INTRODUCTION
Pain continues to be a symptom which is almost constantly present in critically ill patients. Its ineffective assessment and control are associated with an increase in mortality and morbidity 1. The situation experienced by the patient is further aggravated by the difficulty to communicate, as well as by the fear and anxiety inherent to being admitted to an Intensive Care Unit (ICU). These circumstances manifest themselves through changes in several areas: level of consciousness, sleep, circulatory, endocrine, metabolic, gastrointestinal, and psychological 2,3,4.
However, although the changes caused by pain are well known -as well as the fact that it constitutes a stressor agent for ICU patients-, the rates of uncontrolled pain in critically ill patients remain high 5, and pain continues to be undervalued 6. The American Association of Critical-Care Nurses 1mentions that critically ill patients experience pain throughout their hospitalization. More than 30 % of ICU patients feel pain when resting, while more than 50 % feel pain during routine care procedures (mostly nursing interventions, which include the aspiration of secretions, positioning, and wound care, among others).
Pain can be manifested through vocalizations, movements/mobility, facial expressions, mood or behaviors 2, and remains one of the challenges when providing care to critically ill patients 2,7. Pain cannot be accurately assessed if we take into account only physiological factors, because they might be affected by various phenomena, such as anxiety and sepsis 8. Therefore, it is important to promote the systematic use of adequate assessment tools, which are sensitive to behavioral indicators. These instruments allow the implementation and optimization of both pain relief and pain control strategies 9, reducing long-term complications 10.
Uncontrolled pain, due to an inadequate assessment and the ensuing non-intervention, may result in complications during the patient's recovery process, and, consequently, in additional treatment costs 11. As a major outcome, pain may evolve and become chronic, commonly leading to various psycho-social effects, such as depression, anxiety, delirium, and post-traumatic stress 2.
Thus, the provision of an effective pain management to the patient, through the correct use of appropriate assessment tools, and the consequent intervention and reassessment, will allow the obtainment of several health benefits, such as a reduction in mechanical ventilation time, a decrease in healthcare-associated infection rates, and a decline in hospitalization length within the ICU 6,10.
In this sense, nurses, being a professional group favored by its prolonged contact and close proximity with respect to the patient/family, play a key role in pain monitoring, as well as in the adjustment of treatment plans, since pain may undergo some changes 3. Hence, this study tried to review, in a systematic manner, the existing literature about the scales/indicators which are available for pain monitoring in critically ill patients incapable of verbalizing. Additionally, we attempted to identify the applicability of the scales used for pain assessment in critically ill patients who are unable to verbalize their suffering.
METHODOLOGY
This study was conducted according to the methodology recommended by the guidelines of the Joanna Briggs Institute for Evidence Based Practice 11. It was oriented by the following research question that was developed in the PEO format: (P) Population (Type of Participantes) - Critically ill patients incapable of verbalizing; (E) Exposure of interest (Independent variable) - Scales/Indicators for pain monitoring; (O) Outcome (Independent variable) - Applicability.
We defined inclusion and exclusion criteria (Table 1) within the following categories: participants (selection of studies regarding critically ill patients, who were unable to verbalize, and presented an age greater than, or equal to, 18 years); Exposure (Scales/Indicators for pain monitoring); Outcome (applicability of scales/indicators for pain assessment); and available documents (selection of articles which were accessible in full text, and were published in Portuguese, English, Italian, or Spanish, between January 2012 and December 2017). Additionally, all works concerning non-original or qualitative studies were excluded.
Search strategy
Our systematic review of etiology was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist 12, in order to achieve the standards which are usually required for this type of work.
Regarding the search that was performed within the databases, two researchers started the search by inserting the search terms. In order to identify the specific database descriptors, we resorted to several keywords of articles related to the theme under study. Subsequently, the resulting descriptors were included in the Major Heading (MH) option, and were consulted in the Health Sciences Descriptors (DeCS) catalogue.
We then conducted a systematic review, encompassing the articles published in journals indexed in the following databases: MEDLINE, CINAHL and Cochrane Central Register of Controlled Trials. To that purpose, we used the descriptors "Doente Crítico" ("Critically Ill Patient"), "Dor" ("Pain"), "Escala" ("Scale") and "Instrumento" ("Instrument"), together with some variations of these terms, both in Portuguese ("doente crítico" AND "dor" AND "escala" OR "instrumento") and in English ("critical patient" OR "critically ill patient" AND "pain" AND "scale" OR "instrument"), which were obtained through the combination of the Boolean operators AND, and OR.
