Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de la Sociedad Española del Dolor
versión impresa ISSN 1134-8046
Rev. Soc. Esp. Dolor vol.26 no.5 Madrid sep./oct. 2019 Epub 23-Mar-2020
https://dx.doi.org/10.20986/resed.2019.3700/2018
ORIGINALS
Epidural betamethasone injection in lumbosacral radicular syndrome: effi cacy evaluation for interlaminar and transforaminal approaches
1Profesor Agregado. Servicio de Terapia del Dolor. Departamento y Cátedra de Anestesiología. Hospital de Clínicas. Montevideo, Uruguay.
2Profesor Adjunto. Servicio de Terapia del Dolor. Departamento y Cátedra de Anestesiología. Hospital de Clínicas. Montevideo, Uruguay.
3Anestesiólogo. Servicio de Terapia del Dolor. Departamento y Cátedra de Anestesiología. Hospital de Clínicas. Montevideo, Uruguay.
4Asistente. Servicio de Terapia del Dolor. Departamento y Cátedra de Anestesiología. Hospital de Clínicas. Montevideo, Uruguay.
Introduction:
Betamethasone is a frequently used steroid for epidural injection, recently incorporated in the Uruguayan pharmaceutical market.
Aims:
The aim of this study is to evaluate the efficacy of parasagittal interlaminar and transforaminal epidural betamethasone in unilateral lumbosacral radicular syndrome, utilizing the Brief Pain Inventory (BPI).
Material and method:
Is a prospective study comparing parasagittal interlaminar and transforaminal epidural betamethasone. Patients with chronic unilateral lumbosacral radicular pain were included. The BPI was administered before and one month after epidural injections. Pain intensity was measured by the Visual Numeric Scale (VNS, question 6 of the BPI) and the Intensity Score. Interference of pain in daily activities was measured by the Interference Score. Satisfactory responses to injections were considered with a 2 points reduction in VNS. The statistical evaluation was performed by paired an unpaired T test to continuous data and Chi Square to evaluate proportions. A p value less than 0.05 was considered statistically significant.
Results:
Fifty four patients were treated with epidural betamethasone. In 29 the parasagittal interlaminar route was utilized while 25 were treated by the transforaminal route. A 20 % reduction in baseline VNS was observed with the interlaminar route and 36 % reduction with transforaminal approach. Intensity and Interference Scores were also reduced. This reductions were statistically significant when comparing to baseline data (paired t test) but differences between groups were not significant (unpaired t test). However the number of positive responses as defined above was greater in the transforaminal group, 64 % versus 38 % in the interlaminar group, statistically significant difference using the Chi Square analysis (p=0.01).
In patients with positive responses, interlaminar and transforaminal betamethasone produce clinical and statistically significant reductions in pain intensity and interference, without difference between groups.
Conclusion:
Epidural betamethasone produced a reduction in pain intensity and interference utilizing the BPI, by the two routes utilized to access the epidural space. Although no statistically differences were observed in this reductions between groups, the frequency of positive responses were higher when the drug is administered by the transforaminal route. Epidural interlaminar parasagittal betamethasone injection is a reasonable alternative to the transforaminal route, without the neurologic complications described utilizing this technique.
Key words: Epidural steroid injections; lumbar radicular pain; betamethasone
INTRODUCTION
The epidural steroid injection is one of the procedures that we used with more frequency in the treatment of the lumbar radicular pain in our service 1. Betamethasone is a steroid of wide use for epidural application in the world, of recent incorporation to the vade mecum of our country 2,3,4.
The steroid injection in the epidural space is performed more frequently through the interlaminar or transforaminal routes 5. Scientific evidences of which approach is more effective than the other are not available, although there is the perception that the transforaminal route obtains better results because it concentrates more steroid in the disc-radicular conflict zone 6,7. In spite of this, it is known that the route involves a higher potential risk of neurological injuries, caused by medullary ischemia secondary to injury of the radiculomedullary artery. This injury has been associated with vascular spasm or vascular occlusion; the latter could be related to the size of particles of the injected steroid 8. In this sense, betamethasone is the steroid that shows the smaller size particles, and in this way, it could have a better profile of security than triamcinolone, the most frequently used agent for these injections in our settings 9.
