My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Salud Pública
On-line version ISSN 2173-9110Print version ISSN 1135-5727
Rev. Esp. Salud Publica vol.93 Madrid 2019 Epub Sep 07, 2020
ORIGINALS
Physicians' awareness and assessment of shared decision making in oncology practice
1Department of Quantitative Methods for the Economy and Business. University of Huelva. Huelva. Spain.
2Department of Financial Economics, Accounting and Operations Management. University of Huelva. Huelva. Spain.
3Radiation Oncology Service. Juan Ramón Jiménez Hospital. Huelva. Spain.
4Medical Oncology Service. Juan Ramón Jiménez Hospital. Huelva. Spain.
Background:
Implementation of Shared Decision Making (SDM) in oncology is limited. The objective of the study was to determine the extent of physicians' awareness of Shared Decision Making (SDM) in their treatment of cancer patients, the usefulness that they assign to SDM, the role they play, their assessment of SDM, and perceptions of the main barriers and facilitators to its use.
Methods:
A questionnaire was completed by medical oncologists, radiation oncologists and general surgeons working in Andalusia (Spain). Sociodemographic, clinical-care and aspects of SDM variables were collected. SDM was evaluated using the SDM-Q-Doc questionnaire. Non-parametric contrasts were used to determine the possible differences between medical specialties.
Results:
The questionnaire was sent to 351 physicians. The response rate was 37.04%, 63 women and 67 men, with an average age of 45.6 years and 18.04 years' experience. Of these, 33.08% were medical oncologists, 34.61% radiation oncologists and 29.23% general surgeons. A total of 82.3% stated they had received no training in SDM, whereas 33.8% said they knew a lot about SDM and applied it in practice; 80% considered it to be very useful. In addition, 60% of respondents said they were mainly the ones who made the decisions on treatment. An evaluation of SDM on the SDM-Q-Doc scale showed that all the specialities scored more than 80/100. The main barriers to applying SDM were the difficulty patients experienced in understanding what they needed to know, the lack of decision aids and time.
Conclusions:
Some 82% of physicians have no training in SDM and 66% don´t use it in practice, with decisions on treatment taken mainly by the physicians themselves. Strategies to increase training in SDM and to implement it into clinical practice are important.
Key words: Shared decision making; Physicianpatient relations; Neoplasms; Role; Barriers; Facilitators
INTRODUCTION
Making decisions in oncology can be a complex issue. On numerous occasions patients and physicians have to choose between various treatments available that offer both risks and benefits in equal measure; for example, deciding between a tumourectomy or mastectomy in breast cancer cases, or between active vigilance, surgery or radiotherapy in prostate cancer. It is in such cases, where there is no single or “best” decision, that it is essential to consider the values and preferences of the patient1, and incorporate new clinical practice models such as Shared Decision Making (SDM).
SDM is a joint interactive decision-making process between physician and patient characterized by the flow of information in both directions between the two parties. During this process, the physician shares technical information with the patient, who in turn provides the physician with personal information, so that they can reach an agreement on the treatment option to be chosen.
The use of SDM is linked to numerous benefits such as reducing patients' anxiety and depression, improvements in their quality of life and an increase in patients' satisfaction with their treatment2,3, and in physicians' job satisfaction4. Despite these advantages, there is no evidence that SDM has been widely implemented in practice5. Studies that have investigated why this is so have analysed the main barriers and facilitators to its application6.
In Spain in recent decades, public institutions have shown increasing interest in empowering patients and their active participation in making medical decisions. In this sense, the most significant progress in SDM has been the creation of a series of health information resources aimed at educating patients7, as well as different decision aids (DAs)1.
In terms of research on SDM in Spain, and despite the steady increase in the number of studies in this field since the last decade7, very little research has been done on SDM in relation to oncology. The studies have mainly centred on analysing the perspectives of cancer patients, in particular work by the Josep Laporte Foundation and the Universidad de los Pacientes, in which the patients wish to play a more active role in the health care process and be consulted on the diagnostic and therapeutic options available to them8,9. Later studies reach similar conclusions revealing that according to the patients' perspective, SDM has yet to be rolled out in practice10, and identifying the main factors that influence it11.
