INTRODUCTION
The Department of Corrections is responsible for protecting the inmates life, safety and health and therefore provides healthcare coverage corresponding to the level of primary healthcare. The General Act on Healthcare guarantees the rights of inmates and their access to healthcare in a basis of effective equality. Therefore, the public Administration is responsible for organizing and implementing all preventive and assistance measures within a concept of a comprehensive health system1. Each correctional facility counts upon primary health teams including physicians, nurses and auxiliary nurses, in variable number depending on its size and that of the population it hosts. Some facilities also have pharmacists and Radiology technicians. Despite healthcare services depending on the Department of Corrections (IIPP in Spanish) are part of the National Health System (MHS), which means that are integrated within the public network with access to tests and the posibility of referral, the healthcare staff of correctional facilities depends both organically and functionally on the Ministry of the Interior, except in those autonomous communities where this competence has been transferred. The organization of this part of the Public Health System has been scarcely addressed in technical forums and has become more relevant throughout recent years when the European Union opened the discussion on whether this should be managed by the Health admi nistration or the correctional administration2,3. This paper intends to improve the understanding on this part of public health, by comparing a series of healthcare indicators among correctional facilities: one of which has been transferred to Osakidetza, the Basque Health System, and the rest with healthcare services within the department of corrections.
In our country, legislators have granted IIPP the role of healthcare authority responsible for the physical and mental health of those hosted within correctional facilities, as well as the maintenance of appropriate hygiene and health conditions of the establishments themselves1. However, this responsibility does not to entail that they should be responsible for the organization of healthcare in prisons. The World Health Organization (WHO) established in its 2003 Moscow Declaration the need to establish close links between public Cohesion and Quality of the NHS4. It opened the way for prison healthcare services to be transferred to the corresponding autonomous community to be fully integrated in their public health system, something which has only taken place in the Basque Country as of July 20115 and in Catalonia as of September 20146.
Therefore, today in all the remaining autonomous communities, the organization of prison health services depends both organic and functionally on the department of corrections, a non-health administration, with a mission and a vision focused more on safety and control than on the management of healthcare provisions for inmates, which is perfectly understandable on the other hand.
The aim of this study is to describe and analyze the differences between the processes and the results of healthcare provision according to what administration is in charge of organizing prison health services: the community or the department of corrections. Therefore, we intend to compare the processes and use of services in the facilities under study, measured through predefined indicators.
MATERIAL AND METHODS
We have analyzed the differences in the provision and use of services of a prison transferred to the community health system and other four facilities dependent on the department of corrections (IIPP).
It is a cross-sectional descriptive study where the study unit is the prison itself. We have used general data on each facility and under no circumstances do they depict individuals. The facilities have been chosen according to a criterion of convenience. We have compared a prison of the Basque Country autonomous community with other four facilities with similar characteristics from other parts of the country, whose healthcare administration depends on the Ministry of the Interior.
All prisons in this study host a mean population of under 400 inmates, with a mean stay (rotation) of over 200 days, with similar social and age-related characteristics and with similar healthcare teams with regard to their provision and functioning.
Data has been collected from the Monthly Health Statistics Record of the department or corrections corresponding to the period between 2013 and 2014.
From that data, we have created a series of indicators (see Table 1) according to the recommendations of the NHS, consulted by the Ministry of Health, Social Services and Equality7. Moreover, we have consulted the indicators recommended by the National Institute of Statistics and the Basque Institute of Statistics.
Table 1 Analysed indicators.
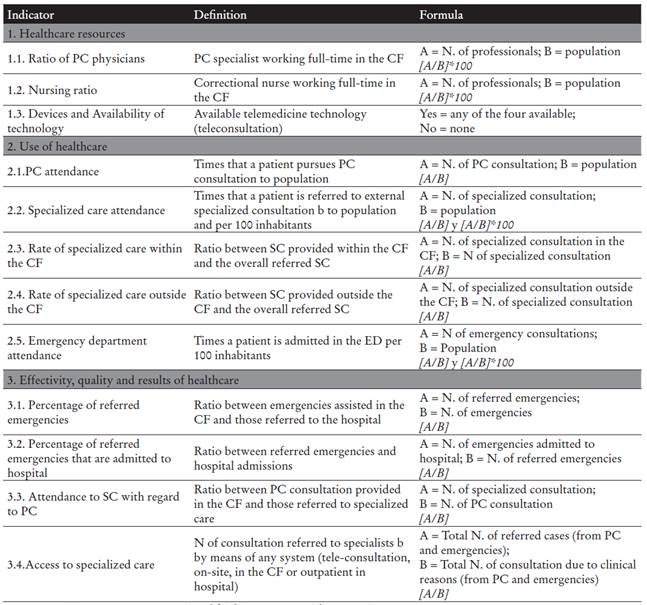
Note. PC: primary care; CF: correctional facility; IIPP: Spanish Corrections Department.
aPC consultation: overall consultations within the CF: on demand, scheduled or regimental.
bConsultations referred to specialists= overall number of each speciality, first visits or annual revisions in hospital, specialization centers or the CF itself. Does not include tests, dentistry visits, rehabilitation sessions, hemodialysis or radiotherapy sessions.