The objective of our study was to evaluate the effectiveness of the epidural injection of betamethasone under x-ray guidance, in patients with unilateral lumbar radicular pain, by the parasagittal interlaminar and transforaminal approaches, using the Brief Pain Inventory (BPI) as a tool of results evaluation. For the parasagittal interlaminar variant, the distribution pattern of the contrast in the anterior epidural space and the presence or absence of radiculogram, as well as of paresthesia or homolateral pain during the steroid injection were also studied. In addition, the profile of side effects and complications of the technique was studied.
MATERIAL AND METHOD
This is a prospective randomized study to evaluate the effect of the epidural injection of betamethasone using the parasagittal interlaminar and transforaminal approaches under radioscopy, in a selected population with unilateral lumbar radicular pain because of disc herniations, lumbar disc protrusions or lumbar spinal stenosis. The Brief Pain Inventory (BPI) was used to evaluate pain in selected patients. This self-administered questionnaire allows patients to quantify the intensity of their pain and the degree in which it interferes with emotional and functional aspects. In addition, the questionnaire consists of additional items evaluating the subjective level of relief that the treatment provides, the location of the pain and its description. The questionnaire is based on questions regarding pain intensity and how this affects different aspects of the person's life, rating from 0 to 10. The analysis of both dimensions allows to obtain the Intensity and Interference Scores. The Intensity Score arises from averaging the responses related to the intensity of pain, while the Interference Score results from averaging the responses related to the functional and affective consequences that such pain produces 10,11,12. The question number 6 of the questionnaire refers to the intensity of the pain at the moment at which the questionnaire is applied, and it can be equivalent to the application of the Verbal Numerical Scale (VNS), usually used as a tool of intensity assessment. The questionnaire was applied before the performance of the procedure, which was considered the baseline situation, and it was repeated in the follow-up one month after the procedure.
The inclusion criteria were: patients with lumbosacral radicular syndrome of 6 or more months of evolution, with a Magnetic Resonance Imaging (MRI) with evidence of disc herniations, disc protrusion or spinal stenosis, with poor response to the pharmacologic treatment for at least 1 month. A decrease of 2 points or more in the VNS (question 6 of the questionnaire) one month after injection was considered a satisfactory response to epidural steroid 13.
The following exclusion criteria were considered: patients under 18 years old and over 80 years old, pregnant women and patients with low back pain without radicular radiation, bilateral lumbar radicular pain and previous spine surgery.
The study was approved by the Committee of Ethics of the University Hospital. All the patients signed the informed consent usually used for the procedure.
The procedure was performed in the surgical room. A peripheral venous catheter was placed with the patient on ventral decubitus position. Asepsis was conducted with alcoholic chlorhexidine and the local anesthesia was performed with 0.5 % lidocaine. Eighteen 3 1/2 or 4 3/4 inches tuohy needles (depending on patient size) were used for the parasagittal interlaminar technique. In the anteroposterior radioscopic view, the needle was inserted into the L4-5 or L5-S1 interlaminar spaces, using the tunnel vision technique, homolateral parasagittal of the side corresponding to the radicular pain (Figure 1). Loss of resistance was performed with saline. In the lateral view, a 4 mL contrast injection (Omnipaque(c)) was administered and the presence of anterior, posterior or both epidurograms was recorded (Figure 1). In the anteroposterior view the presence of radiculogram was recorded (Figure 1). A vial of betamethasone (12 mg of a mixture of phosphate and betamethasone acetate in 2 mL of solution) was then administered diluted with 3 mL of 0.5% lidocaine (total solution: 5 mL). The technical quality of the procedure was determined with the presence of paresthesia or concordant pain during the injection, and radiological data such as presence of radiculogram (Figure 1). Twenty two, 3 1/2 or 4 3/4 inches quincke needles were used in the transforaminal group and inserted using the oblique, lateral and anteroposterior radiological views. The final position of the needle in the oblique view was the subpedicular zone, while in the lateral view was the anterior superior angle or the roof of the neuroforamen, in the so-called safety triangle (Figure 2). The contrast volume injected was equivalent to the performed in the interlaminar group, obtaining a radiculogram and epidurogram after the injection (Figure 2). The solution of betamethasone was the same used in the interlaminar group, injecting the total volume of the solution in one or two levels, depending on clinical criteria.

