Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista de la Sociedad Española del Dolor
versão impressa ISSN 1134-8046
Rev. Soc. Esp. Dolor vol.26 no.5 Madrid Set./Out. 2019 Epub 23-Mar-2020
https://dx.doi.org/10.20986/resed.2019.3742/2019
ORIGINALS
New strategies for postoperative pain management in tonsil surgery. Is all that glitters gold?
1Residente de Anestesiología y Reanimación. Complejo Asistencial de Zamora, España.
2Licenciado Especialista en Anestesiología y Reanimación. Complejo Asistencial de Zamora, España.
Introduction:
Tonsillectomy is surgical procedure which is being every time more often in adult patients. Postoperative pain may be very intense, and it has a very important mark in the quality of life of our patients. Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) may not be enough for pain management during the first 48 hours post-surgery. Morphine patient-controlled analgesia (PCA) is an effective and safe alternative for postoperative acute pain management.
Material and methods:
Our main goal was to compare the quality of analgesia between morphine PCA and acetaminophen and NSAIDs use for acute pain control in adult patients who had tonsillectomy surgery. Our secondary goal was to study the frequency of side effects and the satisfaction level on each group.
A retrospective cohort study was performed with those adult patients who underwent tonsillectomy during the year 2017. Pain was evaluated during the first 24- and 48-hours post-surgery with the numerical rating scale (NRS). Secondary side effects were reported. The statistical study was performed with SPSS® programme.
Results:
a total of 46 patients were evaluated, 20 patients belonged to the group for conventional analgesia and 26 belonged to the group of morphine PCA. We did not find significative differences in the demographic characteristics in both groups. PCA group had a smaller NRS compared to the other conventional analgesia group during the first 24 and the 48 hours. The difference was statistically significant for pain control during activity and resting. The incidence of secondary effects was greater for the PCA group (46,15 %) than for the acetaminophen and NSAIDs group (15 %).
Discussion:
Analgesia with morphine PCA is more effective than the administration of acetaminophen and NSAIDs for postoperative pain control in tonsillectomy procedure in the adult patient. The adverse effects are more frequent with morphine PCA.
Key words: Morphine; analgesia patient-controlled; tonsillectomy; postoperative pain
INTRODUCTION
The tonsillectomy is an increasingly frequent surgical procedure in adult patients. In recent years, advances in the surgical techniques have been developed. However, the treatment for the postoperative pain supposes a great challenge for anesthesiologists 1. Pain is related to the mucosa damage, which is innervated by the glossopharyngeal and the vagus nerves 2.
Pain has a great impact on the patient, it is of severe intensity, it makes difficult the feeding and interferes with night rest.
Conventional analgesia (CA) with acetaminophen and NSAIDs is inadequate for a satisfactory pain management in the first 48 hours after surgery 3. Patient-controlled analgesia (PCA) 4is effective, safe and practical for the treatment of postoperative pain.
The analgesic quality is one of the most important objectives that the anesthesiologist looks for in the postoperative period. According to the World Health Organization, the quality is defined as the process by which each patient has to receive a series of therapeutic measures to obtain the best possible result, with the minimum risks, adverse effects and the maximum satisfaction of the patient 5.
It is difficult to provide a unique definition of satisfaction, because satisfaction can often depend on the expectations that each patient has, if these have been satisfied and, on the treatment that the patient has perceived from the health provider more than on the analgesic result itself 6. Therefore, satisfaction is considered the fulfillment or not of the expectations of the patient, added to the technical or quantitative component of pain management.
AIMS
The primary aim of the study was to compare between the analgesic quality of morphine PCA and the analgesia with acetaminophen and NSAIDs in adult patients who underwent a tonsillectomy.
The secondary aims were to analyze the incidence of adverse effect and the satisfaction in each one of the groups.
MATERIAL AND METHOD
A retrospective cohort study was conducted. The sample consisted of patients undergoing tonsillectomy scheduled in 2017 in the Healthcare Complex of Zamora (Spain).