Furthermore, and despite the fact that success in SDM in oncology largely depends on physicians, little research has been done on their perspective on this issue. Studies have tended to focus on the validation of the SDM-Q-Doc questionnaire to measure SDM12, and to analyse the rates of satisfaction among health care professionals and their patients13.
Given that it is essential to continue raising the rate at which SDM is implemented in oncology in Spain, we consider it necessary to carry out an in-depth study of aspects of SDM that have so far been ignored. The aim of our work is to analyse the extent of knowledge of SDM among oncology physicians and its usefulness to them, together with the main barriers and facilitators to its implementation from their viewpoint. We will also examine the physicians' perception on who should have made the decision on treatment and who, in reality, made that decision; and we will measure the SDM process from their perspective according to the SDM-Q-Doc scale.
SUBJECTS AND METHODS
Participants
This was a descriptive transversal study performed between September 2015 and February 2016 via an online questionnaire. The study population was formed of medical oncologists, radiation oncologists and general surgeons as well as other specialists related to oncology, belonging to the Andalusian Health Service.
Using the database available from the various scientific societies, a list was drawn up of 351 e-mail addresses (167 medical oncologists, 78 radiation oncologists and 106 general surgeons); the SurveyMonkey software was used in the research. The study received no financial support, and before initiating the study approval was obtained from the Ethics Committee of the Juan Ramón Jiménez Hospital in Huelva
Questionnaire
The questionnaire started with a detailed explanation of the study, and once the participant had agreed to take part, he/she completed the survey, which was anonymous and for which the participant received no payment. At 15 and 45 days after sending out the questionnaire, the participants were sent a reminder to complete the survey.
Since it was possible that not all the participants were familiar with the term SDM, it was defined in the questionnaire according to Charles et al14.
The survey was in three parts:
The sociodemographic information referred to gender and age. The clinical information referred to years of experience as a health care professional, area of expertise (medical oncology, radiation oncology, general surgery, and others), type of cancer they most commonly treated (multiple options available), average time of first patient visit, their hospital's reference population and percentage of cancer patients operated on (for surgeons only). Questions on SDM included:
Familiarity with the concept and its usefulness. To know their degree of familiarity with SDM, participants were asked whether they had received training in SDM, and about the extent of their knowledge of the subject. To assess the latter aspect, they could choose one of four options: I don't know anything about it; I have some idea about it; I know quite a lot about it but I don't use it in practice; I know a lot about it and I use it regularly. The usefulness of SDM was measured on a five-point Likert scale ranging from “not at all useful” (1) to “very useful” (5).
Perception of who should make the decision on treatment, and who really makes the decision: both aspects were evaluated according to the five points established by King15: Totally the patient; Mostly the patient; Both patient and physician equally; Mostly the physician; Totally the physician.
Assessing SDM. This was done with the Shared Decision Making Questionnaire-physician version (SDM-Q-Doc). Since this survey had not been validated in Spanish at the time of the study, a translated version, authorized by two of the authors of the scale (Martin Härter and Isabelle Scholl, of the University Medical Center of Hamburg-Eppendorf, Germany) was used16. This questionnaire contained nine items, each describing a step in the SDM process. Each item was scored on a six-point Likert scale ranging from “completely disagree” (0) to “completely agree” (6). The sum of the responses to the nine items generated a total score of between 0 and 45. To facilitate interpretation of the results, this score was multiplied by 20/9 to get a score of between 0 and 100, in which 0 was the lowest score and 100 the highest17.
Barriers and facilitators to implementing SDM. These were established based on a systematic review of the bibliography and were specified by the physicians involved in the study. To assess these two aspects, a six-point Likert scale was used ranging from “completely disagree” (0) to “completely agree” (5).