In a first phase, the titles and abstracts of all the articles previously identified through the search strategy were carefully read, in order to select the works that answered the guiding question and met the inclusion criteria. This reading process, together with the evaluation of the evidence's quality, was performed by two independent researchers, to ensure a critical assessment during the articles' selection procedure. The abstracts which did not present sufficient information regarding inclusion and exclusion criteria were selected for further analysis of the entire text. Subsequently, the same researchers assessed, in an independent manner, the full-text articles, selecting the studies according to the eligibility criteria. Due to some disagreements among the researchers, we requested the intervention of a third evaluator.
The assessment of the studies' quality was achieved through a tool proposed by the Joanna Briggs Institute 12: the Critical Appraisal Checklist for Descriptive/Case Series. In the absence of any guidelines concerning the operationalization of the classification grid used to evaluate the studies' quality, we adopted the following criteria, considering the percentage of the global items: low quality, when less than 50 % of the items were met; moderate quality, when 50 % to 75 % of the items were met; and high quality, when more than 75 % of the items were met.
RESULTS
A total of 149 studies, classified as potentially relevant, were obtained through this systematic review's search strategy; 22 of these articles were considered not qualified, due to duplication, or through the employment of the search limiters; 95 were set aside after title reading; and 13 were excluded after abstract reading. The remaining 19 articles were then subjected to an eligibility assessment, through full reading. Finally, 11 studies, which fully met the pre-established inclusion criteria, were included in the systematic review (Figure 1).
According to the previously mentioned criteria for methodological quality assessment, 10 articles were considered of high quality, while the remaining 2 were considered of moderate quality. The bibliographic identification of the included studies is shown in Table 2.
Table II. Synthesis of the information extracted from the 12 studies included in the SLR, following a standardized method that identifies the study, as well as its objectives, method, results and conclusions

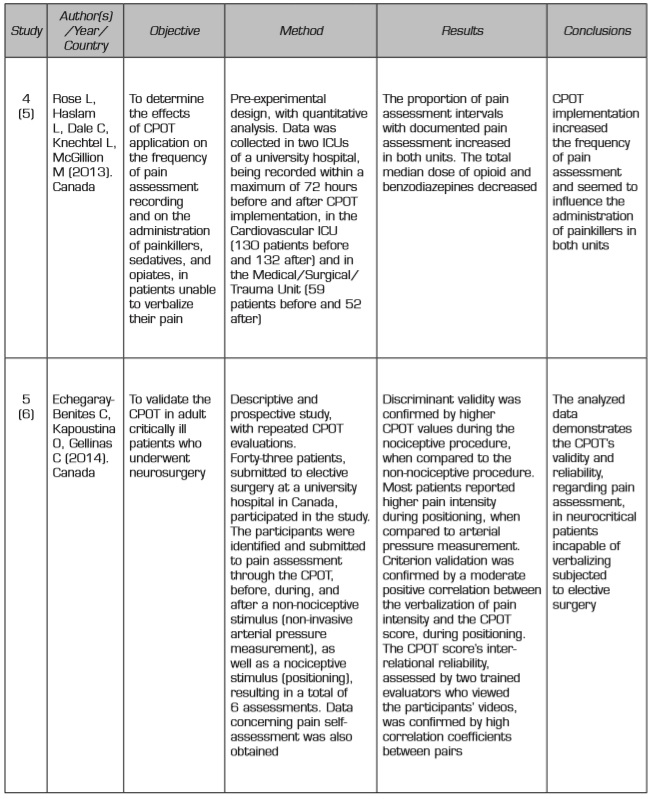
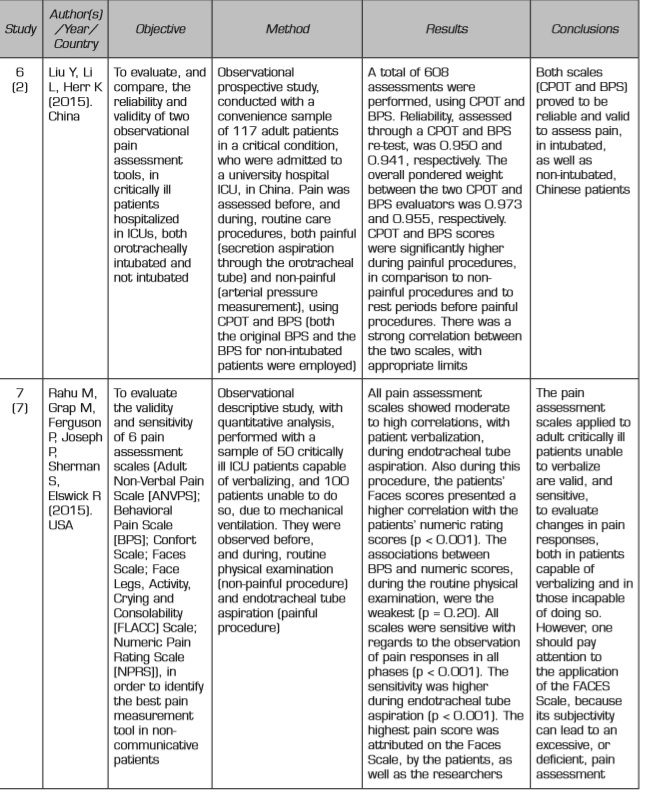

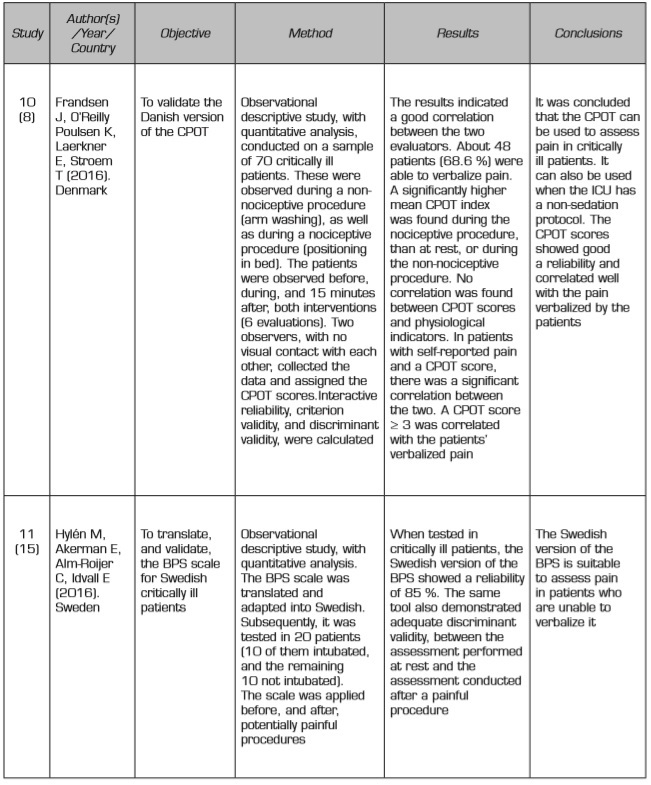
The extraction and synthesis of the information contained in the 11 selected studies was performed by two researchers, who used a standardized method that encompassed the following aspects: identification, objectives, methodology, results and conclusions (Table 2).