Patients were divided into two groups: a PCA group and a CA group.
The CA consisted of a bolus of intravenous acetaminophen (1 g) administered every 8 hours, alternated with bolus of intravenous metamizole (2 g). The amount of 50 mg of intravenous dexketoprofen every 8 hours was scheduled as rescue analgesia. The PCA was administered with a continuous perfusion of 1 mg of morphine hydrochloride per hour, and bolus at the patient's request of the 0.5 mg of morphine. The closing time was 20 minutes.
The group treated with morphine PCA was scheduled antiemetic prophylaxis with intravenous ondansetron 4 mg/8 h. Patients treated with CA did not receive prophylactic medication because the administered drugs are barely emetogenic being able to add, if administered, undesirable side effects because of prescribing them unnecessarily.
The inclusion criteria were: patients between 16-80 years who underwent an tonsils elective surgery, without hypersensitivity to opioids, that accepted and understood the handling of the PCA.
Patients who could not understand the handling of the PCA, patients who refused the technique, patients with history of allergy to opioids and those with acute respiratory decompensation and/or hemodynamic instability were excluded.
The following variables were recorded: pre-existing medical condition, pain measured with the verbal numerical scale (VNS), at rest and on exertion, defined as speaking, drinking water or eating, in the 24 hours and the 48 hours after surgery. In addition to age, the physical condition according to the American Society of Anesthesiologists (ASA), the allergies and the appearance of adverse effects: allergic reaction, dizziness, nauseas, nauseas and vomits, pruritus, urinary retention, ileus, and respiratory depression. Moreover, duration of the surgery was recorded, the beginning of the oral tolerance and the demand, to greater, of the prescribed of postoperative analgesic and, finally, the subjective assessment of the patient with a Likert scale of 5 points.
Adequately controlled pain was defined with VNS on exertion below 5 and VNS at rest below 3.
Groups were not randomized because this was a retrospective study proposed after the implementation of the pharmacological measures. Group assignation was based on the criterion of the anesthesiologist in charge of the Post-anesthetic Recovery Unit who prescribed one treatment or the other. Moreover, the surgeries were performed by different members from the Service of Otorhinolaryngology of our hospital, so very small groups were formed, which difficulted forming sub-groups.
The statistical analysis was performed using the program SPSS(r). Qualitative variables were analyzed using the chi square test and the Fisher exact test, whereas quantitative variables were analyzed using the nonparametric Mann-Whitney U test.
RESULTS
A total of 53 adults underwent elective tonsillectomy in 2017. Five of them were excluded because they had a postoperative analgesia different from those that we wanted to analyze. Two adults were excluded because they had not got a complete follow-up. Therefore, we analyzed 46 patients, 26 of them were included in the PCA group, whereas the remaining 20 patients received CA (CA group) (Table 1).
No statistically significant differences between groups in relation to age, sex or the disease by which the surgery was indicated were found.
Most of the patients they had a classification of their physical condition as ASA I and II.
In our center, the tonsillectomy in adults does not follow a regime of Major Outpatient Surgery, therefore all patients are admitted to the Otolaryngology Service for several days (average stay 4.1 ± 1.6 days in the AC group; average stay: 4.3 ± 1.5 days in the PCA group) without significant differences (p = 0.35) between the stay of both groups.
A patient of the AC group was re-operated on the 2nd day after surgery and another of the PCA group on the 3rd day, finding no difference between the incidence of post-surgical bleeding between both cohorts (p = 0.68).
Pain
VNS 1.st day
During the first day, for the pain at rest, the maximum VNS score was 7 in the PCA group, whereas it was 10 in the CA group.
The median of the first group was 1, whereas the median of the second group was 4.
Regarding pain on exertion, patients of the PCA group showed a maximum VNS of 9 and a median of 3; whereas patients of the CA groups shower a maximum VNS of 10 and a median of 5.
