Introduction
Concentration and transmission of tuberculosis (TB) within high-risk populations, especially prisoners, is a major challenge to successful TB control worldwide1. In 2010, the average TB notification rate in correctional facilities in Europe was 1,055 per 100,000 inhabitants, 23 times that of the general population2-4. Prisons have served as the epicenters of outbreaks of rifampicin-resistant (RR) TB and, in some settings, they persistently host high rates of RR-TB4 5. To improve the epidemiological situation in penitentiary systems, the World Health Organization (WHO) recommends systematic performance of mass screening among inmates and passive case finding, i.e. detecting TB among symptomatic individuals, who seek for healthcare in prisons6 7. In parallel, the programs are advised to include rapid diagnostic tests for TB like Xpert MTB/RIF and liquid culture for detection of TB6 7. However, today, there is limited evidence to demonstrate that the inclusion of rapid diagnostic tests into mass screening or passive case finding algorithms along with the associated financial load is justified by a significant reduction of the burden of TB in prisons. Major heterogeneity in TB case finding approaches has emerged in prisons worldwide8 9.
According to the WHO, the estimated TB incidence rate and related mortality in Azerbaijan in 2016 was 66 and 0.28 per 100,000 inhabitants, respectively2. Also, the TB notification rate among inmates is 26 times that of the general population4. The aim of our case-case control study was to evaluate the impact of mass screening and passive case finding to the notification and treatment outcomes of TB in high TB/RR-TB burden prisons of Azerbaijan before and after the introduction of rapid diagnostic tests to the mass screening and passive case finding algorithms. The study took an advantage of a comprehensive TB program run by the Main Medical Department of the Azerbaijan Ministry of Justice, which has been recognized as a best practice for TB/RR-TB management in prisons10-12.
Matherials and methods
Study population
The study included all new and relapse cases of TB notified in all nineteen prisons of Azerbaijan during the period between January 2009 and December 2015. Cases of re-treated TB, other than relapses and cases identified at the pre-trial facilities, were excluded. During the study period, the population in prisons in Azerbaijan was stable, being on average 173 per 100,000 inhabitants. The study protocol was approved by the Bioethics Committee of the Ministry of Health of Azerbaijan.
Definitions and case finding algorithms
Passive case finding was defined as detection of TB among people seeking care in a health care facility6. Mass screening signified regular screening of the whole population to identify cases with TB7.
Prior to 2009, TB identification was not performed in a systematic way in prisons. In January 2009, annual mass screening was launched in the correctional facilities, consisting of a standardized five-symptom TB questionnaire (cough, sputum production, and subjective weight loss, loss of appetite or chest pain) and chest radiography (Figure 1).

Figure 1 Algorithms of TB case finding used in the correctional facilities of Azerbaijan during the whole study period, 2009-2015.
If any of the five TB symptoms were present or any relevant radiographic abnormalities were detected (irrespective of whether the abnormalities were considered suggestive of active or inactive TB), a single sputum sample was collected and tested by smear microscopy. Patients with a positive microscopy result were isolated and referred to the prison TB hospital for further diagnosis and treatment. During the same period, identification of presumptive TB cases by passive case finding was based on the presence of cough for >2 weeks. Such cases were isolated and referred to the prison TB hospital for further diagnosis and treatment. In context of the current study, this period from January 2009 to December 2011 is defined as a pre-intervention period.
From January 2012, sputum samples from all presumptive TB cases identified by the presence of any TB symptom or any abnormality suggestive of TB on chest radiography during the annual mass screening were tested by liquid culture, based on the Mycobacterium Growth Incubator Tubes (MGIT). Patients with positive culture result were referred to the prison TB hospital for treatment. During the same period, the passive TB case finding was done through identification of cases with cough for >2 weeks with the following Xpert MTB/RIF testing. Patients with positive Xpert MTB/RIF results were also referred to the prison TB hospital for treatment. For the current study, this period from January 2012 to December 2015 is defined as a post-intervention period. The participation rate for mass screening was between 97% and 98% during all the study period. Additionally, during the post-intervention period, the inmates admitted to the non-TB prison hospitals were screened using standardized five-symptom questionnaire and chest radiography. In cases, where any TB symptom was present or any radiographic abnormalities were detected, sputum was tested with Xpert MTB/RIF, followed by reference to the prison TB hospital in case of positive test result. We should also consider that the research of contacts was carried out within passive case finding during the whole study period.