Fig. 1. Left: parasagittal interlaminar approach L5-S1. On the left, the lateral radioscopic approach is shown, with the Tuohy needle in the epidural space. The injected contrast is distributed through the anterior and posterior epidural spaces. On the right is the anteroposterior radioscopic approach, with the Tuohy needle lateralized to the left. Contrast injection allows to show the epidurogram in this approach and the radiculogram of the left roots L4, L5 and S1.

Fig. 2. Right: transforaminal approach L5-S1. On the left, the Quincke needle with its end located in the anterior superior angle of the corresponding neuroforamen is shown. Contrast injection draws the anterior epidural space. On the right, the anteroposterior radioscopic approach is shown, with the corresponding epidurogram and radiculogram of the right L5 root.
Before the procedure and 4 weeks after it the following data were measured: pain intensity by the VNS (question 6) and Intensity and Interference Scores. The determination of a positive response was established as a decrease of 2 points or more in the VNS. The percentage of patients with positive or negative responses was established.
The data are shown as the mean and its standard deviation. Student t test for paired and independent samples was used, according to the case, and the Chi square test for the statistical evaluation of proportions. A value of p < 0.05 was considered statistically significant. The graphs and the statistical analysis were performed with the program Graphpad Prism version 7.0.
RESULTS
A total of 64 patients with unilateral lumbosacral radicular pain were included in the study between January, 2016 and November, 2017. Ten patients who received the treatment did not return for the follow-up (3 by parasagittal interlaminar approach, 7 by transforaminal approach). The mean age of the patients was of 51 years. Regarding sex, 32 patients were females and 8 patients were males. The mean time of pain evolution was 29 months. All the patients showed disc protrusions in spaces L4/L5 and L5/S1 with variable degrees of canal stenosis in the MRI. None of the treated patients had disc herniation. A total 29 out of 54 patients were treated with betamethasone by parasagittal interlaminar approach and 25 out of 54 patients by the transforaminal approach. Betamethasone administered by the parasagittal interlaminar approach reduced the score in the VNS by 20 %, 7.7 ± 1.5 to 6.2 ± 3,1 (statistically significant difference, p = 0,03, Student t test for paired samples) and by the transforaminal approach 36 %, of 8.3 ± 1.5 to 5.3 ± 3.3 (p = 0.0001). Figure 3shows the normalized values of VNS (that is, showed as percentage of change) of both groups, at baseline and one month after treatment. Although the percentage of change is greater in patients in whom the transforaminal approach was used compared with the interlaminar approach, this difference is not statistically significant (p = 0.13, Student t test for independent samples).

Fig. 3. Variation of the scores on the Verbal Numerical Scale (VNS) compared to baseline values as normalized data, one month after interlaminar (IL, n = 29) and transforaminal (TF, n = 25) betamethasone injections. No significant differences in the variations of the VNS between both approaches were found (Student t test for independent samples).
Intensity and Interference Scores were also reduced by the epidural steroid injection (Figure 4and Figure 5). Betamethasone administered by the parasagittal interlaminar approach produced a statistically significant reduction of the Intensity Score from 7.2 ± 1.2 to 5.8 ± 2.1 and the Interference Score from 7.0 ±1.8 to 5.8 ± 2.5 (p = 0.002 and p = 0.01, respectively; Student t test of paired samples). Betamethasone administered by the transforaminal route decreased the Intensity Score from 7.7 ± 1.6 to 5.7 ± 2.4 and the Interference Score from 7.7 ± 1.7 to 6.3 ± 3, statistically significant reduction (p = 0.0002 and p = 0.008, respectively). No statistically significant differences were found between both approaches when comparing the reduction of both scores.

Fig. 4. Variation of the Intensity Score results compared to baseline values as normalized data, one month after the epidural betamethasone injections of by the interlaminar (IL, n = 29) and transforaminal (TF, n = 25) approaches. No significant differences in the variations of the Intensity Score were found between both approaches (Student t test for independent samples).