Regarding the analyzed articles, 5 aimed to validate the Critical-care Pain Observation Tool (CPOT) behavioral scale for the respective population 6,8,16, 2 were related to the CPOT's implementation for pain assessment in patients incapable of verbalizing 5,10, and the remaining 5 intended to evaluate and compare the sensitivity of pain assessment scales - including the Behavioral Pain Assessment Scale (BPS) and the CPOT - in critically ill patients2,3,7,9.
DISCUSSION
While conducting this systematic review of the available literature, we found that the application of pain assessment tools is essential for achieving effective and documented pain assessment procedures 5. Some studies demonstrate the validation of pain assessment tools, which proved to be valid and reliable 2,5,6,8,10,13,16for the respective population. The results indicate that the BPS 2,3,16and the CPOT 2,5,6,11,12,13,14are the most appropriate scales for pain monitoring in critically ill patients. These evaluation instruments are the most studied and also the most widely applied. Nevertheless, two works 3,7concluded that the Adult Non-Verbal Pain Scale (ANVPS), the Confort Scale, the Faces Scale, and the Pain Assessment Behavioral Scale (PABS) as well as BPS for Non-Intubated Patients (BPS-NI) 2were just as valid and equally sensitive to pain responses during painful procedures. This occurred both in the patients who were able to verbalize and in the patients who were unable to do so. However, to avoid an ineffective pain assessment, the same authors emphasize the importance of taking into account the Faces Scale's subjectivity, whenever it is chosen 7.
Considering that the BPS and the CPOT are the scales of choice for pain assessment in critically ill patients, we investigated the existence of comparative studies between these two instruments. In one of those studies, both scales are considered valid for pain assessment in critically ill patients experiencing pain. Nonetheless, the BPS showed score changes both at rest and with the introduction of a painful stimulus, unlike the CPOT, which only suffered alterations in the presence of a painful stimulus 6. This indicates that the CPOT is the preferred tool for pain assessment in the studied population.
One of the works revealed that pain monitoring through the CPOT resulted in the administration of fewer painkillers and sedatives, as well as in shorter ventilation and hospitalization periods 10. Another study demonstrated that, despite being an effective scale to assess the pain in patients incapable of verbalizing it, the CPOT should be used with caution in cases of chronic pain, or delirium 6.
On the other hand, because the BPS should only be used in ventilated patients, it is considered that the CPOT should be preferred in non-ventilated critically ill patients, who present awareness and communication alterations 6,8,9.