Statistical analysis
A descriptive analysis was made based on the frequencies of the variables of gender, age, years of experience, area of expertise, type of cancer most commonly treated, average time of first visit and reference population.
To determine whether there were differences between medical specialities in terms of familiarity, perception, assessment, and barriers and facilitators, various tests were applied, such as the χ2 association test, the Wilcoxon signed rank test, the Kruskal-Wallis H test, and the Mann-Whitney U test for independent samples with Bonferroni correction.
In order to analyse the orientation of the SDM-Q-Doc responses, and the barriers and facilitators to SDM, all possible answers were grouped in two categories: “Disagreement” and “Agreement”. The former included: “Completely disagree”, “strongly disagree” and “somewhat disagree”, while the latter included: “completely agree”, “strongly agree” and “somewhat agree”.
The software used was SPSS Version 20.0.
RESULTS
Clinical and socio-demographic profile
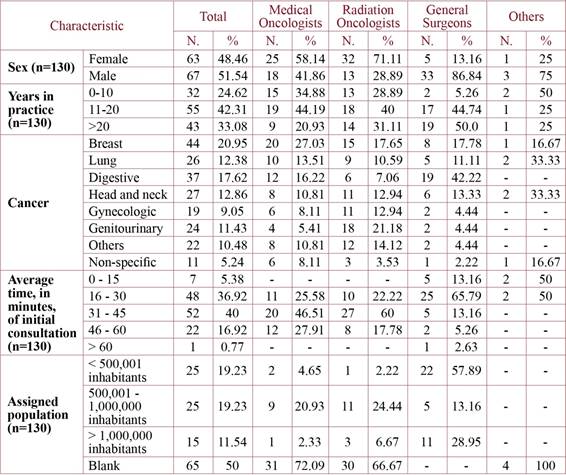
Of the potential 351 participants, there were 130 responses (a response rate of 37.04%). Of these, there were 63 women and 67 men, with an average age of 45.6 and an average of 18.04 years' experience. A total of 43 (33.08%) were medical oncologists, 45 (34.61%) were radiation oncologists, 38 (29.23%) were general surgeons and four (3.08%) came from other specialities (table 1). The latter, although they were registered in the lists of e-mail addresses of the scientific societies of medical oncologists, radiation oncologists and general surgeons, indicated that they belonged to other medical specialties.
In terms of type of cancer they most commonly treated, breast cancer was the most prominent, at 20.95%, followed by digestive/gastrointestinal tumours, 17.62%, and head and neck cancers at 12.86%.
On questions related to time dedicated to the patient on their first visit, 40% of the participants stated that they attended to the patient for between 31 and 45 minutes, and 36.92% between 16 and 30 minutes. Regarding the hospital reference population, 50% declined to answer, putting this group on a par (19.2%) with those who indicated a population of less than 500,001, and those with a reference population of between 500,001 and 1,000,000 inhabitants.
Shared decision making:
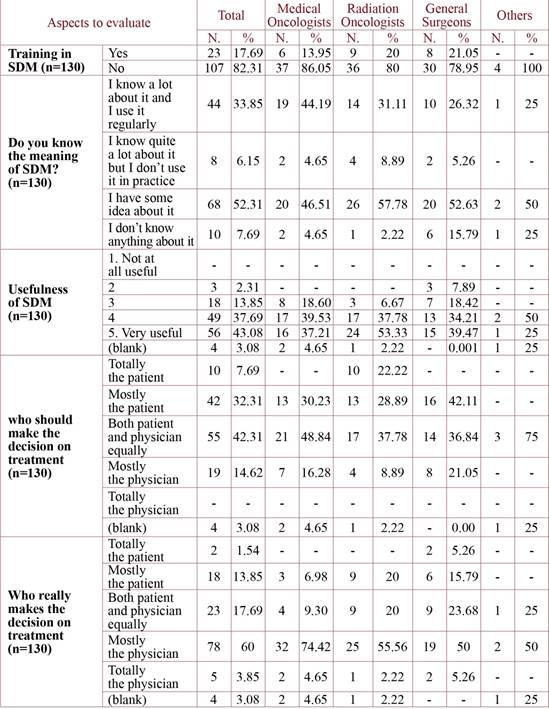
i) Familiarity and usefulness. When the participants were asked about their level of training in SDM, 82.3% stated that they had received no training in SDM while 17.6% stated that they had. A further 52.3% declared that they had some idea of the concept, and 33.8% said they knew quite a lot about it and regularly used this model in such cases (table 2).
