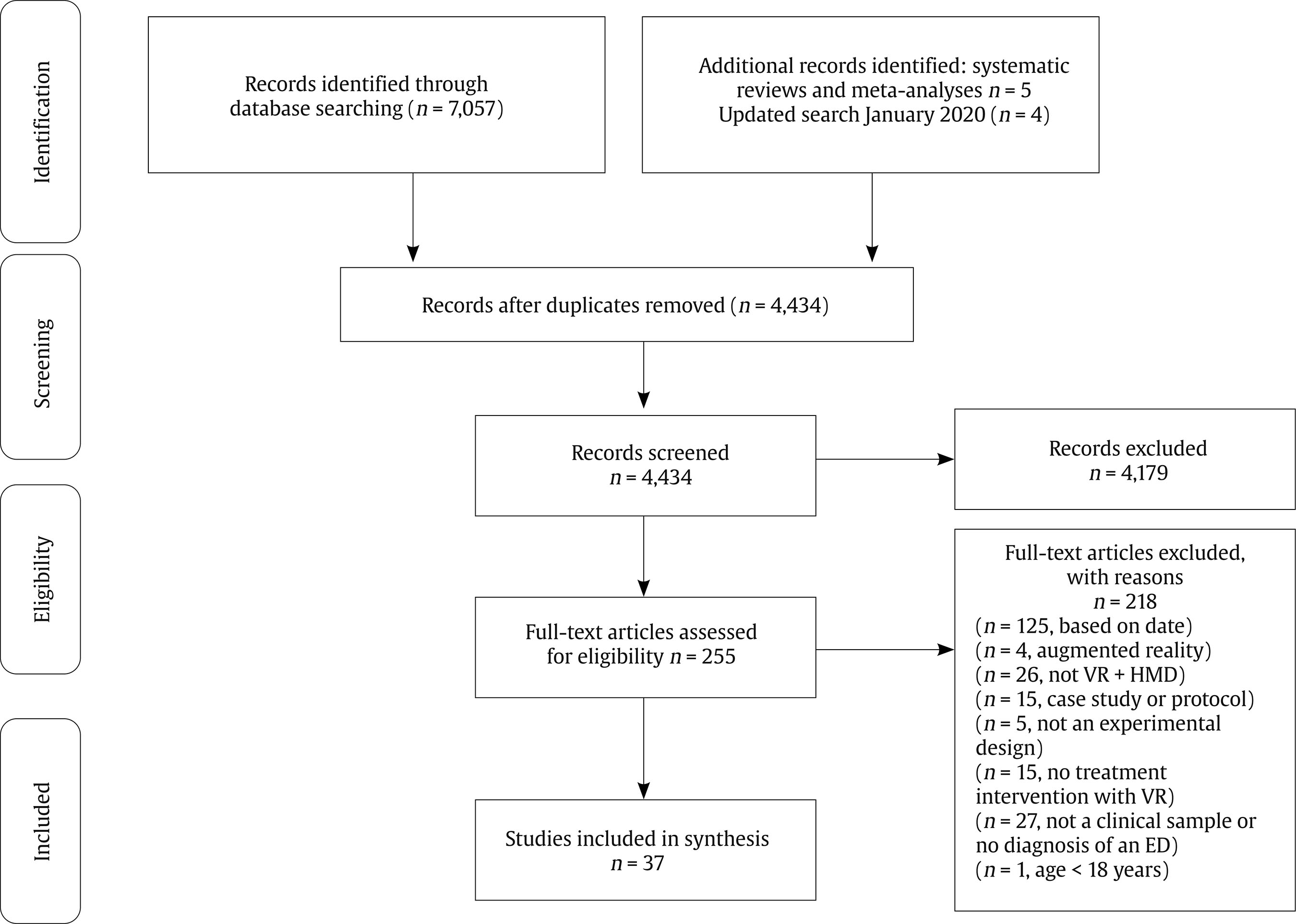
Studies were excluded if they did not adequately describe or include a virtual reality intervention (e.g., virtual experiences through computer displays, projectors such as cave automatic virtual environment) that utilised an HMD (e.g., VR headset, 3D glasses, goggles). Further exclusions were made if studies failed to provide enough information about the design, intervention, VR apparatus, or clinical characteristics of participants (Figure 1). Non-experimental study designs, studies lacking empirical data, single case studies, and study protocols were excluded as they did not meet the criteria for evaluation and quality assessment. Studies containing psychopharmacological agents or disorders beyond those of emotion, or presence of comorbidity with a disorder not considered an emotional disorder, were also omitted (e.g., psychotic disorders, neurodevelopmental disorders) as treatment effects could not be examined independently.