Currently, the BPS is the only pain assessment scale validated for the Portuguese population, having been selected by the Sociedade Portuguesa de Cuidados Intensivos (the Portuguese Intensive Care Society). However, given that this scale should only be used in ventilated patients, it becomes essential to validate the CPOT in the near future, to provide a more comprehensive pain assessment in critically ill patients. According to several studies, the CPOT is the most appropriate tool when the patient is no longer sedated, nor ventilated, but remains incapable of verbalizing pain for various reasons - such as, for example, an alteration of the awareness state -, because the "adaptation to the ventilator" assessment item can be replaced by the "patient's vocalization" 6,14.
In the absence of pain assessment tools, the nurses' description of the pain phenomenon is recorded in the form of a narrative, with body movements being the most frequent descriptive element. This confirms the need to continue the research efforts to improve care through the implementation, and consequent use, of pain assessment behavioral scales in critically ill patients 11.
It is disturbing to note that 23 % of the patients who were admitted to ICUs did not benefit from a documented pain assessment during their entire hospitalization period 17. This is in line with the results obtained in previous studies. The remaining patients had their pain assessed in the form of a narrative, with behavioral indicators being often used.
Concerning the future, it is fundamental to develop guidelines, which orient healthcare professionals towards an effective pain management. Additionally, there should be a consensual model, involving a shared decision process, with the participation of nurses and other healthcare professionals 12.
In order to obtain better clinical results, it is essential to establish updated guidelines specifying the use of assessment tools, such as behavioral scales, in critically ill patients who are unable to verbalize pain 6. This need exists because pain monitoring in orotracheally intubated patients - thus, incapable of verbalizing - is fairly recent, and pain remained undocumented 10, which resulted in a higher prescription of opioids (around half of the patients admitted to ICUs was medicated with opioids). According to the same authors, pain monitoring through behavioral instruments allows the attainment of health gains - such as a decrease in the patients' ICU hospitalization period, as well as in the invasive ventilation period 6-, thus improving the patient's/family's satisfaction level 10.
Additionally, two studies 3,13were conducted to explore the challenges faced by nurses regarding pain management, and also to understand how they documented the presence of pain in their patients. It was found that pain management remains a priority in the provision of nursing care. However, when managing pain, nurses continue to recognize some limitations with respect to their autonomy, which could be overcome through the implementation of pain assessment scales and the respective action protocols 3. It is the nurse's responsibility - as well as his/her professional duty - to provide effective pain relief, bearing in mind that, if sedatives and painkillers are being administered to a patient, he/she may seem misleadingly calm and without pain 18. Endotracheal intubation emerged among the painful procedures more frequently reported by patients admitted to ICUs.
Concerning pain indicators, the studies evaluated: facial expression, body movements, muscle tone, adaptation to mechanical ventilation and vocalization 3,14. When approaching critically ill patients, nurses are in a privileged position to assess their behaviors. Therefore, these professionals should be sensitized and encouraged to use behavioral assessment scales 3.
CONCLUSION
Pain is a subjective symptom that is difficult to assess and to characterize in critically ill patients, having an impact on their general condition and their recovery.
The present work aimed to perform a systematic review of the existing literature regarding of the applicability of scales/indicators to available for pain monitoring in critically ill patients who are unable to verbalize.
Taking into account that pain is an ever-present sign in ICU patients, possessing knowledge about the most appropriate pain scales and indicators may contribute to an improvement in practices.
The obtained results suggest that, to achieve an effective pain management in critically ill patients, it is fundamental to assess pain using behavioral scales such as the BPS and the CPOT. In the analyzed articles it's evident the need of a instrument that considers indicators such as: facial expression, body movements, muscle tone, adaptation to mechanical ventilation and vocalization.
In Portugal, the BPS has been validated and it is the scale most commonly used to assess pain in critically ill patients, however, given that the BPS should only be applied to ventilated patients, but not all the patients incapable of communicating are ventilated, the CPOT, PABS and BPS-NI, emerges as an alternative, because they can be applied to both ventilated and non-ventilated patients unable to verbalize, whether they are sedated or not. Most studies refer to the CPOT as being the most reliable when evaluating the pain in patients who are unable of communicate.
For all these reasons, and based on the obtained data, we can state that it is possible to improve the care provided to critically ill patients experiencing pain, through its monitoring. This improvement contributes to the administration of fewer painkillers and sedatives, as well as shorter ventilation and hospitalization periods, having an impact on treatment effectiveness. Finally, a more effective treatment produces health gains and has lower costs for the institutions.
Therefore, according to the obtained results, it is essential to validate the CPOT for the Portuguese population, as well as to conduct studies that emphasize the experiences of hospitalized patients who were prone to pain during their hospital stay. In addition, there is a need for studies which demonstrate the effectiveness of non-pharmacological interventions, so that the latter can be used simultaneously with pharmacological ones, in order to enhance results with a greater safety and lower costs, thus improving care practice.
