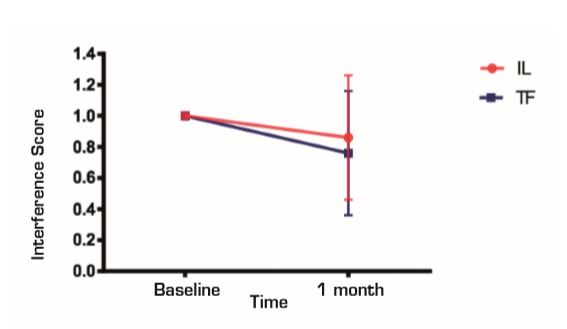
Fig. 5. Variation of the Interference Score results compared to baseline values as normalized data, one month after the epidural betamethasone injections by the interlaminar (IL, n = 29) and transforaminal (TF, n = 25) approaches. No significant differences in the variations in the Interference score between both approaches (Student t test for independent samples).
The percentage of positive responses was higher in the transforaminal group compared with the parasagittal interlaminar approach. The proportion of positive responses in the parasagittal interlaminar and transforaminal approaches were 11/29 (38 %) and 16/25 (64 %) respectively, statistically significant difference with p = 0.01 (Chi square test).
When the changes in the VNS and the Interference Score of those patients whose responses were considered positive using betamethasone interlaminar or transforaminal (11 and 16, respectively) were compared, no differences were found for any of these parameters (Figure 6and Figure 7).

Fig. 6. Variation of the scores in the Verbal Numerical Scale (VNS) compared to baseline values as normalized data, one month after the epidural injections of betamethasone by the interlaminar (IL, n = 11) and transforaminal (TF, n = 16) approaches, including only patients considered as responders (variation in 2 points of the VNS compared to the baseline value). No significant differences in the variations of the VNS between both approaches were found (Student t test for independent samples).

Fig. 7. Variation of the Interference Score results compared to baseline values as normalized data, one month after epidural betamethasone injections by interlaminar (IL, n = 11) and transforaminal (TF, n = 16) approaches, including only patients considered as responders (variation in 2 points of the VNS compared to baseline). No significant differences in the variations in the Interference Score between both approaches were found (Student t test for independent samples).
The score in the VNS of the patients treated with betamethasone by interlaminar route changed from 8.4 ± 1.4 to 3.2 ± 3, which is equivalent to 61 % of improvement, whereas the Interference Score hanged from 6.5 ± 2.2 to 4.5 ± 2, which is equivalent to 30 % of improvement. In the case of betamethasone administered by transforaminal route, the VNS went from of 8.7 ± 1.1 to 3.3 ± 2.3, which is equivalent to 63 % of improvement, whereas the Interference Score decreased from 7.13 ± 2.1 to 4.75 ± 3.1, which is equivalent to 33 % of improvement.
Figure 6shows the changes observed in the intensity of pain in the patients who showed positive responses in both groups, expressed as percentage of change. In both groups patients pain changed from intense to mild pain. Therefore, considering separately the group from "responders", pain went from high to mild intensity in both groups, with an improvement of 2 points in terms of the functional impact of pain measured with the Interference Score (Figure 7). No statistically significant differences in the results were found comparing both approaches when the patients with positive responses were considered separately.
The technical quality of the epidural steroid injection was evaluated in 21 out of 26 procedures performed with the parasagittal interlaminar approach. Anterior epidurograms, that is, achievement of the solution on the ventral epidural space, was obtained in 15 (71 %) of the patients (Figure 1left); 17 (85 %) patients referred pain or paresthesia in the radicular territory during the injection, and a radiculogram was found in 12 (60 %) patients.
No complications of procedures were found in this study.
DISCUSSION
To the best of our knowledge, this study is the first one comparing the interlaminar and transforaminal epidural approaches using the BPI as a tool for assessing outcome. This inventory has been used in our Service for 5 years: it is a useful tool to evaluate the results of analgesic treatments performed 11.