Regarding the usefulness of SDM, 43% stated that it was very useful, marking it with a 5/5 on the scale, followed by 37.7% who gave it 4/5 (table 2). By speciality, the radiation oncologists considered it the most useful.
For level of SDM knowledge and usefulness, there were no significant differences between specialities.
ii) Perceptions of making the decision. Of the participants, 42.3% stated that any decision should be made equally between the patient and the physician, while 32.3% said it should mainly be the patient. None of those surveyed said the decision should be the physician's only (table 2).
However, when asked who, in practice, made the decision, 60% of the participants said that it was mostly the physician, followed by 17.69% who said decisions were made equally between physician and patient.
It is worth pointing out that only in 23% of cases was there any overlap between who should take the decision and who really made it, with only 11 clinicians (8.7%) stating that they thought the decision should be made jointly by both physician and patient, and that this was done in practice.
The medical oncologists were the ones who, in higher number, considered the decision should be made by the patient and the physician equally. However, 79.07% of them responded that the decision was made mostly or totally by them.
The Wilcoxon test (statistic -7.327 and p<0.01) revealed significant differences between who made the decision and who should have made it. However, there was no evidence of significant differences between specialities in the two cases.
iii) Assessing SDM. Of the 130 physicians who began responding to the questionnaire, only 126 completed the assessment the SDM process (table 3). As three of them belonged to other specialities, their responses were not studied as a group apart although their scores were taken into account in the totals. The results were predominantly for agreement, with scores exceeding 90% in all items, even reaching 100% in statements 3, 4 and 5. Only when we examine the responses by speciality do we find a slight dip.
Table 3. Assessment of shared decision making (SDM-Q-Doc, physician version). Percentage of agreement.

This highest transformed total was scored by radiation oncologists (88.99), followed by general surgeons and medical oncologists (table 4).
The Kruskal-Wallis test (χ2=13.032, p=0.01) revealed significant differences in the total scores for the variable corresponding to the SDM evaluation rate by medical speciality.
The Mann-Whitney U test with Bonferroni correction for independent samples showed that the perception of medical oncologists differed significantly from that of general surgeons and radiation oncologists, whereas there were no differences between that of general surgeons and radiation oncologists.
iv) Barriers and facilitators to SDM. Following the analysis of the barriers proposed in the questionnaire (table 5) (n= 124), the main barrier cited related to the difficulty patients had in understanding all that they needed to know (90.3%), followed by the lack of sufficient support resources to carry out proper SDM (87.9%), as well as not having enough time to discuss issues in detail with the patients (78.2%). There were no significant differences in the total scores for the variable corresponding to the barriers according to medical speciality.
Table 5. Barriers and facilitators to implementing shared decision making in oncology practice. Percentage of agreement.

If the adopted role is considered, the only barrier relating to who really made the decision was number 5, “the patients show no interest in collaborating in SDM” (χ2=8.715, p=0.013).
In terms of the SDM facilitators (n=124), the physicians' sense of motivation, their perception of improvement, both in the process itself and in the patients' results, and the patients' interest in collaborating in SDM, all boosted scores for agreement above 90%. The exception was the fact SDM was an institutional objective, which only 46.7% considered to be a facilitator for SDM.