Statistical analysis
The data and indexes from the transferred facility have been compared to those of the facilities dependent of IIPP. Thus, we have calculated the difference between the index of each prison and that of the transferred establishment. To determine whether the difference was statistically significant Student’s t test has been used.
Moreover, we have assessed individual differences between IIPP-dependent institutions and the transferred prison, by comparing proportions with the chi-squared test.
In all cases statistical significance was defined for p<0.05. All analysis was done by means of R statistical software, version 3.2.1.
RESULTS
In 2014, the facilities included in our study had an average yearly population of 300 inmates: over 85% were men8. Table 2 depicts the features of each facility.
Table 2 Healthcare resources and its use within each correctional facility.

Note. CF: correctional facility.
The results of the differences between each facility with regard to the transferred facility are shown in Table 3. The values of the different indexes in each establishment can be consulted in Figures 1 to 3, where the p-value shows the contrast between prisons with the transferred facility as a reference.
Table 3 Differences in healthcare resources and their use in the transferred facility and the resto of correctional facilities.
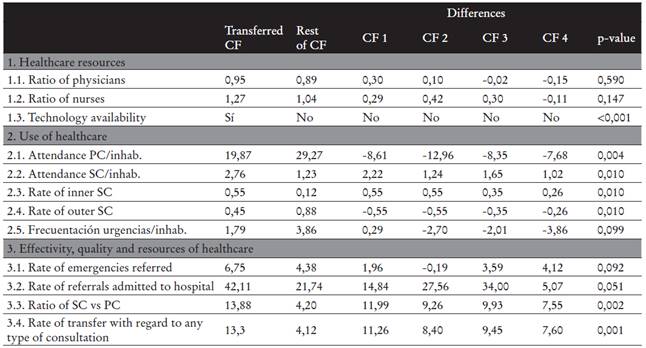
Note. PC: primary care; SC: specialized care; CF: correctional facility; inhab: inhabitant.
*Resto f CF: shows the mean index for the non-transferred facilities; Differences refers to the difference between the corresponding facility and the transferred establishment; p: refers to the contrast of differences.
With regard to the availability of healthcare resources, the physician-nurse ratio per inmate is higher in the transferred facility, yet this difference lacks statistical significance. When comparing the different centers (Figure 1), only one offers a higher ratio that the transferred center, both regarding medical and nursing staff. Regarding the access to technology, only the transferred establishment counts upon telemedicine resources.
The use of resources (Figure 2) also presents differences, statistically significant in this case. The mean attendance to primary health services in non transferred facilities is higher in all cases (p=0.004) while attendance to specialized consultation in the transferred facility doubles that of the other prisons (p=0.010).
From the transferred facility, referral to the emergency department in hospitals is usually higher than in all non-transferred centers except for one (Figure 3).

Figure 3 Differences between facilities with regard to effectivity, quality and results of healthcare.
The percentage of referred emergencies that are finally admitted in hospital is significantly higher in the transferred facility doubling the mean rate of the other establishments. There is also a significant difference regarding the rate of scheduled referrals to specialized consultation services, which is higher in comparison with non-transferred prisons.
DISCUSSION
Prison health has some particularities mainly determined by a higher proportion of pathology in comparison with that of the community on one hand, and by the structural environment where healthcare has to be provided, in a context of isolation and control, on the other. The term “primary health” can not fully define the work of healthcare providers in the correctional setting. In fact, the work of healthcare providers is included within that carried out by other professionals, in charge of the safety and the general organization of the establishment9. Prison healthcare providers contribute by means of their medical-legal aspect, so needed in a facility ruled by the Administration of Justice.
A prison ultimately exists to perform measures of deprivation of liberty, and this fact further defines the rest of services that may be provided within specially including health services, which are therefore differentiated from any other assistance resource, whereas in the community they are dedicated to the assistance of patients10.
We must therefore not forget that prisons are a device of contention and their main aim is not the provision of healthcare for inmates, but their custody. This obviously has an impact on the conditions under which healthcare providers work, regardless of the prison being included in a community system like in the Basque Country or not. With regard to Law, only the General Prisons Organic Law in Spain1 and in the European Council in the EU by means of a recommendation which is not legally binding, make a reference to the provision of healthcare in prisons11.
The imprisoned population has a higher rate of social, family and both physical and mental health-related issues in comparison with the general population in the same age ranges. This is mainly due to the fact that most inmates come from more socially isolated and vulnerable groups. Around 50% have a recent background of drug use, 4% have a severe mental disorder12 and chronic diseases such as diabetes, epilepsy, oral and dental issues, coronary artery disease or asthma are also more common among inmates than in the community. With regard to communicable disease, the rates of tuberculosis infection, HIV (human immunodeficiency virus) infection, HCV (Hepatitis C) infection and sexually transmitted diseases are also higher among the imprisoned population13,14.
From our results, we can conclude that the facilities included in our study are equivalent with regard to their structural characteristics and healthcare needs. There are no significant differences regarding the mean number of inmates nor the human resources that they count upon in terms of healthcare providers (medical and nursing staff). They belong to diverse geographical areas, and thus functioning circumstances determined by their localization are mitigated.
