Introduction
Intimate partner violence (IPV) against women has been internationally recognized as a serious and widespread phenomenon of epidemic proportions that includes physical, sexual, economic, social, and psychological harm toward women perpetrated by a current or former male intimate partner (World Health Organization [WHO, 2013, 2014]). According to a recent WHO (2021) report on global IPV prevalence estimates, 27% of ever-married or partnered women aged 15-49 years have suffered physical and/or sexual violence from a current or former male intimate partner at least once in their lifetime. The persistently high prevalence of IPV has led governments and organizations to implement intervention programs for IPV perpetrators to promote healthy behaviours alternative to violence for male perpetrators convicted of IPV offences to reduce recidivism and protect victims (Scott et al., 2011; Voith et al., 2018; WHO, 2021). Intervention programs for IPV perpetrators can be mandated by courts in lieu of incarceration, or perpetrators can self-refer to some intervention programs (Cheng et al., 2021; Dalton, 2007). Reviews on the effectiveness of such intervention programs for court-mandated IPV perpetrators have found mixed results, with positive but low to moderate effect sizes on reducing recidivism (Arce et al., 2020; Babcock et al., 2004; Cheng et al., 2021; Feder & Wilson, 2005; Santirso et al., 2020; Smedslund et al., 2011; Stephens-Lewis et al., 2021). Scientific literature in this field has pointed to the main challenges that hinder the effectiveness of intervention programs for IPV perpetrators, specifically, high dropout rates, low treatment adherence, low levels of personal responsibility attribution, and low levels of motivation to change, which are particularly present in court-mandated (Bowen & Gilchrist, 2004), high-risk, and highly resistant perpetrators (Carbajosa et al., 2017; Eckhardt et al., 2008; Jewell & Wormith, 2010). Risk factors that increase the occurrence of IPV recidivism in these perpetrators include previous mental health issues (Petersson & Strand, 2017), sociodemographic characteristics (i.e., immigrant status), childhood experience and/or exposure to family violence, experience of stressful life events (Lila et al., 2019), trauma (Kwong et al., 2003), and substance use (Langenderfer, 2013). Another challenge that has been widely recognized in scientific research is the lack of individualized intervention programs specifically tailored to participants’ risk factors such as substance use and/or other underlying problems (Butters et al., 2021; Karakurt et al., 2019).
Alcohol and/or other drug use problems (ADUPs) have been strongly and consistently associated with IPV perpetration (Cafferky et al., 2018). Approximately 50% of perpetrators attending intervention programs for IPV have ADUPs (Crane et al., 2015; Kraanen et al., 2010; Stuart et al., 2003; Stuart et al., 2009). Although ADUPs are “neither a necessary nor a sufficient cause, excessive alcohol use does contribute to the occurrence of partner violence and that contribution is approximately equal to other contributing causes such as gender roles, anger, and marital functioning” (Leonard & Quigley, 2017, p. 7). In addition, ADUPs are strongly associated with low treatment adherence, dropout, recidivism, and severe violence in perpetrators court-mandated to attend IPV intervention programs (Bowen & Gilchrist, 2006; Easton et al., 2018; Jewell & Wormith, 2010; Lila et al., 2020; Moore & Stuart, 2004; Olver et al., 2011). Thus, perpetrators with ADUPs have been identified as a high-risk, highly resistant group of IPV perpetrators who may require tailored interventions to address their IPV perpetration (Gilchrist & Hegarty, 2017). Compared to those without ADUPs, risk factors associated with ADUPs in this population include poorer cognitive abilities (Romero-Martínez et al., 2016; Romero-Martínez, Lila, & Moya Albiol, 2019; Vitoria-Estruch et al., 2017), exposure to childhood trauma (Alexander, 2014; McBurnett et al., 2001), stressful life events (Lila et al., 2013), less perceived social support (Catalá-Miñana et al., 2017; Taft et al., 2010), psychopathological symptoms (Stuart et al., 2003; Thomas et al., 2013), impulsivity, antisocial, borderline, and aggressive personality disorders (a term coined by Millon (2007) describing a clinical personality pattern characterized by a tendency to act impulsively, violently and antisocially; (Expósito-Álvarez et al., 2021). In consideration of the above characteristics, dealing with perpetrators with ADUPs and other associated risk factors frequently represents a challenge for professionals in these intervention programs (Karakurt et al., 2019; McMurran, 2017).
Several authors state that risk assessments are required to help professionals to identify specific risk and protective factors in IPV perpetrators with ADUPs (Leonard & Quigley, 2017), and develop treatment plans sensitive and responsive to these risk factors and treatment needs (Finkel, 2007; Massa et al., 2020; Travers et al., 2021). Achieving abstinence or reducing ADUPs alone has been shown to have positive but not sustained effects on reducing IPV recidivism in this high-risk and highly resistant group of perpetrators (Wilson et al., 2014). Thus, identifying and addressing risk factors associated with ADUPs could have the potential to improve IPV perpetrator program effectiveness (Karakurt et al., 2019; Leonard & Quigley, 2017; Murphy & Ting, 2010). This could be especially beneficial for court-mandated participants who, compared to self-referred participants, present higher IPV recidivism rates (Mills et al., 2013; Shepard et al., 2002), higher social desirability and denial (Daly et al., 2001), are more antisocial (Dixon & Browne, 2003; Turner et al., 2022), exhibit higher levels of external locus of control, and are less motivated to change (Bowen & Gilchrist, 2004), also shown by their increased likelihood to be in the precontemplation stage (Tutty et al., 2020). Therefore, those referred by the judicial system to attend interventions for IPV perpetrators may require more tailored support to address risk factors that contribute to increasing their resistance to treatment (Cheng et al., 2021; Cunha et al., 2022; Tutty et al., 2020). However, more research is needed to provide an integrated view of the main risk factors present in court-mandated IPV perpetrators with ADUPs.