A single injection of betamethasone into the lumbar epidural space through the parasagital interlaminar and transforaminal routes, resulted in a slight, but statistically significant, improvement in pain intensity and its functional impact in patients with unilateral chronic lumbosacral radicular syndrome. No statistically significant differences in these data regarding the administration of betamethasone were found when comparing both approaches.
It is well known that there are patients who, for different factors, do not show satisfactory responses to steroid injections administered by any approach. Factors such as long times of evolution and previous psychological aspects such as anxiety, depression or high levels of catastrophism influence the satisfactory analgesic responses 14,15,16.
Moreover, the type of injury found in the MRI can influence in a lower response, because the best analgesic responses to steroid injections are found in patients with disc herniations 5.
Patients in our sample showed times of pain evolution longer than 2 years, being the injuries found in most of the cases lumbar disc protrusions and variable degrees of spinal stenosis, and in no case disc herniations. The role of psychological factors such as depression, anxiety or catastrophism in the outcome of steroid injections has not been assessed, being such evaluation part of an ongoing study.
When those patients whose pain intensity was reduced by 2 points in the BPI are discriminated, and responders are separated from non-responders, we found that epidural injection by parasagittal interlaminar route shows 38 % of positive responses compared to 64 % when the transforaminal route is used, statistically significant difference.
This reflected a tendency to a more effective analgesic response when betamethasone is administered by the transforaminal route.
Although these outcomes are below those found in other studies, which ranges between 75 % and 80 % of efficacy, our results show the success of a single injection, whereas in other studies it is frequent that repeated steroid injections are evaluated 5.
Those patients who were classified as "responders" using the VNS showed clinically a significant change in pain intensity and its functional repercussion. In them, pain changed from severe pain (8-9 in the VNS) to low pain (3 in the VNS) with a reduction of 2 points in the Interference Score. The observed improvement did not show clinical nor statistically significant according to the approach used for the epidural injection in this group of patients.
Comparison of parasagittal and transforaminal epidural injections has been studied by other authors. Candido, in 2008, describes parasagittal interlaminar epidural approach and finds efficacy similar to the observed with the transforaminal approach. This finding is reproduced by other authors, therefore, it is suggested as an alternative technique to the transforaminal approach without its neurological risks 17,18.
A potential factor to explain the smaller percentage of acceptable responses using the parasagittal interlaminar approach in our study is the use of a smaller volume of solution (5 mL) than the usually used in this route (8 to 10 mL). Nevertheless, a volume from 2.5 to 5 mL is usually used in the transforaminal route, which could explain a greater availability of the steroid in the zone of disc-radicular conflict. The use of greater injected volumes of solution in the epidural space is related to better analgesic responses, probably by an effect of dilution and/or washing of algogenic substances of the epidural space 19.
Another factor that can potentially explain a smaller percentage of success with the parasagittal interlaminar approach is the access of the solution to the anterior epidural space (75 %). In the study conducted by Candido, this approach showed a 100 % reach to the anterior epidural space, which could not be reproduced in the present study 17.
CONCLUSION
A single lumbar epidural injection of betamethasone in patients with lumbosacral radicular syndrome clinically produced a short-term significant reduction of the intensity of pain and its functional repercussion in approximately half of the treated patients. The transforaminal approach showed with more frequency positive responses than the parasagittal interlaminar approach. The techniques were safe, not finding important complications or side effects.