The differences in the NVS were statistically significant for both pain at rest (p = 0.002) and on exertion (p = 0.022) (Figure 1).
VNS 2nd day
Score VNS at rest during 2nd day showed a clear difference between those treated with morphine hydrochloride and those treated with CA (p = 0.000) (Figure 2).

Fig. 2. Box-plot representing pain measured by the verbal numerical scale (VNS) on the 2nd day after surgery, on the left (light pink): at rest, on the right (dark pink): on exertion.
The median of the patients of group PCA was 0.
Those patients treated with CA showed a VNS median of 3, with large data dispersion (VNS 0-8).
In relation to VNS score on exertion during the second day, the median was 0 for the PCA group and 4 for the CA group. These differences were statistically significant.
Assessment by the patient
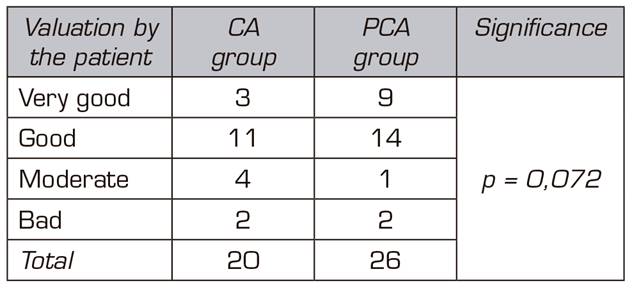
Patients were surveyed regarding their satisfaction with the administered analgesia (Table 2). Patients were requested to classify the received analgesia as very good, good, moderate, bad and very bad.
No significant differences (p = 0.072) between treatment groups were found.
Adverse Effects
Finally, as a secondary aim of this study, we also analyzed the incidence of adverse effects that presented our patients after the surgery and once discharged from the Post-anesthetic Recovery Unit (Table 3).
Twelve patients from the group treated with morphine PCA showed adverse effects (46.15%), whereas only 3 patients from the group treated with CA showed some type of complication (15%).
Only 5 patients of PCA group needed a rescue bolus of self-administration with PCA system. The average of administrations was 0.5 in 48 hours, with a minimum of 0 bolus and a maximum of 3. The number of rescue bolus was not associated (p = 0.56) with the appearance of adverse effects. Eleven out of 20 patients of the CA group requested from the nursing staff the rescue medication that were set between the scheduled doses of acetaminophen 1 g and metamizole 2 g.
Differences between men and women at the time of appearance of adverse effects were not found (p = 0.128).
Nausea and vomiting were the most frequent adverse effects.
In the group of patients treated with CA (Figure 3), as above mentioned, 3 of them showed some type of adverse effect, nausea and vomiting were the most frequent.

Fig. 3. Adverse effects found in patients treated with morphine (on the left) and with conventional analgesia (on the right).
All the patients of both groups initiated liquid oral tolerance according to the criterion of the Service of Otorhinolaryngology 4 hours after surgery, progressing throughout the 8 first hours to tolerance to solids with no complication.
DISCUSSION
The VNS of the patients of the PCA group was significantly lower than those treated with CA, therefore it is possible to affirm that the morphine is more effective than the conventional treatment in pain management, in both at rest and on exertion, at all the periods of time of the treatment of adult patients who underwent elective tonsillectomy.
Despite the present tendency is going towards a minimum administration of postoperative opioids, we should keep in mind that these are excellent analgesics for surgeries with moderate-severe pain.
However, the treatment of the postoperative pain in the tonsillectomy is still an unsolved challenge. Pain intensity is important in the first 48 hours after surgery, although the discomfort can last beyond one week.
The NSAIDs have been associated with less adverse effects than opioids, nevertheless, NSAIDs are inadequate to manage severe pain. Furthermore, these drugs alter platelet aggregation and prolong bleeding time, and can be associated with postoperative hemorrhage 7.