The present systematic review filled this gap by rigorously analyzing the specific risk factors in men with and without ADUPs court-mandated to attend intervention programs for IPV perpetrators. Although there are other types of partnerships that involve IPV (e.g., LGBTIQ+; Badenes-Ribera et al., 2016; Coston, 2021; Gilchrist et al., 2023; Liu et al., 2021; Peitzmeier et al., 2020), the present systematic review focuses on male perpetrators, as IPV is most commonly and severely perpetrated by men against women (Centers for Disease Control and Prevention [CDC, 2022]; WHO, 2013). As far as we are aware, this is the first systematic review to identify the specific risk factors beyond issues strictly related to substance use that differentiate IPV perpetrators with and without ADUPs in court-mandated group-based intervention programs for IPV perpetrators. A better understanding of the main risk factors present in participants with ADUPs on entry to such programs will help inform intervention needs for this high-risk, highly resistant population, which may improve their treatment outcomes (Crane et al., 2016; Massa et al., 2020).
Method
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021). The study protocol was prospectively registered with the International Prospective Register of Systematic Reviews (PROSPERO 2022 CRD42022297377) on 13 January 2022.
Search Strategy
A systematic search of the following electronic databases was conducted: Web of Science, PsycINFO, and Scopus. The search strategy on terms related to IPV was developed by the research team and adapted from a previous review conducted by the team (Santirso et al., 2020). No limitation was applied for the year or language of publications. Citations were managed using Endnote Version X9. The search was conducted in October 2020 and repeated in November 2021. The search strategy was performed through an iterative process using multiple combinations of the keywords in four clusters and included the following terms: (intimate* violen* OR partner* violen* OR domestic* violen* OR marital* violen* OR couple* violen* OR spous* violen* OR husband* violen* OR situation* violen* OR partner* abus* OR domestic* abus* OR spous* abus* OR marital* abus* OR husband* abus* OR intimate* terror* OR partner* aggress* OR husband* aggress* OR spous* aggress* OR marital* aggress* OR couple* aggress*) AND (alcohol* OR substance OR drug OR drinking) AND (intervention* OR program* OR treatment* OR therapy* OR group) AND (batterer* OR offender* OR perpetrator* OR aggres* OR men). We complemented the electronic search with backward and forward searches to further identify relevant publications.
Eligibility
Inclusion criteria were: (1) studies published in peer-reviewed journals to guarantee minimum methodological standards in the included studies; 2) quantitative studies; 3) sample included at least 70% men who were court-mandated to attend an intervention program for IPV perpetrators; 4) results were presented separately for men; 5) risk factors for IPV (e.g., levels of anger) were compared between IPV perpetrators with and without ADUPs and/or levels of ADUPs were compared between IPV perpetrators with and without risk factors for IPV (e.g., participants with high versus low anger) and/or the association between risk factors and levels of ADUPs was evaluated; 6) data were collected on entry to court-mandated IPV perpetrator intervention. Two reviewers (CEA and FA) independently screened the records by abstract and title to identify studies that met eligibility criteria. Full texts of the selected studies were independently assessed by three authors (CEA, FA, and GG) and discrepancies were resolved by discussion and consensus with additional authors (ML and EG). When we needed further clarification to establish eligibility or supply additional data required for our review, the authors of the studies were contacted by email.
Data Extraction
Two of the researchers independently extracted the data (CEA and FA). Study characteristics that were extracted included the country where each intervention took place, their sample size, % of men court-mandated to attend an intervention program for IPV perpetrators, methodology, ADUPs-related measures, risk factors-related measures, and a summary of the main results showing the risk factors in IPV perpetrators with ADUPs. The extracted data included a summary of documented risk factors for IPV in perpetrators with and without ADUPs analyzed in included studies, the number of included studies that assessed at least one risk factor in each category, and the number of included studies that investigated each risk factor. Discrepancies were resolved by consensus with a third author (GG or ML).
Assessment of Methodological Quality
Study quality was assessed using the Mixed Methods Appraisal Tool (MMAT; Hong et al., 2018; Pace et al., 2012). Specifically, the designs evaluated were non-randomized quantitative studies. For each study design, the MMAT presents a five-question checklist to assess the methodological quality of the studies. The response options were ‘yes’, ‘no’, or ‘can’t tell’ if the study does not report appropriate information to answer. Three authors (CEA, FA, and GG) independently assessed the risk of bias in included studies with disagreement resolved by discussion and consensus with additional authors (ML and EG).
Results
Database searches resulted in 6,053 records. Once duplicates were removed, 3,995 records remained. After initial exclusion based on titles and abstracts, 53 records were selected for full-text assessment. Twenty-four studies were excluded as: they were not quantitative studies (n = 2); the target population was less than 70% men court-mandated to an intervention program for IPV perpetrators (n = 10); the results were not presented separately for men (n = 3); comparisons of risk factors for IPV between IPV perpetrators with and without ADUPs, comparisons of levels of ADUPs between IPV perpetrators with and without risk factors, or associations between risk factors and ADUPs were not available (n = 7) and the data collected on entry to IPV perpetrator program were not presented (n = 2). A total of 29 manuscripts met the inclusion criteria and were included in the review (Figure 1).