REFERENCES
1. Castromán P, Surbano M, Alberti M, Schwartzmann A, Cristiani F, Ayala S. Inyección epidural de corticoides en el tratamiento del Síndrome Radicular Lumbosacro (SRL). Anest Analg Reanim [Internet]. 2015;28(2):3-3. Disponible en: http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-12732015000200004&lng=es [ Links ]
2. Knezevic NN, Lissounov A, Candido KD. Adding particulate or non-particulate steroids to the local anesthetics when performing parasagittal interlaminar epidural injections. Pain Physician. 2014;17:E633-E671. [ Links ]
3. Manchikanti L, Singh V, Cash KA, Pampati V, Falco FJ. The role of fluoroscopic interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: A randomized, double-blind trial. Pain Practice. 2013;13:547-58. [ Links ]
4. Manchikanti L, Singh V, Cash KA, Falco FJ, Pampati V. Evaluation of the effectiveness of lumbar interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: a randomized, double-blind, controlled trial. Pain Physician. 2010;13:343-55. [ Links ]
5. Manchikanti L, Abdi S, Alturi S, Benyamin RM, Boswell MV, Buenaventura RM, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician. 2013;16(2 Suppl):S49-283. [ Links ]
6. Manchikanti L, Pampati V, Falco FJE, Hirsch JA. Assesment of the growth of epidural injections in the Medicare population from 2000 to 2011. Pain Physician. 2013;16:E349-E364. [ Links ]
7. Manchikanti L, Cash KA, Pampati V, Falco FJE. Transforaminal epidural injections in chronic lumbar disc herniation: a randomized, double-blind, active controlled trial. Pain Physician. 2014;17:E489-E501. [ Links ]
8. Rathmell JP, Benzon HT, Dreyfuss P, Huntoon M, Wallace M, Baker R, et al. Safeguards to prevent neurologic complications after epidural steroid injections. Consensus opinions from a Multidisciplinary Working Group and National Organizations. Anesthesiology. 2015; 122(5):974-84. [ Links ]
9. Benzon HT, Chew TL, McCarthy RJ, Benzon HA, Walega DR. Comparison of the particle sizes of different steroids and the effect of dilution: a review of the relative neurotoxicities of the steroids. Anesthesiology. 2007;106(2):331-8. [ Links ]
10. Keller S, Bann C, Dodd SH, Schein J, Mendoza T, Cleeland CH. Validity of the Brief pain Inventory for use in documenting the outcomes of patients with non-cancer pain. Clin J Pain. 2004;20(5):309-18. [ Links ]
11. Surbano M, Antúnez M, Coutinho I, Machado V, Castroman P. Uso del Brief Pain Inventory (BPI) para la evaluación de las técnicas intervencionistas en el tratamiento de la lumbalgia. Revista El Dolor. 2014(62):10-4. [ Links ]
12. Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Owestry Disability Questionnaire. Spine. 2000;25(24):3115-24. [ Links ]
13. Gatchel RJ, Mayer TG, Choi YH, Chou CR. Validation of a consensus-based minimal clinically important difference (MCID) threshold using an objective functional external anchor. Spinal J. 2013;13(8):889-93. [ Links ]
14. Sivaganesan A, Chotai S, Parker SL, Asher AL, McGirt MJ, Devin CJ. Predictors of the efficacy of epidural steroid injections for structural lumbar degenerative pathology. Spine J. 2016;16(8):928-34. [ Links ]
15. Samwel H, Sappendel R, Crul BJP, Voerman VF. Psychological predictors of the effectiveness of radiofrequency lesioning of the cervical spinal dorsal root ganglion. Eur J Pain. 2000;4:149-55. [ Links ]
16. Turner JA, Comstock BA, Standaert CHJ, Heagerty PJ, Jarvic JG, Deyo RA, et al. Can patient characteristics predict benefit from epidural corticosteroid injections for lumbar spinal stenosis symptoms? Spine J. 2015;15:2319-31. [ Links ]
17. Candido KD, Raghavendra MS, Chintagada M, Badiee S, Trepashko DW. A prospective evaluation of iodinated contrast flow patterns with fluoroscopically guided lumbar epidural steroid injections: the lateral parasagittal interlaminar epidural approach versus the transforaminal epidural approach. Anesth Analg. 2008;106:638-44. [ Links ]
18. Chang Chien GC, Knezevic NN, McCormick Z, Chu SK, Trescot AM, Candido KD. Transforaminal versus interlaminar approaches to epidural steroid injections: a systematic review of comparative studies for lumbosacral radicular pain. Pain Physcian. 2014;17:E509-E524. [ Links ]
19. Rabinovitch DL, Peliowski A, Furlan AD. Influence of lumbar epidural injection volume on pain relief for radicular leg pain and/or low back pain. Spine J. 2009;9:509-17. [ Links ]
Received: July 28, 2018; Accepted: March 19, 2019











 texto en
texto en 


