Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Anales del Sistema Sanitario de Navarra
versión impresa ISSN 1137-6627
Anales Sis San Navarra vol.32 no.3 Pamplona sep./dic. 2009
Comment on the clinical note: Acute necrotizing esophagitis in an unstable patient
Comentario a la nota clínica: Esofagitis necrotizante aguda en paciente inestable
Rodrigo M et al described a case of black esophagus (BE) in a 77-year-old male who developed severe hemodynamic instability, and BE was cited as rare condition1. The mentioned report is very interesting and well documented, but additional comments and illustrations from the study of a brazilian patient with coexistent BE and candidiasis could be appropriate to emphasize concerns about frequency rate and associated factors.
Although ischemic factors can play a pathogenic role, hemodynamically stable patients have presented with BE too. Worth of note, only about a hundred cases of this entity were reported since the first description in 19901-4; notwithstanding, published necropsy data are suggestive that BE may be under diagnosed and/or under reported2,5. The aim of the present paper is to enhance the suspicion index about BE, which will have better outcome if early diagnosis and precocious treatment can be accomplished.
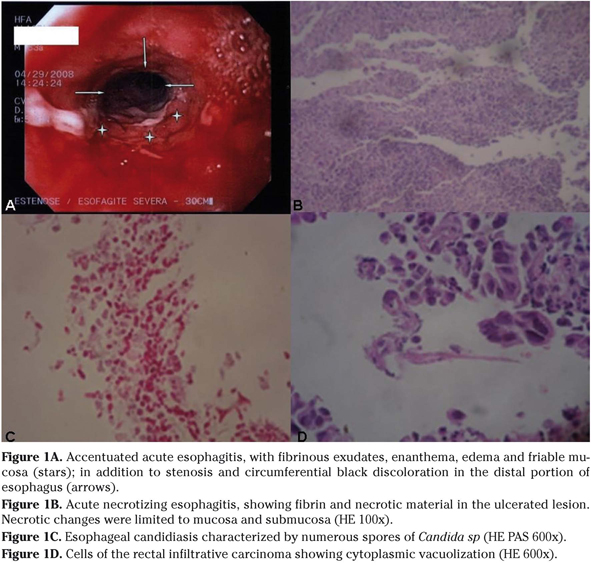
An 83-year-old male was admitted because of hypoglycemia, vomiting, dysphagia, and weight loss. He was in use of NPH insulin and furosemide to treat diabetes and hypertension and there was antecedent of an advanced invasive rectal cancer. The endoscopy study detected mild stricture, ulceration and black discoloration in distal esophagus (Fig. 1A), in addition to duodenal ulcers. Esophageal biopsy samples showed characteristic features of acute esophageal necrosis and ulcerated esophagitis (Fig. 1C), coexistent with local accentuated moniliasis (Fig. 1D). Rectosigmoidoscopy revealed an ulcerated infiltrative rectal tumor at 3cm from the anal limit, affecting ¾ of the lumen. The diagnosis of rectal carcinoma was confirmed by biopsy (Fig. 1D). TC showed perirectal invasion and liver implants. Remarkable laboratory data were hypoalbuminemia, accentuated anemia and leukocytosis with neutrophilia, in addition to hyponatremia and high platelet count1-4. These changes can be found in acute phase response (APR) and protein-energy malnutrition (PEM)6,7. He received gastric protection, total parenteral nutrition and intravenous fluconazole. Even with clinical improvement, the patient refused treatment for advanced cancer. After gastrostomy done because of esophageal stenosis, he was referred to home-care support.
In spite of the malignant co morbidity and indicative features of APR and PEM, there was no circulatory instability, and the clinical evolution was favorable. Wallberg et al. reported similar favorable outcome of BE in a 75-old-year patient with sepsis4, which is a major cause of systemic inflammatory response and circulatory failure. Common clinical features are dyspepsia, epigastralgia, hematemesis, melena, and vomiting, but the diagnosis suspicion of BE during endoscopy must be further confirmed by histological data. Circumferential black discoloration is often seen in distal esophagus, with mucosa erosions, ulcers, exudates, necrosis and vessel thrombi1-4. Differential diagnosis of BE includes acanthosis nigricans, melanoma, melanosis, pseudomelanosis, ocronosis and necrotic lesions due to caustic or corrosive agents1-4.