The first remarkable result when comparing the transferred facility and non-transferred establishments, is the lower attendance rate to primary health consultation and the higher referral to specialized consultation. This is evident possibly because access to specialized care is enhanced in an integrated structures where the organization of services includes both primary and specialized care. In this case, the transferred facility ensures an improved continuity between different healthcare services, when compared to establishments where primary and specialized care depend on different institutions with no administrative nor functional relationship.
With regard to referred emergencies from the transferred facility, the fact that most are finally admitted in hospital probably is due to a correct assessment by the prison health team and this reveals further healthcare quality in comparison with the other prisons, where the admission rate is significantly lower. There is also an enhanced presence of computer-based communication technology between the prison and the rest of he public health system in the transferred facility.
Chronic pathologies that require specialized care are further covered when an appropriate continuity between the primary and secondary levels is ensured. The rates of specialized consultation in this facility are higher and more efficient than in the rest of prisons. This is not related with an increased pressure on primary care services since that is not higher in the transferred facility but it is related to an improved access to specialized care. In prisons managed by the department of corrections, access to hospital and specialized care is more difficult and inefficient, mainly because each level is managed by a different entity: IIPP manages healthcare in prison and specialized ad emergency services in hospitals are managed by each autonomous community. This all translates into a reduced rate of scheduled specialized consultation and an increased rate of emergency attendance without the cases requiring hospital admission. Some authors could think that there is a contradiction when considering a greater rate of referred specialized as a quality result. We have to consider that prion health services traditionally suffer from organization diffi culties when accessing the specialized level and thus, the high rate of referred emergencies to hospital. This is the way to counteract the difficulty of regulated referrals that IIPP managed prison physicians encounter. This also explains why the referred emergencies have a lower admission rate than those of the transferred facility, which counts upon an improved integration and transfer protocols, enhanced access to specialized consultation and to the emergency department when needed. Therefore, in this case, a higher attendance to specialized care does not entail a low degree of resolution but improved continuity of care. It is true, however, that higher rates of referred specialized do not necessarily imply an improved coordination, but obviously a lower rate of scheduled specialized consultation together with a higher rate of referred emergencies reveal poor coordination between levels of care.
It is worth considering that with regard to structural and population characteristics, out of the sixty-six facilities of the IIPP network that were available, we have chosen those that were more similar to the transferred facility in terms of population, architecture, inmate rotation and healthcare resources. When referring to telemedicine, we have considered the availability of tele-consultation or specialized virtual consultation.
A limitation of the methodology in this study is the source of data, where it is difficult to ensure a lack of classification bias due to potential under-report or transcription mistakes. It would be therefore recommendable to carry out similar studies with bigger samples as to check the conclusions that have been drawn.
Efficiency, one of the main requirements of any health management model, is essential in the correctional setting, since the constant increase of costs and the expectation of an improved health status among inmates in a setting where recovery from disease is far from optimal, further adds pressure on prison health services4.
In the systematic revision of scientific literature on prison health there is a lack of articles on functioning indicators and therefore, this is a pioneer study in Europe for the assessment of indicators and their comparison between two different models. It alto so contributes to cover a need that the WHO has stated publicly: “to fight against the lack of knowledge on the status of prison health and its relevance for public health in the society and among many of its stake holders”. Accurate knowledge of the health needs of inmates, many of whom belong to vulnerable social groups, should be a priority for the organization of health care services in each country2.
In an increasing number of European countries, the provision of prison healthcare is a responsibility of the Ministry of Health. In Europe, the integration of prison health in public health administrative structures is a reality but also a slow process. Experts have stated the “strong evidence” in terms of long-term benefits of the integration of prison health within public health systems, such as for example: improved public health both inside and outside prisons, a strong contribution in the fight against inequality in terms of health and even a role in reduced re-offence rates4. However, it is also noted that this process entails a series of difficulties including social rejection, legal complexity and difficult administrative and budgetary suitability.
Prison healthcare services in Europe have progressively grown throughout the years, empirically and pragmatically without any real planning to meet the needs of its users. In Spain, by law (LOGP), it should be the NHS providing healthcare for the imprisoned population and only exceptionally should private services be hired, when the NHS can not face a specific need. The data hereby presented are also aimed at an improved future planning of this type of care within the NHS2.
It would be desirable that this type of studies be replicated with bigger samples as to provide a stable model of care for the imprisoned population.
In this study we have observed an improved access to specialized care in the facility included in the community health system. This is based on a series of effectivity and outcome indicators that have provided significantly better results in this prison.
Currently, at a time when advances in the field of healthcare occur at break-neck speed, to stay aside of a healthcare organization with all its diagnostic, therapeutic and educational potential is a handicap for healthcare providers and for the work that they develop3.
The conclusion is that when prison healthcare is provided by means of a community public health system is of a higher quality due to an improved continuity of care and a broader availability of technical and educational resources. This makes us conclude that a change in the management model of prison health would improve the healthcare provided to inmates.
