Screening, Study Selection and Data Extraction
The process of study selection is displayed in Figure 1. The initial search was conducted in March 2019 and resulted in 4,425 non-duplicated articles, 3,629 of which were published between 1989 and 2019 (updated search conducted and independently reviewed in January 2020). Following removal of duplicates and studies published in languages other than English, titles and abstracts were screened. The removal of studies was then guided by the inclusion and exclusion criteria. Screening and data extraction were conducted independently by the lead author [DR] and an independent reviewer. Criteria for data extraction were determined prior to commencing the review. To ensure accuracy of data extraction, authors [DR, AG] recorded data using a standardised form. Initial data collected at screening included sample size, study design, mean age, diagnostic assessment, intervention features (i.e., use of HMD, dosage, duration), main findings, and limitations. Disagreement and discrepancies between reporting were resolved through discussion. Extracted data were synthesised descriptively. The rate of agreement was calculated at 86.1%. Consensus was reached through discussion and input from members of the research team [BC, LC]. Following full-text screening and data extraction, a total of 37 studies remained.
Risk of Bias and Quality Assessment
The ROBIS risk of bias assessment tool (Whiting et al., 2016) was selected to assess the methodological quality of the included studies. Assessment of bias consisted of random sequence generation (D1), allocation concealment (D2), blinding of participants and personnel (D3), blinding of outcome assessment (D4), incomplete outcome data (D5), selective reporting (D6), and other bias (D7). The Critical Appraisal Skills Programme, 2018 (CASP) for RCTs checklist was also utilised to assess the methodological quality of studies (2018). In ensuring the criteria were applied consistently, the quality of assessments for risk of bias and CASP was tested on three studies (Banos et al., 2002; Coelho et al., 2008; Rothbaum et al., 2000) published before 2010. These articles were randomly sampled from a pool of excluded studies (k = 33), using a random number generator. The studies met all other inclusion criteria except publication date. This procedure was employed to ensure consensus could be reached between the raters [DR, AG] prior to, and throughout the assessment of the final articles (n = 37). CASP and risk of bias were examined for all articles by the first author [DR], with a subset of studies (60%) selected at random for independent review [AG]. The inter-rater agreement for the preliminary assessment of risk of bias and CASP was 85.7% (k = 3). For the final articles (n = 37) the inter-rater agreement for risk of bias was 77.9% (n = 22) and 80.2% for the CASP (n = 23). Discrepancies were resolved through discussion between raters and authors [LC, BC].
Results
Overview of Included Studies (n = 37)
Most studies were conducted in Europe (k = 18), with specific phobias being the most commonly researched disorder (k = 12). Only one study examined a VRI for more than one type of phobia (Moldovan & David, 2014), namely social, height, and flying phobias. The most common therapeutic approach was CBT, with virtual reality exposure therapy (VRET) being the most frequent technique applied in treatment (k = 35). Interestingly, none of the resultant articles examined the effect of VRIs for depressive disorders, a combination of disorders/transdiagnostic application, nor for OCD. Few VRIs could be used with minimal guidance by a therapist or utilised remotely (k = 5), with interventions primarily focused on coaching, symptom-focused treatment, or comprehensive therapy (Reynolds et al., 2015).
Table 1. Overview of Included Studies by Disorder (n = 37)

Note. ABS II = Attitudes and Beliefs Scale II; ACQ: Agoraphobia Cognitions Questionnaire; ADIS-IV = Anxiety Disorders Interview Schedule for DSM-IV; AQ = Acrophobia Questionnaire; ASC-P = Appraisal of Social Concerns – Probability subscale; ASC-C = Appraisal of Social Concerns – Consequence subscale; ASI = Anxiety Sensitivity Index; ATHQ = Attitude toward Height Questionnaire; ATQ30 = Automatic Thoughts Questionnaire; BAT = Behavioural Approach Task; BAI = Beck Anxiety Inventory; BBQ = Brunnsviken Quality of Life Scale. BDI = Beck Depression Inventory; BFNE = Brief Fear of Negative Evaluation Scale; BSQ = Bodily Sensation Questionnaire; CAPS-5 = Clinician-administered PTSD Scale for DSM-5; CAS = Chambless Agoraphobic Questionnaire; CGI = Clinical Global Impressions Scale; CSQ-8 = Client Satisfaction Questionnaire; CTQ = Childhood Trauma Questionnaire Short Form; DAS = Dysfunctional Attitude Scale; DASS 21 = Depression Anxiety Stress Scale; DEFAS = Danger Expectations and Flying Anxiety Scales; DERS = Difficulties of Emotion Regulation Scale; DES = Dissociative Experience Scale; DFS = Dental Fear Scale; ERS = Experience Rating Scale; EUROHIS-QOL = Eurohis Quality of Life Scale; FAM = Flight Anxiety Modality Questionnaire; FAQ = Focus of Attention Questionnaire; FAS = Flight Anxiety Situation Questionnaire; FFMQ = Five Facets of Mindfulness Questionnaire; FFQ = Fear of Flying Questionnaire; FFS = Fear of Flying Scale. FNE-B = Fear of Negative Evaluation Brief Form; FSQ = Fear of Spiders Questionnaire – French version. FQ = Fear Questionnaire; GAD-7 = General Anxiety Disorder 7 items. GAF = Global Assessment of Functioning; GPQ = Gatineau Presence Questionnaire GSE = General Self-Efficacy Questionnaire; HAMA = Hamilton Anxiety Rating Scale. HADS = Hospital Anxiety and Depression Scale; HIQ = Heights Interpretation Questionnaire; IAPT = Improving Access to Psychological Therapies Scale; IASMHS = Inventory of Attitudes toward Seeking Mental Health Services; IPQ = Igroup Presence Questionnaire; ITC-SOPI = Independent Television Company SOP Inventory; ITQ = Immersive Tendency Questionnaire; LIS = Life Interference Scale; LSAS-SR = Liebowitz Social Anxiety Scale-Self Reported Version; MAIA = Multidimensional Assessment of Interoceptive Awareness; M-FAST = Miller-Forensic Assessment of Symptoms; MIA: Mobility Inventory for Agoraphobia; MINI = Mini International Neuropsychiatric Interview; MSAQL = Manchester Short Assessment of Quality of Life; NEQ-32 = Negative Effects Questionnaire; PCL-5 = PTSD Checklist for DSM-5; PCL-C = PTSD Checklist Civilian Version; PCL-M = PTSD Checklist – Military Version; PDBQ = Personality Disorder Belief Questionnaire; PDSS = Panic Disorder Severity Scale; PHQ-9 = Patient Health Questionnaire; PPGAS = Panic, Phobia and Generalized Anxiety Scale; PRCS = Personal Report of Confidence as a Speaker; PRJQ = Presence and Reality Judgment Questionnaire; PQ = Presence Questionnaire; PSE-SQ = Perceived Self-Efficacy towards Spiders Questionnaire; PTS = Paranoid Thoughts Scale; QMI = Questionnaire upon Mental Imagery; SAS = Social Adjustment Scale; SBQ = Spider Beliefs Questionnaire; SCID-I = Structured Clinical Interview for Axis-1 Disorders; SCID-II: Structured Clinical Interview for Axis-1 Disorders; SCQ: Social Costs Questionnaire; SDS: Sheehan Disability Scale; SESS: Self-Efficacy for Social Situations Scale; SF-36 = The Medical Outcome Studies 36-item Short Form Health Survey; SPRS = Social Performance Rating Scale; SPQ = Spider Phobia Questionnaire; SPS = Social Phobia Scale; SIAS = Social Interaction Anxiety Scale; SoPQ = Sense of Presence Questionnaire; SOQ = Session Opinion Questionnaire; SSPS = Self Statements during Public Speaking Scale; SSQ = Simulation Sickness Questionnaire; SSRPH = Stigma Scale for Receiving Psychological Help; STAI = State Trait Anxiety Inventory; SUD = Subjective Units of Discomfort; SWEAT = Specific Work for Exposure Applied in Therapy; TC/E = Treatment Credibility/Expectancy Questionnaire; TES = Therapist Evaluation Scale; TPQ = Treatment Preference Questionnaire; TRES = Therapeutic Relationship Evaluation Scales; VAS = Visual Analogue Scale; WAI-SF = Working Alliance Inventory Short Form; WSA = Work and Social Adjustment Scale.
A variety of recruitment strategies were employed to develop and test VRIs, these included but were not limited to, self and clinician referrals through universities, health services, workplaces, social media, and other online advertising. VRIs were typically tested in research settings (k = 35) over primary health care settings (k = 1). All VRIs were delivered individually, with therapists or research personnel tailoring treatments to clients during exposure based VRI (k = 35). Studies frequently reported that the VRI was adapted from traditional treatment protocols (k = 29). Most research utilised VR HMDs that were tethered, costly, and manufactured prior to 2010. Most VR experimental conditions were efficacious when compared to waitlist and control conditions with mostly large treatment effects (Table 1). The precision of treatment effects was infrequently reported and only a small number of studies (k = 6) included at least one or more VR specific measures (i.e., presence, immersion, cybersickness) and one or more client centric measures of treatment (i.e., treatment satisfaction, preference, acceptability). A more detailed summary of the included studies is provided in Table 1.