The results of our study are consistent with the published by Ballantyne et al. 8in 1993, and later shown by McNicol et al. 4in 2015. In both studies, patients whom controlled by themselves the analgesia had less pain than those depending on the analgesia administered by the nursing staff.
Despite no significant differences were found between both groups (p = 0.072) when analyzing the global satisfaction of pain control, we could find a tendency of greater satisfaction in the group of patients treated with intravenous morphine. This result is consistent with the literature, McNicol et al. 4(2015) concluded that patients with morphine PCA showed a greater satisfaction with pain management.
The presence in our study of a greater number of complications in the patients treated with morphine compared to those treated with CA is consistent with the previously published. Watcha et al. 9in 1993 found a higher incidence of postoperative nausea and vomiting in those patients treated with opioids compared to patients treated with NSAIDs, and some years later Kehlet et al. 10confirmed these findings.
Although the tonsillectomy is an increasingly frequent procedure in the adult patient, it is still a rare surgical intervention in our hospital. The small sample size of the present study can condition the strength of the conclusions, being necessary to increase the sample size to improve the statistical power.
CONCLUSIONS
Pain management after tonsils surgery is better with morphine PCA than with CA.
More than half of the patients treated with CA need rescue medication.
The satisfaction of both groups of patients is good or very good and it does not show significant differences.
The presence of adverse effects is higher in patients treated with morphine PCA.
REFERENCES
1. Gerbershagen HJ, Aduckathil S, van Wijck AJM, Peelen LM, Kalkman CJ, Meissner W. Pain Intensity on the First Day after SurgeryA Prospective Cohort Study Comparing 179 Surgical Procedures. Anesthesiology. 2013;118(4):934-44. DOI: 10.1097/ALN.0b013e31828866b3. [ Links ]
2. Poller K, Volk GF, Wittekindt C, Meissner W, Guntinas-Lichius O. Verbesserung der Schmerztherapie nach Tonsillektomie bei Erwachsenen durch Schmerzmessung mit QUIPS ("Qualitätsverbesserung in der postoperativen Schmerztherapie"). Laryngo-Rhino-Otol. 2011;90(2):82-9. DOI: 10.1055/s-0030-1269848. [ Links ]
3. Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-57. DOI: 10.1016/j.jpain.2015.12.008. [ Links ]
4. McNicol ED, Ferguson MC, Hudcova J. Patient controlled opioid analgesia versus non-patient controlled opioid analgesia for postoperative pain. Cochrane Database Syst Rev. 2015(6):CD003348. doi: 10.1002/14651858.CD003348.pub3. [ Links ]
5. Organization WH, Europe dOf. The principles of Quality Assurance: Report on a WHO meeting. Euro Rep Stud. 1985;(94):1-37. [ Links ]
6. Linder-Pelz S. Social psychological determinants of patient satisfaction: a test of five hypotheses. Soc Sci Med. 1982;16(5):583-9. DOI: 10.1016/0277-9536(82)90312-4. [ Links ]
7. Kokki H, Nikanne E, Aho M, Virtaniemi J. Pain Intensity after Laseruvulopalatoplasty and Tonsillectomy. Otolaryngol Head Neck Surg. 2003;128(2):273-9. DOI: 10.1067/mhn.2003.82. [ Links ]
8. Ballantyne JC, Carr DB, Chalmers TC, Dear KBG, Angelillo IF, Mosteller F. Postoperative patient-controlled analgesia: Meta-analyses of initial randomized control trials. J Clin Anesth. 1993;5(3):182-93. [ Links ]
9. Watcha M, White P. Postoperative Nausea and VomitingIts Etiology, Treatment, and Prevention. Anesthesiology. 1992;77(1):162-84. [ Links ]
10. Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001;87(1):62-72. DOI: 10.1093/bja/87.1.62. [ Links ]
Received: May 13, 2019; Accepted: September 09, 2019











 texto em
texto em