Risk factors for BE include alcoholism, cardio circulatory disorders, pulmonary diseases, cirrhosis, diabetes, esophagitis, gastric obstruction, hiatal hernia, malignancies, malnutrition, and renal failure1-4. Interestingly, esophageal candidiasis or rectal cancer are associations very rarely reported. Malignancies found in patients with BE are: cancers from colon, biliary tract, hypofarynx, lung, ovary, pancreas, prostate, and rabdomyosarcoma. Esophageal stricture is the major complication2,4.
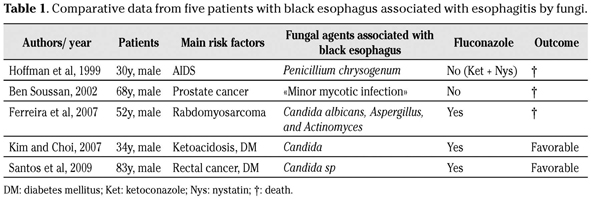
Coexistent BE and candidiasis should be better cleared because: reports about this association are rare5,8,9; endoscopy disclose esophageal candidiasis in 1-8% of all patients examined10; fungi may be opportunistic agents in immunocompromised individuals8-10, including those with APR and PEM associated with cancer or AIDS5,8,9. As occurred in the present case, the esophageal changes may undergo favorable resolution after management with proton pump inhibitors, sucralfate, and nutrition care, in addition to treatment of associated infections (Table 1).
As necropsy data have suggested that BE can be under diagnosed, case reports and letters to the editor could increase the awareness about this disorder.
V.M. Santos1,2, R.B. Villaça3, I.P. Gouvêa4, D.A.R. Sá2
1. Catholic University Medical Course.
2. Department of Internal Medicine from Armed Forces Hospital (HFA). Estrada do Contorno do Bosque s/n, 70.603-900. Brasília-DF. Brazil.
3. Department of Gastroenterology from HFA.
4. Department of Pathology from HFA.
References
1. Rodrigo M, Gorraiz BE, Merino C, Eguaras J, Elizalde JM, Soler W. Esofagitis necrotizante aguda en paciente inestable. An Sist Sanit Navar 2009; 32: 113-116. [ Links ]
2. Julián Gómez L, Barrio J, Atienza R, Fernández-Orcajo P, Mata L, Saracíbar E et al. Acute esophageal necrosis. An underdiagnosed disease. Rev Esp Enferm Dig 2008; 100: 701-705. [ Links ]
3. Ramos R, Mascarenhas J, Duarte P, Vicente C, Casteleiro C. Acute esophageal necrosis: a retrospective case series. Rev Esp Enferm Dig 2008; 100: 583-585. [ Links ]
4. Wallberg ME, Young P, Finn BC, Thomé M, Chueco AA, Villarejo F. Esófago negro secundario a esofagitis necrotizante aguda. Reporte de un caso clínico. Rev Méd Chile 2009; 137: 672-674. [ Links ]
5. Ben Soussan F, Savoye G, Hochain P, Hervé S, Antonietti M, Lemoine F et al. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc 2002; 56: 213-217. [ Links ]
6. Monteiro JP, Cunha DF, Da cunha SF, Dos santos VM, Silva-Vergara ML, Correia D et al. Resposta de fase aguda, subnutrição e estado nutricional do ferro em adultos com AIDS. Rev Soc Bras Med Trop 2000; 33: 175-180. [ Links ]
7. Santos VM, Cunha SF, Cunha DF. Velocidade de sedimentação das hemácias: utilidade e limitações. Rev Assoc Med Brasil 2000; 46:232-236. [ Links ]
8. Ferreira S, Claro L, Sousa R, Vitorino E, Lage P, Chaves P et al. Esófago negro associado a infecção por Candida albicans, Aspergillus e Actinomyces. J Port Gastroenterol 2007; 14: 143-146. [ Links ]
9. Hoffman M, Bash E, Berger AS, Burke M, Yust I. Fatal necrotizing esophagitis due to Penicillium chrysogenum in a patient with acquired immunodeficiency syndrome. Eur J Clin Microbiol Infect Dis 1992, 11: 1158-1160. [ Links ]
10. Kim YH, Choi SH. Black esophagus with concomitant candidiasis developed after diabetic ketoacidosis. World J Gastroenterol 2007; 13: 5662-5663. [ Links ]
 Correspondence:
Correspondence:
Vitorino Modesto dos Santos
SMPW Quadra 14, Conjunto 2, Lote 7, Casa A
Setor de Mansoes Park Way, 71745-140
Brasília-DF. Brazil
Tfno. (0xx55) 61 33802666
Fax (0xx55) 61 32331599
E-mail: vitorinomodesto@gmail.com