Efficacy of VRIs
The majority of VRIs outperformed waitlist controls on various self-report measures of social anxiety (Anderson et al., 2013; Bouchard et al., 2017; Kampmann et al., 2016; Kim et al., 2017; Lindner, Miloff, Fagernas, et al., 2019; Robillard et al., 2010), panic disorder with/without agoraphobia (Meyerbröker et al., 2011; Meyerbroeker et al., 2013; Pelissolo et al., 2012); PTSD (Reger et al., 2016), and various specific phobias (Freeman et al., 2018; Michaliszyn et al., 2010; Raeder et al., 2019; Shiban, Brutting, et al., 2015). Many VRIs were either equally effective or not statistically different from other active treatment conditions, such as for social anxiety disorder (Anderson et al., 2013; Robillard et al., 2010), panic disorder and agoraphobia (Malbos et al., 2013; Pelissolo et al., 2012; Quero et al., 2013), PTSD (Beidel et al., 2019; Norr et al., 2019; Reger et al., 2019), and various specific phobias (Lindner, Miloff, Fagernas, et al., 2019; Michaliszyn et al., 2010; Raeder et al., 2019; Rus-Calafell et al., 2013; Tortella-Feliu et al., 2011). Some VRIs were more effective than active treatments for social anxiety (Bouchard et al., 2017), PTSD (McLay et al., 2011), and specific phobia (Gujjar et al., 2019). Conversely, active treatment conditions in three studies outperformed VRIs across measures of social anxiety (Kampmann et al., 2016) and PTSD symptomology (McLay et al., 2017; Reger et al., 2016).
Methodological Features of Studies
Of the final studies, 19 were randomised control trials (RCTs), with the remainder of studies consisting of two open trials, one multiple baseline design, one parallel case series, and the remainder (k = 14) consisting of other observational analytic study designs. All studies clearly addressed a focussed issue, with most randomising participants to conditions (k = 29). Few studies adequately reported on information pertaining to randomisation method, type of randomisation, and how random allocation sequencing occurred. Fourteen studies explicitly reported on statistical power, nine of which met power estimates. Most studies comprised small samples, with intervention groups consisting of 54 participants or less. Only two studies were conducted in hospital settings (Levy et al., 2016; McLay et al., 2011), with the remainder taking place in research laboratories or tertiary institutions. Dropout rates in the current systematic review were similar to those reported in meta-analytic studies (Carl et al., 2019; Turner & Casey, 2014). It is important to note that some studies had minimal attrition (Freeman et al., 2018; Geraets et al., 2019; Kim et al., 2017; Tortella-Feliu et al., 2011) (Table 1). High incidences of attrition appeared to be more common in VRIs for PTSD, though attrition rates were still similar to those seen in traditional face-to-face interventions (Beidel et al., 2019; Deng et al., 2019) and other meta-analytic studies of VRIs for anxiety disorders (Beidel et al., 2019; Benbow & Anderson, 2019; Deng et al., 2019). Assessment of risk of bias domains revealed that concealment of allocating participants to groups was problematic, as was reporting of incomplete outcome data (Figure 2). Interestingly, many VRIs achieved clinical significance in the presence of sub-optimal methodological rigour, and these previous observations were independent of effect size (Turner & Casey, 2014). A full appraisal of each study against the CASP is displayed in Appendix.
Clinical Features of VRIs
Dosage, duration, and frequency. A high degree of variability in dosage, duration, and frequency of VRIs was evident (Table 2). Frequency of treatment ranged from one-session treatment to twenty sessions of VR and duration of VRIs varied from 5 minutes to 120 minutes. Some studies scheduled breaks for participants, with most studies immersing participants sequentially for shorter intervals to mitigate adverse effects such as simulator sickness. This variability makes it difficult to distinguish optimal dosage, duration, and frequency of VRI sessions by disorder.
Table 2. Clinical Characteristics of VRI Studies by Disorder

Note. 1Approximate. Hyphen (-) indicates data not available.
Presence, immersion, and simulator sickness. VR specific measures, such as presence, immersion, simulator sickness, visual analogue, and body sensation, were included in a small number of studies (Table 1). Of the studies that included measures of presence, mixed findings were reported. Non-significant relationships were found between perceived presence and treatment efficacy in Malbos et al. (2013). Based on the difference between scores between pre-test and post-test on various dependent variables, small insignificant positive correlations were found between the presence questionnaire and the agoraphobia cognitions questionnaire (r = .15, p = .56), depression anxiety stress scales (r = .36, p = .15), and the mobility inventory for agoraphobia (r = .10, p = .36) (Malbos et al., 2013). No significant differences were observed in a behavioural approach task for spider phobia, with scores at post-treatment for those with high-presence compared to those with low presence scores (ß = .90, 95% CI = -0.32 to 2.13, p = .14) suggesting perceived levels of presence in a VRI compared to in-vivo exposure did not influence improvements in a behaviour task (Lindner, Milhoff, Fagernas, et al., 2019).