Risk of Bias Results
Risk of bias in included studies was assessed, using MMAT criteria for quantitative non-randomized studies (n = 29; see Figure 2). In terms of the representativeness of the target population, only seven studies gave clear indicators, including inclusion and exclusion criteria of the target population and reasons why certain eligible individuals chose not to participate (Studies 2, 9, 10, 12, 14, 22, and 26). Measurements were appropriately described in all studies (see Figure 2). With regard to complete outcome data, most of the studies (n = 22) gave all numbers and accounted for missing data, except for seven studies, six of which only met one of these conditions (Studies 1, 4, 7, 11, 24, and 29), and one which did not mention missing data (Study 5). Unexpected or inappropriate methods were used to control for confounding factors in six studies (Studies 1, 2, 8, 10, 19, and 27). In terms of the presence of contamination in the assignment of the intervention, the intervention was not administered as intended in two studies (Study 2, 3), and one study used a sample recruited from domestic violence programs in several communities (Study 8). All studies were included in the narrative synthesis regardless of quality.
Study Characteristics
Twenty-nine studies reported data for 8,893 male perpetrators attending intervention programs for IPV perpetrators. As shown in Table 1, most studies were conducted in the USA (n = 14; Studies 1, 3, 4, 5, 8, 9, 11, 14, 20, 21, 23, 24, 25, and 29) and Spain (n = 13; Studies 2, 6, 7, 10, 12, 15 to 19, 22, 27, and 28). One study was conducted in New Zealand (Study 13) and one in Ireland (Study 26). Samples sizes ranged from 16 IPV perpetrators (Study 17) to 1,039 (Study 10). In 24 of the 29 studies, the total sample of adult males was court-mandated to attend an intervention program for IPV perpetrators (Studies 1 to 7, 9 to 13, 15 to 19, and 23 to 29). In the remaining studies (Studies 8, 14, 20, 21, and 22) and in accordance with the inclusion criteria for the study selection, the lowest percentage of court-mandated participants was 70% (Study 20). In addition, while the majority of included studies explicitly clarified that participants were men who perpetrated IPV against women (IPVAW) or mentioned IPVAW as the theoretical framework of the study (n = 25; Studies 1 to 10, 12, 14 to 20, and 22 to 28), four studies did not clarify the male IPV perpetrators’ sexual orientation (Studies 11, 13, 21, and 29).
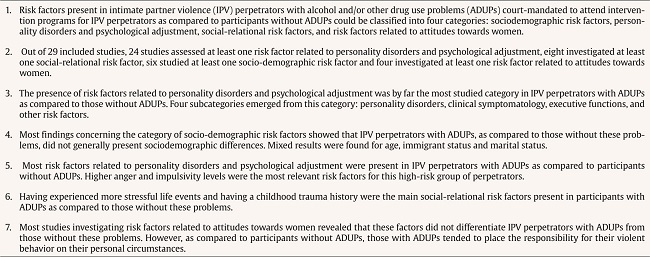
Table 1. Risk Factors in Intimate Partner Violence (IPV) Perpetrators with Alcohol and/or other Drug Use Problems (ADUPs) in the Selected Studies.

Table 1 (cont). Risk Factors in Intimate Partner Violence (IPV) Perpetrators with Alcohol and/or other Drug Use Problems (ADUPs) in the Selected Studies.

Table 1 (cont). Risk Factors in Intimate Partner Violence (IPV) Perpetrators with Alcohol and/or other Drug Use Problems (ADUPs) in the Selected Studies.

Table 1 (cont). Risk Factors in Intimate Partner Violence (IPV) Perpetrators with Alcohol and/or other Drug Use Problems (ADUPs) in the Selected Studies.
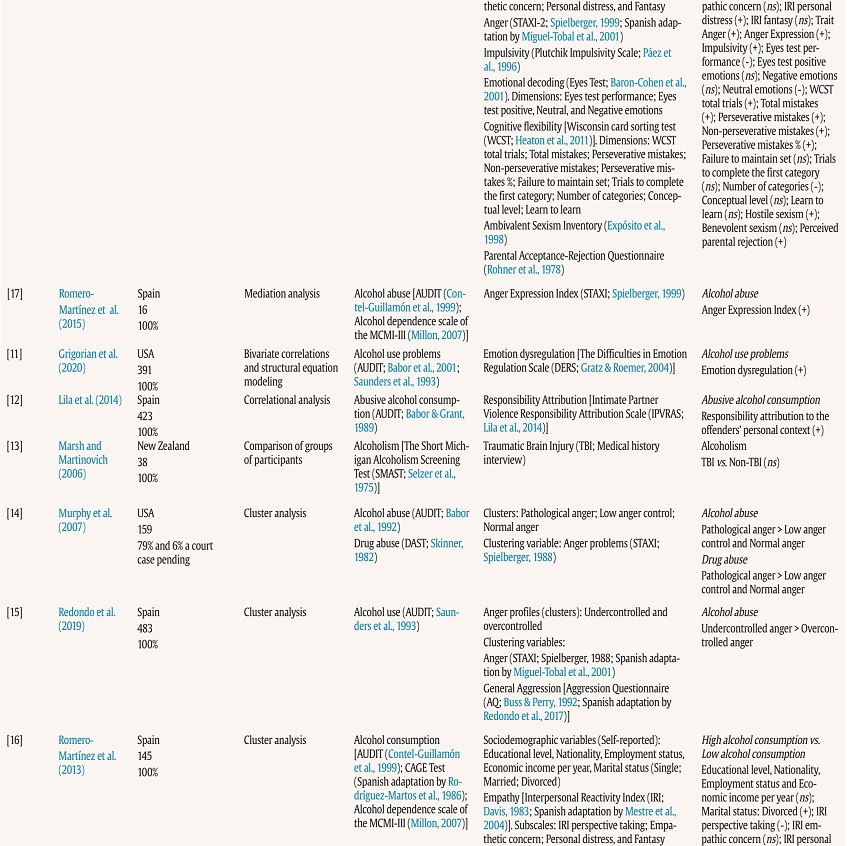
Table 1 (cont). Risk Factors in Intimate Partner Violence (IPV) Perpetrators with Alcohol and/or other Drug Use Problems (ADUPs) in the Selected Studies.