Laboratory tests
All tests were performed at the laboratory network of Azerbaijan Penitentiary System (PS), which implements all WHO-recommended laboratory diagnostic tests for TB13. External quality control for this laboratory system has been provided by the Supranational Reference Laboratory in Borstel, Germany since 200714.
Treatment
Treatment strategies employed at the Azerbaijan PS have been described elsewhere 10 and were unchanged during the whole study period. In brief, all inmates, as soon as they were diagnosed with TB, received free standardized treatment with first-line drugs (FLD), i.e. isoniazid, rifampicin, pyrazinamide and ethambutol for drug-susceptible TB or individualized treatment with second-line drugs (SLD) for RR-TB in accordance with the WHO recommendations15. Linezolid, clofazimine, bedaquiline and delamanid were not available during the course of the study.
Data collection and analysis
The data from screening reports, medical charts and bacteriological laboratory reports were entered into the Azerbaijan PS TB registry database (EpiInfo 6.04d, Atlanta, Georgia, USA). The following variables were transferred and used for the current study: 1) sputum smear microscopy results, rifampicin (RIF) resistance and body mass index (BMI) from the point of diagnosis; 2) time and type of case detection; 3) treatment outcomes with FLD and SLD.
Linear regression, binary logistic regression and multinomial logistic regression analyses were used to compare the periods for the key data, as well as to perform within-period analyses. Variables like age, gender, duration of imprisonment, smoking, education levels, foreign nationality, as well as the type of correctional facility were not used for adjustment in logistic regression models, since they were found to be insignificant during the crude analysis. Statistical analysis was performed using STATA SE software (version 12, StataCorp, College Station, Texas, USA).
Results
A total of 2,315 patients with TB were identified in the 19 prisons of Azerbaijan during the study period: 1,799 (77.7%) new and 516 (22.3%) relapse cases, respectively. Among these, 1,032 (44.6%) were smear-positive, 307 (13.3%) were RIF-resistant and 380 (16.4%) occurred among individuals with BMI<18.5 kg/m2 at the diagnosis.
During the pre-intervention period, 709 (55.4%) of 1,280 TB patients were identified by passive case finding, while the remainder (571 patients, 44.6%) were identified through mass screening (Table 1). During the post-intervention period, 1,035 TB patients were detected: 445 (42.9%) by passive case finding, 469 (45.3%) by mass screening, and 121 (11.7%) by screening at entry to the non-TB prison hospital.
Table 1 Comparisons between the period, when the rapid tests for detection of TB (Xpert MTB/RIF and liquid culture) were introduced into mass screening and into passive case finding (post-interventional period), and the preceding period (pre-interventional period) for the overall number of identified smear-positive TB cases, RIF-resistant cases and those with BMI<18.5 kg/m2 at the diagnosis and the number of identified smear-positive TB cases, RIF-resistant cases and those with BMI<18.5 kg/m2 identified by mass screening and passive case finding. The aim was to show the impact of the inclusion of the rapid tests on the TB burden in the correctional facilities (Azerbaijan, 2009-2015).