Navarro-Haro et al. (2019) found a gradual decrease in presence scores as participants progressed through VR sessions for flying phobia, whereas mean scores on the presence questionnaire increased between and across treatment sessions for social anxiety disorder (Bouchard et al., 2017). However, these increases in scores across sessions did not significantly predict decreases in symptomology. Results from one study revealed that presence did not moderate pre-treatment and post-treatment anxiety scores for various phobias (i.e., social, flying, and height phobia) (Moldovan & David, 2014), nor did presence predict reduction of fear in a VRI for spider phobia (Tardif et al., 2019). Two studies included the immersive tendency questionnaire by Witmer and Singer (1998). Neither study found a significant relationship between immersion and improvements in treatment outcome (Moldovan & David, 2014; Tardif et al., 2019). These findings indicate that the role of presence and immersion in treatment outcome in VR remains unclear. In reference to translation, VRIs with sub-optimal immersive environments can still be effective in the treatment of certain psychological disorders. Consumers and clinicians have the option to forgo more costly HMDs with greater technical specifications (i.e., FOV, frames per second, etc.) for those that create a more affordable immersive experience.
The effects of simulator sickness on treatment outcomes were also mixed, despite all using the simulator sickness questionnaire (SSQ) by Kennedy et al. (1993). Freeman et al. (2018) reported consistently low levels of simulator sickness across the treatment period for flying phobia (first treatment session M = 2.21, p < .001 and last treatment session M = 1.35, p = .002). Scores on the SSQ did not significantly predict attrition in the treatment of SAD (Bouchard et al., 2017), but scores were shown to be significantly higher in a clinical sample of SAD comparted to a non-clinical sample (Kim et al., 2017) and this was consistent across treatment sessions (t50 = -3.12, p = .003). Scores on the SSQ varied among other studies examining VRET for agoraphobia (M = 14.0, SD = 8.50) (Malbos et al., 2013) and spider phobia (M = 7.80, SD = 6.51) (Tardif et al., 2019). These findings indicate that simulator sickness may be more common at the start of treatment and may influence early termination of treatment, particularly in clinical populations. However, no clear link to other treatment outcomes was observed in the included studies.
Therapist involvement. As reported elsewhere (Newman et al., 2011), most VRIs tend to include a high degree of therapist involvement. Some studies reported the role of the therapist as being a point of contact for questions pertaining to treatment or in assisting with troubleshooting of VR technology (Freeman et al., 2018; Kampmann et al., 2016). Others reported minimal therapist involvement in VR treatment, suggesting that some VRIs may have potential for remote use in the physical absence of a therapist. Certain studies emphasised the role of the therapist as an active agent in the design and development of virtual environments that could be tailored to the client's therapeutic needs, such as personalized exposure scenarios (Freeman et al., 2018; Loucks et al., 2019). None of the studies quantified the extent of therapist involvement (i.e., minutes per session), and few clearly reported on the primary role of the therapist in each respective VRI. The impact of therapist involvement in many of the included studies on outcome remains inconclusive. Table 2 demonstrates the extent of therapist involvement across studies. Few studies reported minimal to no therapist guidance and the capacity of VRI to be used remotely as a standalone or adjunctive consumer-led intervention remains largely unexplored.
Remote VRIs. Five of the included studies had no or minimal therapist guidance (Freeman et al., 2018; Kim et al., 2017; Levy et al., 2016; Lindner, Miloff, Fagernas, et al., 2019). Levy et al. (2016) treated hospital outpatients with acrophobia from a remote distance using VRET. Three sessions consisted of remote VRET, while the remaining three were conducted in a traditional therapy office in the presence of the therapist. Findings revealed no significant differences in experiences of anxiety, presence, or working alliance between the remote VRET and guided VRET sessions, suggesting that participants had similar experiences remotely to traditional VRET. Freeman et al. (2018) used a virtual coach to guide participants through an inexpensive VRET (“Now I Can Do Heights”) for fear of heights. This VRI was designed to be used without a therapist; however, it could be delivered by a therapist in a traditional clinical setting. The virtual coach provided psychoeducation from a cognitive perspective and asked participants to rate their fear on a series of questions. The underlying mechanism of treatment was for individuals to determine how accurate their fears were, identify and challenge safety-seeking behaviors, and mitigate avoidance towards challenging scenarios. Uptake and completion of the full course of treatment were high (n = 44, 90%) and the authors noted that treatment effects (d = 2.0) far exceeded those seen in a meta-analysis of therapist assisted exposure treatments (d = 1.1) (Wolitzky-Taylor et al., 2008).