Table 1 (cont). Risk Factors in Intimate Partner Violence (IPV) Perpetrators with Alcohol and/or other Drug Use Problems (ADUPs) in the Selected Studies.

Note.(+) = significantly higher/statistically significant positive association; (-) = significantly lower/statistically significant negative association; ns = non-significant association/differences; vs. = versus; > = significantly greater than; < = significantly less than.
Risk Factors in Perpetrators Court-mandated to Intervention Programs for IPV perpetrators with and without ADUPs
Table 2 displays a summary of investigated risk factors grouped into four main categories: (1) sociodemographic variables, (2) personality disorders and psychological adjustment, (3) socio-relational variables, and (4) attitudes towards women. Risk factors related to personality disorders and psychological adjustment were grouped into four subcategories: (2.1) personality disorders, (2.2) clinical symptomatology, (2.3) executive functions, and (2.4) other risk factors. The number of studies investigating each risk factor is presented separately for participants with alcohol and other drug use problems in Table 2. Where studies measured alcohol and other drug use conjointly (Studies 10, 25, and 26), results were included in both columns for IPV perpetrators with alcohol use problems and for IPV perpetrators with other drug use problems.
Table 2. Summary of Risk Factors in Intimate Partner Violence (IPV) Perpetrators with Alcohol and/or other Drug Use Problems (ADUPs) Analyzed in Identified Studies.
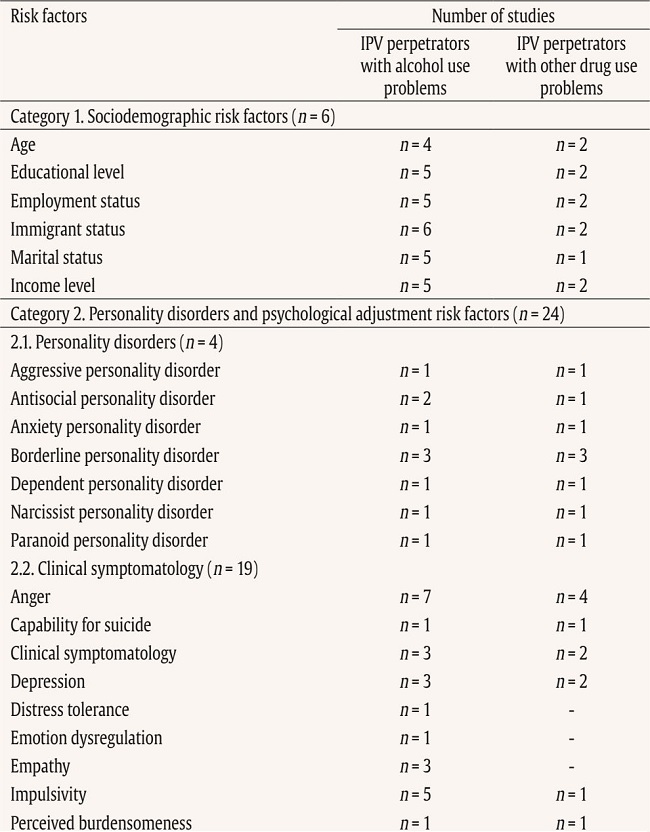
Table 2 (cont.). Summary of Risk Factors in Intimate Partner Violence (IPV) Perpetrators with Alcohol and/or other Drug Use Problems (ADUPs) Analyzed in Identified Studies.

Sociodemographic Risk Factors
Sociodemographic risk factors were examined in six of the 29 included studies (see Table 2; Studies 7, 10, 16, 18, 25, and 28). Overall, most studies reported non-significant differences in sociodemographic risk factors between IPV perpetrators with and without ADUPs, except for age, immigrant status, and marital status, which showed mixed results (see Table 3 for a summary of critical findings).
Immigrant status was the most studied risk factor in this category. Three of the six studies showed non-significant differences in terms of immigrant status when comparing IPV perpetrators with and without ADUPs ([Studies 16, 18, and 28]; see Table 1). However, when assessing only Latin American IPV perpetrators in Spain, Study 7 found that being Latin American was a risk factor present in IPV perpetrators with hazardous alcohol consumption compared to non-hazardous alcohol consumption. Other studies reported that IPV perpetrators with ADUPs had a significantly lower prevalence of immigrant participants in Spain (Study 10) and a higher prevalence of Latino and white participants in the USA than IPV perpetrators without ADUPs (Study 25). Age, which was the least studied risk factor in this category (n = 4), and marital status (n = 5) also showed mixed results within studies. Some studies reported no differences between groups in terms of age (Studies 7 and 28) or marital status (Studies 7, 25, and 28). Others showed that significantly greater proportions of perpetrators with ADUPs were older (Study 25), younger (Study 10), divorced (Study 16), and single than those without ADUPs (Study 18).
Most of the studies showed that participants with and without ADUPs were not significantly different in terms of employment status, income, and educational level (Studies 10, 16, 18, 25, and 28). Only one study showed that IPV perpetrators with ADUPs had significantly fewer years of education compared to those without (Study 25) and another reported a higher rate of unemployment among IPV perpetrators with ADUPs compared to those without (Study 10; see Table 1).