| Pre-interventional period (2009-2011, n=1,280*) |
Post-interventional period 2 (2012-2015, n=1,035*) |
OR (CI 95%) | P value | aOR (CI 95%) | P value | |
|---|---|---|---|---|---|---|
| Smear-positive TB cases | 609 (47,6) | 423 (40,9) | 0,76 (0,64-0,89) | 0,001 | 0,80 (0,68-0,96)*** | 0,014 |
| RIF-resistant TB cases | 200 (15,6) | 107 (10,3) | 0,62 (0,48-0,80) | <0,001 | 0,66 (0,51-0,85)*** | 0,001 |
| With additional resistance to second-line injectables | 12 (0,9) | 13 (1,3) | 2,16 (0,82-5,70) | 0,117 | 1,53 (0,74-3,14) | 0,246 |
| With additional resistance to fluoroquinolones | 3 (0,2) | 12 (1,2) | 13,0 (1,70-99,3) | 0,013 | 4,38 (1,59-12,00) | 0,004 |
| Extensively drug resistant TB | 2 (0,2) | 9 (0,9) | 17,1 (0,74-99,7) | 0,203 | 4,15 (0,74-23,33) | 0,105 |
| Cases with BMI<18.5 | 240 (18,8) | 161 (15,5) | 0,79 (0,64-0,99) | 0,044 | 0,83 (0,67-1,04)*** | 0,105 |
| Mass screening€ | 571 (44,6) | 469 (45,3) | - - | - - | - - | - - |
| Smear-positive TB cases | 191 (14,9) | 160 (15,5) | - - | - - | 1,04 (0,80-1,36)**** | 0,737 |
| RIF-resistant TB cases | 57 (4,4) | 43 (4,1) | - - | - - | 0,92 (0,60-1,40)**** | 0,714 |
| Cases with BMI<18.5 | 78 (6,1) | 41 (4,0) | - - | - - | 0,60 (0,40-0,90)**** | 0,015 |
| Passive case finding****** | 709 (55,4) | 445 (43,0) | - - | - - | - - | - - |
| Smear-positive TB cases | 418 (32,7) | 202 (19,5) | - - | - - | 0,61 (0,49-0,79)***** | <0,001 |
| RIF-resistant TB cases | 143 (11,2) | 54 (5,2) | - - | - - | 0,62 (0,44-0,87)***** | 0,006 |
| Cases with BMI<18.5 | 162 (12,7) | 93 (9,0) | - - | - - | 0,96 (0,73-1,05)***** | 0,156 |
Note. aOR: adjusted odds ratio; BMI: Body mass index; RIF: Rifampicin; TB: Tuberculosis; IUsed for calculation of percentages in the respective column; IIUsed for calculation of the percentages in the respective column; IIIAdjustment was made to the overall number of smear-positive cases, RIF-resistant cases and those with BMI<18.5 kg/m2 at the diagnosis; IVAdjustment was made to the number of smear-positive cases, RIF-resistant cases and those with BMI<18.5 kg/m2 diagnosed by mass screening; VAdjustment was made to the number of smear-positive cases, RIF-resistant cases and those with BMI<18.5 kg/m2 diagnosed by passive case finding; VIDuring mass screening at the pre-interventional period presumptive TB presenting any TB symptom based on standardized five-symptom questionnaire and/or any abnormality compatible with TB on chest radiography were tested with smear microscopy, while in post-interventional period smear microscopy was substituted by liquid culture. VIIPassive case finding during the pre-interventional period identified presumptive TB cases based on presence of cough continuing for longer than two weeks, while in post-interventional period presumptive TB cases were identified based on presence of cough continuing for longer than two weeks and following Xpert MTB/RIF testing. Multivariate binary logistic regression analysis was used to identify the difference between the periods for the overall number of smear-positive cases, RIF-resistant cases and those with BMI<18.5 kg/m2 at the diagnosis, as well as to identify the difference between the periods for the number of smear-positive cases, RIF-resistant cases and those, with BMI<18.5 kg/m2 detected by mass screening and passive case finding.
During the post-intervention period, there were significant linear trends towards decrease in the annual rates of the notified (p=0.009), smear-positive (p=0.011) and RIF-resistant TB cases (p=0.02). The annual rates of decrease (95% confidence limits) were -435 (-614; -255), -356 (-517; -195) and -99 (-160; -38), respectively (Figure 2). No significant trends were present for any of these variables during the pre-interventional period of the study (Figure 2).