Promising findings also have been observed for remote VRIs for social anxiety disorder (Kim et al., 2017; Lindner, Miloff, Fagernas, et al., 2019). Kim et al. (2017) sought to examine whether mobile-based VR self-training was as valid and effective as VRET based on previous studies (Anderson et al., 2013; Kampmann et al., 2016; Robillard et al., 2010). Significant treatment effects were observed for VR self-training and for group (non-clinical vs. clinical social anxiety disorder) on the HADS, LSAS, and the SIAS. Improvements were reported for both conditions for general anxiety, performance anxiety, and social interaction anxiety, as well as depression.
In Lindner, Milhoff, Fagernas, et al.'s (2019) study, treatment for fear of public speaking comprised either one session of exposure therapy with a therapist or one session of self-led VRET. Both conditions demonstrated strong treatment effects, with the therapist-led condition more efficacious (d = 1.67) than the self-led VRET condition (d = 1.38). Participants from both conditions subsequently completed a four week, online modular program that promoted transition to in-vivo exposure. This study provides an example of the capacity for VR to be combined with other digital mental health interventions for efficacious remote delivery of treatments. Similarly in Lindner, Miloff, Fagernas, et al.'s (2019) subsequent study relating to treatment of spider phobia, one-session treatment with a therapist was compared to one session of self-led VRET, with both conditions demonstrating strong treatment effects. Therapists in both studies (Lindner, Miloff, Fagernas, et al., 2019; Lindner, Miloff, Zetterlung, et al., 2019) took on a “computer technician” role and were to provide care if a serious emotional response was elicited. One commonality that can be seen in these studies is their application of consumer available VR hardware (e.g., HTC Vive, Samsung Gear VR). Such technology would allow for easy remote delivery of self-led interventions, although this would need to be explored further in future research. Although minimal studies have been conducted to date, early findings are promising for the delivery of in home and remote interventions.
Treatment Experience
Few studies included one or more measures of user engagement, treatment satisfaction, or attitudes towards VRIs. Studies that did include secondary outcome measures relating to user engagement included client satisfaction (Anderson et al., 2013), session opinion and treatment preference (Botella et al., 2014), working alliance (Anderson et al., 2013; Moldovan & David, 2014), mental health associated stigma (Mishkind et al., 2017), access and attitudes towards psychological treatment (Freeman et al., 2018; Reger et al., 2016), and the therapeutic relationship (Michaliszyn et al., 2010; Pelissolo et al., 2012). Scores from the experience rating scale-therapist version demonstrated that prior to administering either treatments therapists held more pessimistic views towards VRET than traditional face-to-face CBT for panic disorder with agoraphobia (p = .01). However, patients' expectancies of either treatment did not differ (Pelissolo et al., 2012). No differences were observed for ratings of the therapeutic relationship between VRET or CBT.
Other Features of VRI Technology
Most studies utilised HMDs and other VR equipment that was manufactured prior to 2010 (Table 3). Compared with the advanced VR technology currently available to consumers, the technological specifications of VR equipment used in the studies reviewed were substandard. According to a multi-user study by Mehrfard et al. (2019), comparative analysis revealed that three specific HMDs (i.e., Samsung Odyssey+, Oculus Rift S, and the HTC Vive) performed better across various metrics such as comfort, image quality, weight, and tracking stability. These HMDs were not common among studies in this review, with most of the HMDs having poorer technical specifications, such as lower display resolutions, narrower field of view (FOV), less intuitive head tracking degrees of freedom (DOV), and were tethered to a computer, which incurred additional costs. These were the eMagin z800 and the nVisor sx60, and have been reported to be the two most commonly used HMDs in mental health research (Jerdan et al., 2018).
Table 3. Specifications for Head Mounted Displays (Jerdan et al., 2018; Snoswell & Snoswell, 2019; Wiederhold & Riva, 2019)
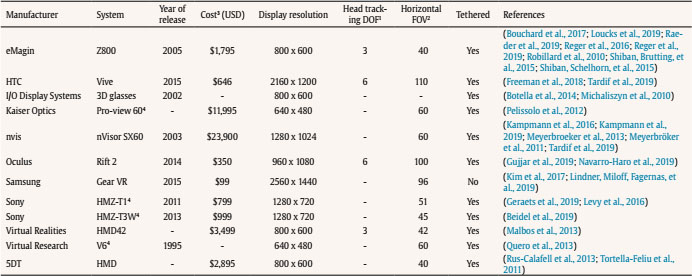
Note. 1DOF = degrees of freedom; 2FOV = field of view; 3approximate cost; 4discontinued VR system. Hyphen (-) indicates data not available.
Studies (k = 7) that specified use of a HMD but not system (Anderson et al., 2013; Gebara et al., 2016; McLay et al., 2014; McLay et al., 2017; McLay et al., 2012; McLay et al., 2011; Moldovan & David, 2014; Norr et al., 2018).