Personality Disorders and Psychological Adjustment Risk Factors
The most investigated risk factors were those related to the category of personality disorders and psychological adjustment, which were assessed in 24 out of 29 included studies. When considering subcategories, four studies investigated at least one risk factor related to personality disorders, 19 studies assessed at least one clinical symptomatology risk factor, five studies analysed at least one risk factor related to executive functions, and seven studies investigated other risk factors related to personality disorders and psychological adjustment in IPV perpetrators. Overall, the most salient risk factors related to personality disorders and psychological adjustment in IPV perpetrators with ADUPs, compared to those without ADUPs, were higher anger and impulsivity levels (see Table 3).
Personality Disorders. With regard to personality disorders, the most studied risk factor was borderline personality disorder (n = 3). Included studies found that IPV perpetrators with ADUPs showed significantly higher levels of borderline personality traits (Studies 10, 25, and 29) and higher levels of antisocial (Studies 4 and 10), aggressive, anxiety (i.e., a term coined by Millon, 2007 as a clinical personality pattern which refers to a sadistic tendency to react impulsively and violently, seeking risk and harm and resisting pain and punishment), narcissist, and paranoid personality disorders in IPV perpetrators with ADUPs (Study 10). No differences were reported regarding dependent personality disorder in IPV perpetrators with and without ADUPs (Study 10).
Clinical Symptomatology. The most investigated risk factors in the subcategory of clinical symptomatology were anger (n = 7) and impulsivity (n = 5; see Table 2). All studies investigating these risk factors consistently reported higher impulsivity, and anger including anger trait, anger state, and anger expression in IPV perpetrators with ADUPs compared to those without (Studies 3, 6, 9, 10, 14 to 17, 19, and 25).
IPV perpetrators with ADUPs court-mandated to attend intervention programs for IPV showed significantly higher levels of clinical symptomatology, including depression, than participants without ADUPs(Studies 2, 6, 10, 24, and 29).
Risk factors related to suicide ideation were studied in Study 29. Results were consistent among IPV perpetrators with alcohol use problems and those with drug use problems in terms of higher levels of suicide ideation, perceived burdensomeness, thwarted belongingness, and capability for suicide than IPV perpetrators without alcohol and drug use problems. However, only participants with drug use problems reported differences in terms of suicide attempt history, with a higher prevalence in these participants than those without drug use problems (Study 29; see Table 1).
The three studies that investigated empathy (Studies 16, 18, and 28) found that IPV perpetrators with high alcohol consumption had a significantly lower score in perspective taking than the group with low alcohol consumption and no differences between groups in empathic concern and fantasy. Personal distress was higher in the group of high alcohol consumers compared to the group of low alcohol consumers in two studies (Studies 16 and 18) and non-significant differences were found between groups in another study (Study 28).
Compared to IPV perpetrators without ADUPs, court-mandated perpetrators with ADUPs showed significantly lower levels of distress tolerance (Study 4), self-esteem (Studies 6 and 10), higher levels of emotion dysregulation (Study 11), and trauma/ posttraumatic stress disorder (PTSD) symptoms (Studies 21 and 25). Particularly, PTSD hyperarousal symptoms were a risk factor when considering IPV participants who used drugs but not alcohol (Study 21; see Table 1).
Executive Functions. Mental rigidity (n = 4) and emotional decoding performance (n = 3) were the most studied risk factors in this subcategory. Mental rigidity was a risk factor present in IPV perpetrators with high alcohol consumption compared to those with low alcohol consumption, which when it is high refers to deficient flexibility in self-regulated behavior (Study 27). Further, those with high, compared to low, alcohol consumption needed significantly more attempts in the Wisconsin Card Sorting Test (WCST; Heaton et al., 2011; Studies 16 and 18), which measures cognitive flexibility, and made more mistakes (Study 16), more perseverative mistakes (Studies 16, 18 and 19), more non-perseverative mistakes (Study 16) and lower number of categories completed (Studies 16 and 18). Non-significant differences were found between groups in failure to maintain set, trials to complete the first category, conceptual level, and learn-to-learn subscales (Study 16). Overall, these findings showed that IPV perpetrators had higher mental rigidity than those without.
Emotional decoding performance, understood as the process of recognizing and interpreting emotional facial expressions, was worse for high than low alcohol consumers across studies (Studies 16, 18, and 19). As shown in Table 1, Study 16 studied whether emotional decoding of neutral, positive, and negative emotions was different in the group of high and low alcohol consumption. Emotional decoding performance was worse for neutral emotions in high alcohol consumers and showed non-significant differences between high and low consumers for positive and negative emotions (Study 16).
When comparing higher versus low alcohol consumers, IPV perpetrators with high alcohol consumption showed a significantly higher cost of shifting attention, which refers to a lack of flexibility to shift the attentional focus, and, in terms of frontal behaviour, higher executive dysfunction, and disinhibition, which describe an alteration of the normal functioning of cognitive processes necessary for the regulation of behavior (Study 28).
Other Risk Factors. Study 23 showed that IPV perpetrators with problem drinking reported higher levels of avoidance coping, lower levels of problem-solving, and no differences in support-seeking coping compared to those without problem drinking. With regard to pathological gambling, IPV perpetrators with hazardous drinking, compared to those without, showed higher levels of pathological gambling (Study 3).