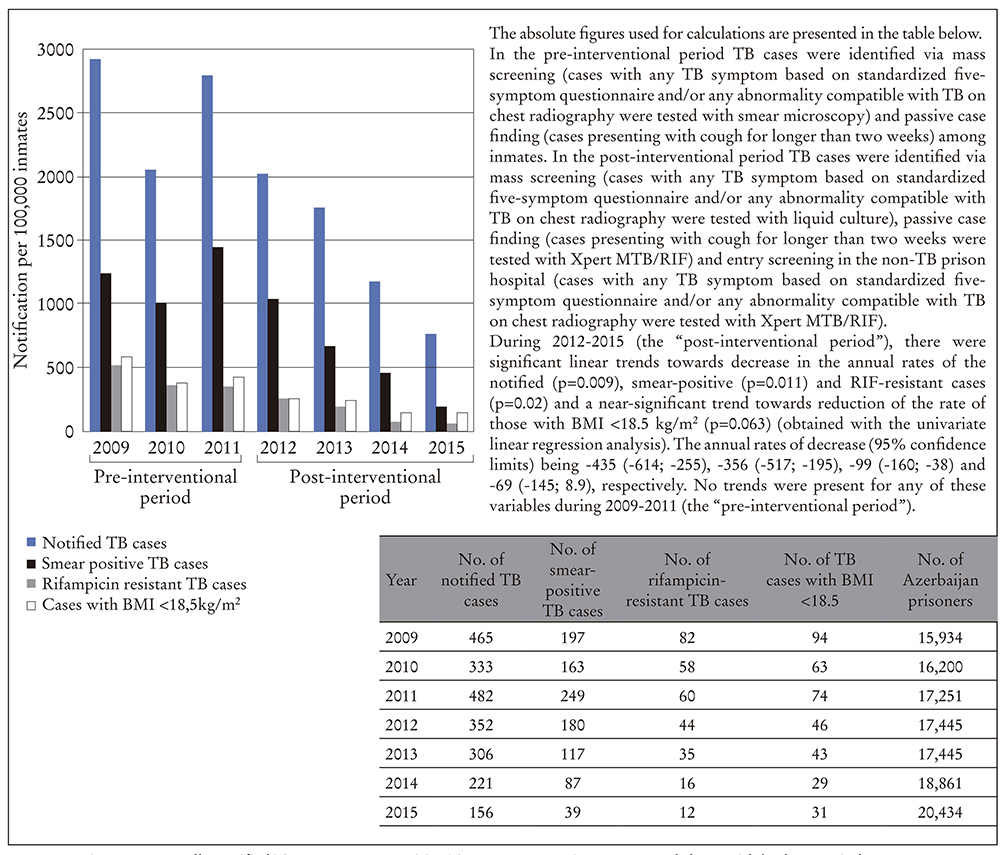
Figure 2 Annually notified TB cases, smear-positive TB cases, RIF-resistant cases and those with body mass index (BMI) below 18.5 kg/m2 at identification in the correctional facilities of Azerbaijan between 01.01.2009 and 31.12.2015, presented as rates per 100,000 prisoners
In contrast to the pre-interventional period, during the post-interventional period, the overall number of smear-positive cases and those with RIF-resistance decreased significantly, while the number of cases with BMI≤18.5 kg/m2 did not change (Table 1). Simultaneously, the number of RIF-resistant cases with additional resistance to fluoroquinolones increased significantly during the post-interventional period (Table 1).
Compared to that, what was evident during the pre-interventional period, the treatment success with FLD during the post-interventional period was significantly higher among all cases, among the cases, which were detected by mass screening and among those cases, which were detected by passive case finding (Table 2). The number of cases identified by passive case finding and successfully treated with SLD were significantly smaller during the post-interventional period than during the pre-interventional period, while no significant difference was identified, when all cases together were compared (Table 2). When the data were analyzed within both study periods, it was found that the cases identified via passive case finding had significantly lower chances for treatment success with FLD, compared to those, identified via mass screening, even after adjustment for smear-positivity, RIF-resistance and BMI≤18.5 kg/m2 (Table 3). The cases detected by the entry screening at the non-TB prison hospital during the post-interventional period had also significantly lower chances for treatment success with FLD than did the cases identified by mass screening (Table 3). Simultaneously, no significant difference for the number of cases identified by various types of case finding and successfully treated with SLD was detected (Table 3).