The affordability of recent VR technologies is widely reported (Bouchard et al., 2017; Kim et al., 2017; Mehrfard et al., 2019), yet no study in the current review reported the exact cost of VR HMDs or accompanying equipment. Internet searches and previously reported price points of HMDs revealed that most of the studies used costly and outdated HMDs (Table 3). Despite the ubiquity of mobile phones, few of the studies included them as a cost effective platform for delivering VRIs via HMDs (e.g., Samsung gear VR, Google Cardboard VR etc.) (Kim et al., 2017; Lindner, Miloff, Fagernas, et al., 2019). Mid-range VR HMDs, such as the Oculus Quest, Oculus Go, and HTC Vive, were also underutilised. None of the included studies reported on the commercial availability of their VRI, and it was unclear if any of the VRIs from the included studies were to be made available to consumers after publication.
Discussion
The aim of this review was to examine efficacy of VRIs for EDs in relation to not only outcome, but also various translational factors that influence the availability of VRIs in clinical and consumer settings. This review provides an updated synthesis of research on VRIs for psychological treatment and extends upon previous systematic reviews and meta-analytic studies, which have examined the efficacy of VRIs for unidimensional classifications of disorders (Botella et al., 2017; Carl et al., 2019; Fodor et al., 2018). The review highlights the extent to which VRIs have been effective for single disorder treatment, predominantly in the application of exposure techniques and as an adjunct to traditional treatments for anxiety disorders and PTSD. However, key gaps relating to transdiagnostic and remote application of VRIs for the treatment of EDs have also been identified. At the start of this decade it was predicted that “as technological innovations continue to develop, the efficacy, portability, and feasibility of the use of technology should continue to grow” (Newman et al., 2011, pp. 100-101). However, across digital mental health technologies, difficulties with translation into clinical practice have been observed, including in the translation of VRIs. We argue that the gaps identified by this review help to explain these translation difficulties.
Main Findings
The efficacy of VRIs for anxiety disorders and PTSD has been widely reported and are supported in the current review (Botella et al., 2017; Carl et al., 2019; Deng et al., 2019; Fodor et al., 2018), yet few have become available outside of research settings with little translation into clinical contexts (Mishkind et al., 2017; Wiederhold & Riva, 2019). To the best of the authors' knowledge, none of the included studies had effectively translated treatment from research to a commercially available VR program, ready for consumer use in the home or clinician uptake in practice settings. Furthermore, none of the included studies reported that the VRI was to be made available to consumers or clinicians, despite promising rates of compliance and completion of these treatments. Research is emerging for remote or minimally guided VRIs, though translation of these into the home remains poorly understood. In addition, although transdiagnostic VRIs offer great promise for overcoming translational issues, research is yet to thoroughly explore this.
Methodological Rigour
While VRIs may yield significant treatment effects in the face of suboptimal reporting, translational research is often outpaced by the ongoing development, updates, and iterations of VR technologies (Mishkind et al., 2017). Rapid prototyping and iterations of VRIs are often not possible due to the significant time delays that exist between demonstration of clinical efficacy in RCTs, to implementation and routine use of evidence-based treatment in practice (Clough & Casey, 2015a; Kirchner et al., 2020). There is considerable room for improvement in the methodological reporting of VRI studies as many studies did not adequately describe the VR apparatus, cost of HMDs, or include measures of engagement, immersion, or presence. As such, the quality of the associated VR software programs was unable to be assessed. This lack of detail in reporting limits implementation efforts and complicates replication of studies.
Similar to findings reported elsewhere (Fodor et al., 2018), results from the risk of bias assessment and study appraisal revealed various methodological considerations related to appropriate and insufficient reporting of randomisation, group allocation procedures, reasons for participant attrition, and data management. Indeed, much of the research reported on originally developed, idiosyncratic VRIs, without reference to broader dissemination or commercial availability. Most of the included studies applied costly (> $1,000 USD), outdated (manufactured prior to 2010), and discontinued HMDs that are not accessible to consumers. Mobile phone-compatible VRIs are an accessible treatment modality that take advantage of the untethered and portable nature of mobile phones. However, this review revealed only three studies in which a mobile HMD was used (Kim et al., 2017; Lindner, Miloff, Fagernas, et al., 2019). VRIs were identified as an efficacious adjunct to traditional treatment, in combination with other technology-based interventions such as video-conference therapy via Skype (Pedram et al., 2020), and as a top-up to one-session VRET with online modules for computerised exposure therapy for public speaking anxiety (Lindner, Miloff, Fagernas, et al., 2019). Taken together, these studies demonstrate the capacity of VRIs to be used for remote, in person, and blended psychological treatment approaches, although the area is still in its infancy.