There were no significant differences in total scores for the variables related to the facilitators according to medical speciality. The facilitators 1, 2 and 3 revealed significant differences per speciality.
DISCUSSION
The results of the questionnaire show that most of the participants, despite not having trained in Shared Decision Making, know what it was, and a big majority, regardless of medical speciality, stated that SDM was useful or very useful. This coincides with findings from Pollard, Bansback and Bryan18 in their systematic review of the subject, which showed a positive attitude towards SDM among clinical practitioners both in primary care and in specialist treatment, including oncology. Another study that focused exclusively on oncology19 also described a positive attitude towards SDM, as did the review by Kane et al3 which observed the interest shown by physicians in general, and oncologists in particular, in applying SDM to their patients.
The positive attitude towards, and recognition of the usefulness of SDM contrasts with the concerns on those surveyed regarding who should make the decision and who, in reality, makes that decision. It is noteworthy that a little under half (42.31%) thought that any decision ought to be taken equally between the physician and patient, and only 17.69% applied SDM in practice. On the other hand, more than half those surveyed thought that in reality it was the physician who made the decision in most cases. These scores are low when compared to results from a study of Dutch oncologists (surgical, radiation and medical)20, in which 95% declared that the patients should be involved in SDM, and 73% preferred to make a decision in collaboration with their patients.
However, factors that should be taken into account include the physicians' values and personal beliefs, their medical experience and type of medical practice, their perception of their patients' life expectancy, and style of communication, all of which can affect the decision-making process in oncology21. Furthermore, a review by Tariman et al21 on medical specialities showed that urologists opted more for surgery while radiation oncologists preferred radiotherapy when dealing with patients with localized prostate cancer.
Another investigation in Australia on the factors that influence oncologists when it came to facilitating SDM with patients, observed that oncologists' values and perceptions affected the extent of their support for SDM. Some believed that not facilitating patient participation in decision making was an act of arrogance, and that involving patients in decision making reduced patient anxiety. In contrast, various oncologists indicated that using SDM could lead the patient to make the wrong decision. But since they believed that the patients wanted treatments that gave them the best possible chance of survival, this tended to overrule oncologists' concerns about including them in the decision-making process. The oncologists also stated that the patients' characteristics influenced patient participation in any treatment decisions22.
The failure to put into practice a joint decision adopted by the physician and the patient that is revealed by our study contrasts with data obtained from the scores for SDM. In this case, the physicians considered that they complied with all the stages of the process, with percentages exceeding 90% for agreement with all the items, even reaching 100% for statements for 3, 4 and 5. We believe that the explanation for these high scores in the SDM-Q-Doc questionnaire, and hence the discrepancy, lies in the fact that the physicians are not familiar with SDM23 or that the scores were based on leniency and gratitude24. Nevertheless, the scores are similar to those in Calderón et al12, in which all the mean scores exceeded 4 on a scale of 0-5. In our case, statements 1 to 6 recorded a mean score higher than 4, although statements 7-9 had scores of between 3.85 and 3.95. The lowest scores were for statements 8 and 9: “My patient and I selected a treatment option together”, and “My patient and I reached an agreement on how to proceed”.
In terms of the barriers considered to undermine the usefulness of SDM, a considerable number of physicians stated that they acknowledged three of the eight barriers suggested, with percentages always higher than 78%. Two in particular, the lack of time and the difficulties experienced by patients in understanding what they need to know, have also been identified in significant systematic reviews on the issue, such as Gravel6, Légaré25 and Perestelo26.
It is also important to emphasize that the only barrier that related to who really makes the decision on treatment was the lack of interest shown by patients in collaborating in the SDM process (44.3% in agreement), which could be one of the main reasons why it is the physician who makes the decision on treatment.
In contrast, the physicians were unanimous in identifying the SDM facilitators, with percentages in all cases above 86%. The only proposal that the majority did not consider to be a facilitator of SDM was when this process became an institutional objective linked to economic incentives. Professional motivation to carry out SDM, physicians' perception of improvement in the health care process or patients' results were also cited as SDM facilitators in the systematic reviews by Gravel6, Légaré25 and Perestelo26.