Table 2 Comparisons between the period, when the rapid tests for detection of TB (Xpert MTB/RIF and liquid culture) were introduced into mass screening and into passive case finding (post-interventional period), and the preceding period (pre-interventional period) for the overall number of cases successfully treated with FLD and SLD, as well as for the cases identified by mass screening or passive case finding and successfully treated with FLD and SLD to show the impact of the inclusion of the rapid tests on the TB burden in the correctional facilities (Azerbaijan, 2009-2014I).
| Pre-interventional period (2009-2011, n=1,280II) |
Post-interventional period 2 (2012-2014, n=834III, IV) |
OR (CI 95%) | P value | aOR (CI 95%) | P value | |
|---|---|---|---|---|---|---|
| Total No. of cases enrolled to the treatment with FLD | 1,159 (90,5) | 735 (88,1) | - - | - - | ||
| No. of cases successfully treated with FLD | 870 (68,0) | 650 (78,0) | 2,38 (1,86-3,05) | <0,001 | 1,93 (1,49-2,50)VII | <0,001 |
| Total No. of cases enrolled to the treatment with SLD | 121 (9,5) | 99 (11,9) | - - | - - | - - | - - |
| No. of cases successfully treated with SLD | 109 (8,5) | 80 (9,6) | 0,46 (0,21-1,00) | 0,053 | ||
| No. of cases identified by mass screeningV and successfully treated | 469 (36,6) | 356 (42,7) | - - | - - | - - | - - |
| No. of cases successfully treated with FLD | 445 (34,8) | 325 (39,0) | - - | - - | 3,60 (2,14-7,06)VII | <0,001 |
| No. of cases successfully treated with SLD | 24 (1,9) | 31 (3,7) | - - | - - | 0,22 (0,04-1,16)VII | 0,07 |
| No. of cases identified by passive case findingVI and successfully treated | 510 (39,8) | 300 (36,0) | - - | - - | ||
| No. of cases successfully treated with FLD | 425 (33,2) | 258 (30,9) | 2,60 (1,81-3,75) | <0,001 | 1,90 (1,32-2,74)VII | <0,001 |
| No. of cases successfully treated with SLD | 85 (6,6) | 42 (5,0) | 0,35 (0,14-0,86) | 0,022 | 0,41 (0,16-1,06)VIII | 0,066 |
Note. BMI: Body mass index; FLD: First-line antiTB drugs; OR: Odds ratio; RIF: Rifampicin; SLD: Second-line antiTB drugs; Successful treatment: Cured + treatment completed; TB: Tuberculosis IOutcomes of SLD treatment of patients detected in 2015 were not yet available at the time of the analyses. IIUsed for calculation of the percentages in the respective column; IIIUsed for calculation of the percentages in the respective column; IVPatients, who were enrolled to treatment with FLD in 2015 and patients, who were enrolled to treatment with SLD in 2014-2015 were still on treatment at the time of the analysis and were excluded from this analysis; VDuring mass screening at the preinterventional period presumptive TB presenting any TB symptom based on standardized five-symptom questionnaire and/or any abnormality compatible with TB on chest radiography were tested with smear microscopy, while in post-interventional period smear microscopy was substituted by liquid culture. VIPassive case finding during the pre-interventional period identified presumptive TB cases based on presence of cough continuing for longer than two weeks, while in post-interventional period presumptive TB cases were identified based on presence of cough continuing for longer than two weeks and following Xpert MTB/RIF testing. Multivariate binary logistic regression analysis was used to assess the difference for the overall number of cases successfully treated with FLD or SLD, as well as to assess the difference for the number of cases detected by mass screening or passive case finding and successfully treated with FLD or SLD. VIIAdjustment was made to the number of smear-positive cases, RIF-resistant cases and those with BMI<18.5 kg/m2. VIIIAdjustment was made to the number of smear-positive cases, those with BMI<18.5 kg/m2, cases resistant to Rifampicin, fluoroquinolones and second line injectables.