Two studies investigated differences between typologies of IPV perpetrators with regard to alcohol use (Studies 8 and 20). In Study 20, IPV perpetrators with alcohol use were more ‘generally violent’. This type of perpetrator was the most likely to be violent towards non-partners, having experienced abuse as a child, reported low or moderate levels of depression and anger, more frequent severe violence, and their violence was usually associated with alcohol abuse (Study 20). However, Study 8 showed non-significant findings. Non-significant differences were also recorded between IPV perpetrators with and without alcohol use problems with regard to temporary loss of consciousness (Study 28), history of traumatic brain injury (Studies 13 and 28), and trait jealousy (Study 5). However, alcohol problems were significantly and positively related to physical and sexual IPV perpetration by men with high levels of trait jealousy (Study 5).
Social-relational Risk Factors
As shown in Table 2, social-relational risk factors were investigated in eight of the 29 studies. The most studied and salient social-relational risk factors present in IPV perpetrators with ADUPs as compared to those without ADUPs were having experienced more stressful life events (n = 4) and childhood trauma history (n = 4; see Table 3). These findings were consistent across studies (Studies 1, 6, 7, 10, 22, 25, and 26). Only one study reported that exposure to childhood trauma was not a risk factor present in IPV perpetrators who used drugs but was present for those who used alcohol (Study 1; see Table 1).
In terms of social support, perpetrators with ADUPs showed lower levels of intimate support across studies (Studies 6, 7, and 10). However, mixed results were found for perceived community integration, community participation, and informal community support, with significantly higher levels among IPV perpetrators with ADUPs versus those without ADUPs in Study 10 and no differences between groups in Study 6. Mixed results were also found for perceived social rejection, with one study showing higher levels for participants with alcohol abuse than those without (Study 6) and other study reporting no differences between groups (Study 7).
Further, higher levels of perceived parental rejection (Study 16) and satisfaction with economic status (Study 6) were found for IPV perpetrators with high alcohol consumption versus low alcohol consumption.
Risk Factors Related to Attitudes towards Women
As shown in Table 2, risk factors related to attitudes towards women were the least studied category, with four studies investigating at least one risk factor relating to attitudes towards women. Overall, the main risk factor in this understudied category was responsibility attributed to the offenders’ personal context, which showed that participants with ADUPs tended to place the responsibility for their violent behaviour on their personal circumstances (see Table 3).
IPV perpetrators with ADUPs did not differ from those without ADUPs in attitudes towards IPV against women (Studies 6 and 10), responsibility attributed to the legal context and the victim (Study 6), and hostile (Study 10) and ambivalent sexism (Studies 10 and 16).
However, hostile sexism was found to be a risk factor present in participants with high alcohol consumption compared to those with low alcohol consumption in Study 16. Moreover, responsibility attributed to the offenders’ personal context was a risk factor identified in IPV perpetrators with ADUPs as compared to those without ADUPs in both studies investigating this risk factor (Studies 6 and 12).
Discussion
This review provides a synthesis of existing literature, which suggested that overall, compared to those without ADUPs, IPV perpetrators with ADUPs who were court-mandated to attend perpetrator intervention programs were more likely to exhibit higher levels of personality disorders, including borderline, antisocial, aggressive, anxiety, narcissist, and paranoid personality disorders, and higher clinical symptomatology, including higher anger, impulsivity, depression, suicide risks, emotion dysregulation, trauma symptoms, and lower empathetic perspective-taking, distress tolerance and self-esteem. Compared to participants without ADUPs, those with ADUPs appeared to present poorer executive functions, including lower emotional decoding performance, higher mental rigidity, cost of shifting attention and greater executive dysfunction and disinhibition. Greater pathological gambling and poorer coping strategies were also found in this group of perpetrators.
The review also found IPV perpetrators with ADUPs, compared to those without ADUPs, were more likely to have experienced exposure to childhood trauma, stressful life events, satisfaction with economic status, perceived parental rejection, and lower intimate social support. In addition, compared to participants without ADUPs, those with ADUPs tended to display higher responsibility attributed to the offenders’ personal context. Inconsistent findings were observed for empathetic personal distress, typologies, perceived community support, perceived social rejection, hostile sexism, and several socio-demographic variables.
Socio-demographic Risk Factors
Evidence from included studies found mixed results for age, immigrant status, and marital status. Mixed findings on immigration could be explained by the immigration paradox, which suggests that recent immigrants may report lower substance use and IPV due to factors such as stronger family ties or cultural norms that discourage such behaviors (Salas-Wright & Vaughn, 2014; Wright & Benson, 2010). However, as immigrants settle in the receiving country and face acculturative stress, their risk for IPV and substance use may increase (Bacio et al., 2013; Gracia et al., 2009; Vaughn et al., 2015). In addition, our findings seemed to show that educational level, employment status, or income level were not consistently considered risk factors that characterized IPV perpetrators with ADUPs compared to those without ADUPs. Research suggests that alcohol and drug use may generate higher financial pressures in perpetrators’ domestic contexts, which in turn may intensify partner conflict (Gadd et al., 2019). In these economic disadvantage situations, IPV perpetrators may feel shame as they are failing to fulfil the normative masculine role of being the provider, which could feed their desire for control and power (Gadd et al., 2019; Radcliffe et al., 2019). However, more research is required to investigate how sociodemographic context and other sociocultural factors (e.g., the country’s economic situation, cultural patterns of alcohol use, and the role of masculinity on substance use) impact IPV perpetrators with ADUPs.