Finally, it is important to emphasise that significant differences were only apparent between the medical specialities in their evaluation rates for SDM, in particular in the perception of the medical oncologists compared to that of the radiation oncologists and general surgeons.
The limitations of our study include that the fact that the conclusions cannot be generalized. The sample size is small and the research was carried out exclusively among health care professionals belonging to the Andalusian Health Service. Secondly, the SDM-Q-Doc questionnaire can be considered generic in its assessment of SDM, in that the items do not always reflect the physicians' situation, which could affect the way in which the survey is completed. In addition, when this study was underway, the Spanish version of the questionnaire for oncologists had not been validated (it was validated in 2017 by Calderón et al12). Another limitation refers to the taxonomies used for the barriers and facilitators to SDM. These had been established in accordance with a systematic review of the bibliography, and the opinions of the physicians involved in writing this work. Finally, this is a retrospective study, and the results could be subject to bias based on memory distortion and/or reinterpretation.
REFERENCES
1. Perestelo-Pérez L, Pérez-Ramos J, Rivero-Santana A, González-Lorenzo M. Toma de decisiones compartidas en oncología. Psicooncología. 2010;7:233-241 [ Links ]
2. Ernst J, Kuhnt S, Schwarzer A, Aldaoud A, Niederwieser D, Mantovani-Löffler L et al. The desire for shared decision making among patients with solid and hematological cancer. Psychooncology. 2011;20:186-193 [ Links ]
3. Kane HL, Halpern MT, Squiers LB, Treiman KA, McCormack LA. Implementing and evaluating shared decision making in oncology practice. CA Cancer J Clin. 2014;64:377-388 [ Links ]
4. Berger S, Braehler E, Ernst J. The health professional-patient-relationship in conventional versus complementary and alternative medicine. A qualitative study comparing the perceived use of medical shared decision-making between two different approaches of medicine. Patient Educ Couns. 2012;88:129-137 [ Links ]
5. Légaré F, Witteman HO. Shared decision making: Examining key elements and barriers to adoption into routine clinical practice. Health Aff (Millwood). 2013;32:276-284 [ Links ]
6. Gravel K, Légaré F, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals' perceptions. Implement Sci 2006;1:16 [ Links ]
7. Perestelo-Pérez L, Rivero-Santana A, Álvarez-Pérez Y, Alonso-Coello P, Orrego C, Serrano-Aguilar P. Shared decision making in Spain: Supportive policies and research initiatives, trends and directions for future. Z Evid Fortbild Qual Gesundhwes. 2017;123-124:85-90 [ Links ]
8. Arrighi E, Jovell AJ. El valor terapéutico en oncología. La perspectiva de los pacientes, familiares y profesionales. Barcelona: Publicaciones Universidad de los Pacientes Fundació Josep Laporte y Universitat Autònoma de Barcelona; 2009 [ Links ]
9. Arrighi E, Blancafort S, Jovell AJ. Evaluación de la Calidad de la Asistencia Oncológica en España. Barcelona: Publicaciones Universidad de los Pacientes Fundació Josep Laporte y Universitat Autònoma de Barcelona; 2008 [ Links ]
10. Padilla-Garrido N, Aguado-Correa F, Ortega-Moreno M, Bayo-Calero J, Bayo-Lozano E. La toma de decisiones compartidas desde la perspectiva del paciente oncológico: roles de participación y valoración del proceso. An Sist Sanit Navar. 2017;40:25-33 [ Links ]