Implications
VRIs are well established as an efficacious treatment modality, particularly for disorders of anxiety and fear. They are a compelling modality for delivering transdiagnostic skills training such as mindfulness, psychoeducation, and cognitive restructuring, although further research in needed to explore these intervention options in VR. Better translation of VRIs for EDs could provide consumers with the opportunity to engage in client-centred, self-guided therapeutic interventions (i.e., through interactive and immersive: mindfulness exercises, skill practice, distraction tasks, psychoeducation, and feedback) in the home, and could be an effective avenue for the prevention of mild to moderate presentations. Furthermore, an in home, transdiagnostic VRI that simulates client-tailored scenarios could be useful in enhancing dosage effects of treatment between traditional face-to-face appointments. Self-guided or remote VRIs could further promote client autonomy with treatment, improve adherence to homework activities between sessions, and may be effective in overcoming barriers to traditional treatment such as stigma and access.
The recent production of more affordable (less than $1,000 USD), high quality, and portable VR hardware (e.g., Oculus Rift, HTC Vive, Google Cardboard) such as those applied by Donker et al. (2019), is promising for consumers and clinicians. The capacity for VRIs to meet client need through the continued provision of structured instructions and immediate feedback is a compelling solution to the translation of treatment into the home. Remotely accessible and self-guided VRIs have the potential to further improve treatment coverage by circumnavigating travel barriers and costly logistics of exposure treatments (Newman et al., 2011).
Other factors that have been reported to limit translation include selecting appropriate, efficacious and evidence-based VRIs (Mehrfard et al., 2019) which may be due to knowledge deficits, limited awareness of VRIs, misconceptions about their cost, clinical efficacy, utility, concerns for working alliance, and deficits in competence with VR technology (Clough, Eigeland, et al., 2019; Clough, Rowland, et al., 2019; Lindner, Miloff, Zetterlund, et al., 2019). In achieving greater translation of VRIs, there is a need for standardized clinical training and education in available and validated VR treatment protocols with explicit directions on how to implement them (Lindner, Miloff, Zetterlund, et al., 2019; Mishkind et al., 2017; Wiederhold & Riva, 2019).
Recommendations and Limitations
VRI studies have been outpaced by rapid advancements in technology and as such it is imperative that innovative research designs be considered. Research designs such as sequential multiple assignment randomized trials (Almirall et al., 2014) or multiphase optimisation strategy trials (Collins et al., 2007) have the capacity to bridge the digital divide and keep pace with ongoing technological iterations and updates required by many third party VR market places (such as the App Store, SteamVR, and the Oculus store). Dismantling studies could be an efficacious strategy for determining the active technological and therapeutic components of treatment that are needed to optimise translation (Newman et al., 2011; Rizzo et al., 2019). Such approaches may also help to improve the quality of research within this field. Future research should clearly report data on the software used, level of engagement and immersion, and quantify the extent of therapist involvement in minimally guided VR treatments.
Studies typically consisted of small samples that lacked statistical power and did not provide adequate detail on VR apparatus, cost-effectiveness, inclusion of a control group and transparent and complete reporting (Fodor et al., 2018). Similar to previous reviews (Fodor et al., 2018; Jerdan et al., 2018), the current review cannot conclude which VR program or HMD is most optimal for clinical use, although this review was limited in its exclusions of non-three-dimensional VR equipment and interventions that did not explicitly use a HMD for the treatment of an ED in a clinical sample of adults.
Finally, although considerable attention has been given to issues of efficacy within this field, it is recommended that future research focus on issues of dissemination and translation. This may include development of clinician training programs to promote adjunctive use of VRIs in practice, a focus on development of commercially available VRIs, and development of repositories or databases for publicly available programs. The latter already exists in many countries, with a focus on online programs and mobile apps (e.g., www.emhprac.org.au). Inclusion of VRIs in these databases would allow clinicians and consumers to easily search for appropriate programs and review the evidence and technical specifications of each, facilitating easier translation for clinical practice and remote use.
Conclusion
Although VR is becoming more accessible in the consumer market, few VRIs for psychological disorders have translated from research to practice. This systematic review provides an update on the current status of VRIs for EDs. The potential of VRIs to improve mental health is continuously being showcased by innovative research and technological transformation. To the best of the authors' knowledge, no VRI has been explicitly designed for the transdiagnostic treatment of EDs. Given the overlap in the aetiology of mood and anxiety disorders and their prevalence in comorbid and co-occurring clinical presentations, a shift away from disorder specific treatment protocols towards a transdiagnostic approach may enhance translation efforts, as is the current focus in many face-to-face treatments. VRIs can target core processes that are relevant across a variety of clinical domains and greater attention should be given to the capacity of VRIs to be utilised for more than just the exposure component of treatments. It is crucial that commercially available HMDs are used with VRIs so that accessible self-help, self-guided, and remote options for care can be used in the home. Further, VRIs that are tailored to higher order dimensions of similar disorders, such as EDs, and which may be delivered remotely, may considerably enhance the translation and reach of these interventions.