Personality Disorders and Psychological Adjustment Risk Factors
The most salient risk factors found in this broad category were anger and impulsivity. Similar to other studies (Oberleitner et al., 2013; Winters, 2005), we found higher levels of anger in IPV perpetrators with ADUPs compared to those without in the studies included in this review. This group of IPV perpetrators were also at higher risk of recidivism and needed more intensive interventions (Oberleitner et al., 2013). One possible explanation underlying these findings could be that IPV perpetrators high in anger may seek alcohol and/or drugs to mitigate their intense and overwhelming emotional reactions (Oberleitner et al., 2013). Another possible explanation could be that substance use may disrupt neurocognitive resources involved in self-regulation, thus increasing the likelihood of IPV (Giancola et al., 2003). Relatedly, alcohol intoxication may act as a disinhibitor in accordance with the I3 model (Finkel & Eckhardt, 2013) and as stated by the Alcohol Myopia Theory (Steele & Josephs, 1990). Intoxication may disrupt normal cognitive processing resulting in a myopic effect where only the most salient stimuli (such as the instigating, and impelling forces in line with the I3 model) are kept over cues that may inhibit IPV (such as inhibiting forces). These results highlight the importance of developing effective intervention strategies for this high-risk group of IPV perpetrators. For example, a systematic review conducted by Gilchrist et al. (2015) of the effectiveness of cognitive behavioural therapy with anger management components for IPV perpetrators who used alcohol showed promising results in the short term and suggested that more research is needed to match this group of IPV perpetrators with specific intervention programs that address their individual needs. Enhancing distress tolerance for perpetrators who use substances has been shown to promote positive behaviour change and skills development (Gilchrist, Johnson, et al., 2021; Gilchrist, Potts, et al., 2021).
Previous studies also observed higher levels of impulsivity among IPV perpetrators with ADUPs (Easton et al., 2008; Stuart & Holtzwroth-Munroe, 2005). A meta-ethnography conducted by Gilchrist et al. (2019) on the interplay between substance use and IPV perpetration showed that survivors and perpetrators both explained IPV perpetration when under the influence of alcohol and other drugs referring to a change in self, as they used narratives in which intoxication transforms an idealized real self into an aggressive and impulsive non-real one. Further efforts are thus needed to develop effective strategies targeted at helping IPV perpetrators increase responsibility and awareness of their anger and impulsivity levels. For instance, a study conducted by Finkel et al. (2009) showed that two weeks of self-regulatory-based activities, such as training perpetrators to recognize internal signs of anger and impulsivity, reduced IPV perpetration in participants with low self-regulatory resources.
Other salient, identified risk factors in IPV perpetrators with ADUPs were, in terms of personality disorders, a trend towards higher scores on antisocial and borderline personality disorders, in terms of clinical symptomatology, higher clinical symptomatology, depression, and trauma symptomatology and, in terms of executive functions, higher mental rigidity. According to Gilchrist et al. (2022), one of the pathways into substance use-related IPV revealed that perpetrators reported using substances as a coping mechanism to help them deal with their emotional pain and mental health issues caused by unresolved previous trauma. Similarly, the self-medication hypothesis states that individuals with PTSD are more likely to develop ADUPs in light of a tendency to drink or use drugs to alleviate PTSD symptoms and cope with difficult internal experiences (Hawn et al., 2020; Khantzian, 1997; Lawrence et al., 2023). These findings underscore the need to address the function of substance use in intervention programs for IPV perpetrators with ADUPs. Effective interventions with this high-risk group of perpetrators should focus on re-scripting childhood experiences, reframing unhelpful schemas, and expressing emotional needs to enhance self-regulation and trauma healing (Gilchrist et al., 2022). However, as IPV perpetrators with ADUPs present high dropout and recidivism rates, retention strategies are also needed to help them complete the intervention and improve their outcomes (Lila et al., 2020; Olver et al., 2011). Based on the ‘what works’ body of knowledge, incorporating motivational strategies has proven effective in increasing treatment engagement and reducing dropout rates in high-risk IPV perpetrators (Santirso et al., 2020). However, further research is needed to ascertain whether the positive effects of motivationally focused alcohol interventions as adjuncts to court-mandated intervention programs for IPV perpetrators are sustained in the long term (i.e., > 6 months post-intervention; Stuart et al., 2013).
Social-relational Risk Factors
Consistent with other studies (Rivas-Rivero & Bonilla-Algovia, 2022; Schumacher et al., 2008), stressful life events, a history of childhood trauma, and lower intimate support seemed to be associated with IPV perpetration among IPV perpetrators with ADUPs. These risk factors should be specifically targeted in interventions for IPV perpetrators as they have been shown to increase the likelihood of IPV recidivism (Kwong et al., 2003; Lila et al., 2019; López-Ossorio et al., 2021). Previous research suggests that unresolved trauma in IPV perpetrators could have an impact on ADUPs (e.g., substance use can be used as a way of coping with stress and trauma) and on intimate relationships by intensifying IPV perpetration (Gilchrist et al., 2019; Mathews et al., 2015). Specifically, IPV perpetrators who disclosed childhood trauma experiences could be perpetrating IPV and using drugs as a defence to regain control and power over their lives (Gilchrist et al., 2022; Øverup et al., 2015). These findings evidence the fact that exploring the history of trauma of IPV perpetrators with ADUPs and their narratives could inform interventions and improve outcomes. In this line, a meta-analysis and systematic review by Karakurt et al. (2019) showed that including trauma-based or substance-use treatment components yielded better outcomes than interventions without this component, as they reported more effective results in decreasing male IPV perpetration. Interventions targeting anti-social cognitions and schemas that sustain their use of violence while promoting intimate and network support could also be helpful (Gilchrist et al., 2022).
Risk Factors Related to Attitudes towards Women
In accordance with previous research, IPV perpetrators tend to use ADUPs and other personal circumstances (i.e., economic problems, loss of control) as an excuse for their violent behaviour during conflict (Gilchrist et al., 2019; Radcliffe et al., 2017). Further research is needed to deeply comprehend how traditional gender norms, victim-blaming attitudes, and the normalization of violence toward women play a role in men’s ADUPs to justify their IPV perpetration (Martín-Fernández, Gracia, & Lila, 2018, 2022; Satyanarayana et al., 2015).