11. Martín-Fernández R, Abt-Sacks A, Perestelo-Pérez L, Serrano-Aguilar P. Actitudes de las mujeres diagnosticadas de cáncer de mama frente a la toma de decisiones compartida. Revista Española de Salud Pública. 2013;87:59-72 [ Links ]
12. Calderón C, Ferrando PJ, Carmona-Bayonas A, Lorenzo-Seva U, Jara C, Beato C et al. Validation of SDM-Q-Doc Questionnaire to measure shared decision-making physician's perspective in oncology practice. Clin Transl Oncol. 2017;19:1312-1319 [ Links ]
13. Jimenez-Fonseca P, Calderón C, Carmona-Bayonas A, Muñoz MM, Hernández R, Mut Lloret M et al. The relationship between physician and cancer patient when initiating adjuvant treatment and its association with sociodemographic and clinical variables. Clin Transl Oncol. 2018; doi: 10.1007/s12094-018-1870-z. (Epub ahead of print) [ Links ]
14. Charles CA, Whelan T, Gafni A, Willan A, Farrell S. Shared Treatment Decision Making: What Does It Mean to Physicians? J Clin Oncol. 2003; 21: 932-936 [ Links ]
15. King VJ, Davis MM, Gorman PN, Rugge JB, Fagnan LJ. Perceptions of Shared Decision Making and Decision Aids Among Rural Primary Care Clinicians. Med Decis Making. 2012; 32:636-644 [ Links ]
16. Shared-decision-making.org. Cuestionario sobre la toma de decisiones compartida (SDM-Q-Doc). 2015. Disponible en: http://www.patient-als-partner.de/media/sdm-q-doc_spanish_version_final.pdf [ Links ]
17. De Las Cuevas C, Perestelo-Pérez L, Rivero-Santana A, Cebolla-Martí A, Scholl I, Härter M. Validation of the Spanish version of the 9-item shared decision-making questionnaire. Health Expect. 2015; 18: 2143-2153 [ Links ]
18. Pollard S, Bansback N, Bryan S. Physician attitudes toward shared decision making: A systematic review. Patient Educ Couns. 2015; 98: 1046-1057 [ Links ]
19. Brace C, Schmocker S, Huang H, Victor JC, McLeod RS, Kennedy ED. Physicians' Awareness and Attitudes Toward Decision Aids for Patients With Cancer. 2010. J Clin Oncol. 2010;28:2286-2292 [ Links ]
20. Pieterse AH, Baas-Thijssen MC, Marijnen CA, Stiggelbout AM. Clinician and cancer patient views on patient participation in treatment decision-making: a quantitative and qualitative exploration. Br J Cancer. 2008;99:875-882 [ Links ]
21. Tariman JD, Berry DL, Cochrane B, Doorenbos A, Schepp KG. Physician, patient, and contextual factors affecting treatment decisions in older adults with cancer and models of decision making: a literature review. Oncol Nurs Forum. 2012;39:E70-83 [ Links ]
22. Shepherd HL, Butow PN, Tattersall MH. Factors which motivate cancer doctors to involve their patients in reaching treatment decisions. Patient Educ Couns. 2011;84:229-235 [ Links ]
23. Santema TB, Stubenrouch FE, Koelemay MJW, Vahl AC, Vermeulen CFW, Visser MJT et al. Shared Decision Making in Vascular Surgery: An Exploratory Study. Eur J Vasc Endovasc Surg. 2016;51:587-593 [ Links ]
24. Stubenrouch FE, Mus EMK, Lut JW, Hesselink EM, Ubbink DT. The current level of shared decision making in anesthesiology: an exploratory study. BMC Anesthesiology. 2017;17:95-103 [ Links ]
25. Légaré F, Ratté S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: Update of a systematic review of health professionals´ perceptions. Patient Educ Couns. 2008; 73: 526-535 [ Links ]
26. Perestelo-Pérez L. Barreras y facilitadores para la implementación de la toma de decisiones compartidas en la práctica clínica: una revisión sistemática. Madrid: Ministerio de Ciencia e Innovación; 2010 [ Links ]
Received: March 26, 2019; Accepted: May 07, 2019; pub: October 09, 2019











 text in
text in