Interventions should work on reframing gender ideals and changing attitudes regarding normative gender roles that sustain IPV perpetration (Gilchrist et al., 2019; Martín-Fernández, Gracia, Marco, et al., 2018). For example, a cluster randomised controlled trial in the Democratic Republic of Congo showed that men in a male-only discussion group focused on challenging gender attitudes and reducing IPV reported greater reductions in intention to commit IPV, justification of IPV, and partner-reported frequency of drinking than the control group, where men participated in non-gender norms-related alternative group sessions (Vaillant et al., 2020). More evidence-based strategies are needed to target gendered power dynamics in intervention programs for IPV perpetrators.
Implications For Research, Practice and Policy
Implications for research, practice and policy are presented in Table 4. The results of this systematic review highlight the importance of screening and identifying a wide range of risk factors in IPV perpetrators with ADUPs structured at different levels. It is essential to develop or improve intervention programs for IPV perpetrators based on the specific needs and identified risk factors of this highly resistant group of perpetrators (Finkel, 2007; Karakurt et al., 2019; Massa et al., 2020). Consistent with the risk-needs-responsivity (RNR) model (Andrews & Bonta, 2010), which strives for adapting intervention programs for IPV perpetrators to individual participant’s specific needs and matching intervention strategies based on risk factors, there is a “need for more individualized approaches to perpetrator treatment that emphasize assessment, motivation enhancement, and interventions targeting mental health and substance use” (Butters et al., 2021, p.399). For example, motivational strategies such as setting self-determined goals to establish and monitor individualized intervention objectives, including those related to ADUPs and identified risk factors (e.g., “reducing my anger levels during partner conflict”) have shown promising results in intervention programs for IPV perpetrators (Lila et al., 2018; Pinto e Silva et al., 2022; Santirso et al., 2020). To further address identified risk factors, for instance, a trauma-informed approach would be recommended for IPV perpetrators with co-occurring ADUPs, a history of childhood trauma and psychological symptomatology (Gilchrist et al., 2019; Karakurt et al., 2019; McKenna & Holtfreter, 2020). Similarly, assessing and identifying each participant’s risk factors could help facilitators develop concrete exercises adapted to IPV perpetrators’ needs (Leonard & Quigley, 2017; Massa et al., 2020). For example, those perpetrators with higher levels of aggressive or antisocial personality disorder could benefit from completing exercises that provide information and reflection on healthy relationships, and that helps them to realise that their aggressive behaviours damage their potential to meet their own needs (Babcock et al., 2016). Overall, monitoring identified risk factors and implementing evidence-based practices that address them could improve participants’ outcomes and help to reduce IPV perpetration. Finally, public funding should be attributed to intervention programs for IPV perpetrators that address documented risk factors for high-risk perpetrators with ADUPs. Global social policies aiming to prevent IPV perpetration (e.g., prevention initiatives focused on reducing tolerant attitudes towards violence against women), ADUPs, and their associated risk factors while promoting mental health are also crucial.
Strengths and Limitations
This systematic review was conducted using PRISMA guidelines (Page et al., 2021), and, to our knowledge, it is the first systematic review to identify risk factors beyond substance use in IPV perpetrators with ADUPs court-mandated to attend intervention programs for IPV perpetrators. Furthermore, a wide range of risk factors was identified and structured at multiple levels, which contributes to a deeper understanding of the complex phenomenon of IPV and ADUPs and informs key intervention targets that could encourage treatment engagement and improve participants’ outcomes and safety for women and children.
The present systematic review has certain limitations. Included studies used heterogeneous methodologies to study risk factors in IPV perpetrators with ADUPs compared to those without ADUPs (e.g., multiple regression, path analysis). This review is also limited by its lack of systematic searching of the grey literature. It is acknowledged that this could have led to a potential source of bias in the findings (Petticrew & Roberts, 2006). In addition, several studies defined and measured ADUPs (e.g., alcohol abuse, alcohol consumption, drug abuse) and some risk factors differently (e.g., borderline personality disorder; see Table 1). Furthermore, some of the results should be interpreted cautiously when only a few studies assessed a risk factor (e.g., only one study assessed suicide ideation). More studies are needed to add knowledge to these least-studied risk factors. Furthermore, the existing literature does not allow us to conclude which of the variables that interact with ADUPs potentiate IPV, so attention should be paid to the complexity of this relationship. Future reviews would also benefit from including a meta-analysis component to quantify the size of the findings. Further research is also needed to study risk factors present in women and other gender and sexual minorities (i.e., LGBTIQ+) to reduce heteronormative bias. These limitations should be considered when interpreting the results.
Conclusion
Men with ADUPs who are court-mandated to attend intervention programs for IPV perpetrators present with more complex social and mental health needs than men without ADUPs resulting in higher dropout and recidivism rates. This review has identified key risk factors in male IPV perpetrators with ADUPs that can be translated into important intervention targets beyond their substance use. Tailoring such interventions to participants’ risk factors and treatment needs has shown promising results over standard interventions (Travers et al., 2021). Thus, integrating substance use components while implementing evidence-based strategies to reduce identified, associated risk factors could improve intervention outcomes and increase their effectiveness for perpetrators with ADUPs (Karakurt et al., 2019; Leonard & Quigley, 2017). A greater understanding of the risk factors that underlie IPV and ADUPs will inform researchers, professionals and policymakers of the main factors that should be targeted to reduce IPV and promote healthy relationships.