Table 3 Comparison between the cases detected in the correctional facilities of Azerbaijan during 2009-2014II by the different types of case finding strategiesI for successfulness of the treatment with FLD and SLD separately for the period, when the rapid tests for detection of TB (Xpert MTB/RIF and liquid culture) were introduced into mass screening and passive case finding (post-interventional period) and for the preceding period (pre-interventional period).
| Pre-interventional period (2009-2011, n=979IV,V) | Post-interventional period (2012-2014, n=730IV,V) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mass screeningVI (n=469) | Passive case findingIV, (n=510) | Mass screening (n=356) | Passive case findingVII, (n=300) | Entry screening at the non-TB prison hospital (n=74) | |||||||
| n (%) | n (%) | aOR (CI 95%) | P value | n (%) | n (%) | aOR (CI 95%) | P value | n (%) | aOR (CI 95%) | P value | |
| Cases successfully treated with FLD | 445 (45,4) | 425 (43,4) | 0,50 (0,38-0,67) | <0,001 | 325 (44,5) | 258 (35,3) | 0,31 (0,17- 0,57) | <0,001 | 67 (9,2) | 0,16 (0,08-0,33) | <0,001 |
| Cases successfully treated with SLD | 24 (2,4) | 85 (16,7) | 0,70 (0,14-3,45) | 0,670 | 31 (4,2) | 42 (5,7) | 0,56 (0,13-2,29) | 0,419 | 7 (1,0) | - | - |
Note. aOR: adjusted odds ratio; BMI: Body mass index; FLD: First-line antiTB drugs; RIF: Rifampicin; SLD: Second-line antiTB drugs; Successful treatment: Cured + treatment completed; TB: Tuberculosis; I During the pre-interventional period, the successfulness of the treatment in patients detected by passive case finding, whereas during the post-interventional period, the successfulness of treatment in patients detected by passive case finding and entry screening at the non-TB prison hospital were compared to the successfulness of the treatment among the patients detected with mass screening; II Outcomes of SLD treatment of patients detected in 2015 were not available at the time of analysis; III During mass screening at the pre-interventional period presumptive TB presenting any TB symptom based on standardized five-symptom questionnaire and/or any abnormality compatible with TB on chest radiography were tested with smear microscopy. IV Passive case finding during the pre-interventional period identified presumptive TB cases based on presence of cough continuing for longer than two weeks; V Successfully treated patients enrolled to the treatment with FLD in 2009-2014 and enrolled to the treatment with SLD in 2009-2013 were analyzed. The rest of the patients were still on treatment at the time of the analysis and were omitted; VI During mass screening at the post-interventional period presumptive TB presenting any TB symptom based on standardized five-symptom questionnaire and/or any abnormality compatible with TB on chest radiography were tested with liquid culture; VII Passive case finding during the post-interventional period identified presumptive TB cases based on presence of cough continuing for longer than two weeks and following Xpert MTB/RIF testing among all inmates, who presented to the prison healthcare units. For the pre-interventional period, multivariate binary logistic regression analysis was used to evaluate the successfulness of treatment with FLD and SLD among patients detected by the passive case finding compared to the successfulness of the treatment with FLD and SLD among patients detected with the mass screening. For the post-interventional period, multivariate multinomial logistic regression analysis was used to evaluate the successfulness of treatment with FLD and SLD among patients detected by the passive case finding and those, who were detected by the entry screening at the non-TB prison hospital compared to the successfulness of the treatment with FLD and SLD among patients detected with the mass screening. In all settings, the independent variables were adjusted for smear positivity, RIF-resistance and BMI<18.5 kg/m2.
Discussion
Our main finding is that introduction of the rapid tests for detection of TB like liquid culture and Xpert MTB/RIF to case finding algorithms in prisons lead to 3-, 10- and 5-fold decrease in the annual rates of all notified, smear-positive and RIF-resistant TB cases, respectively, within a short period. The results of this study are unique, as they provide practical evidence to recommend usage of the rapid tests for case finding in prisons. Formerly, due to the very limited introduction of rapid tests in penitentiaries, such recommendations were mainly based on logical assumptions and mathematical modeling6 7 16 17. Moreover, the finding of many-fold decrease of the TB rates during a short period of time in this study clearly surpassed predictions of the mathematical modeling within similar settings16.
The study showed that the WHO-recommended mass screening and passive case finding work effectively only if coupled with rapid tests. Bearing in mind that each smear-positive case can infect approximately 10-15 persons annually, the role of highly sensitive case finding algorithms in decreasing the TB transmission is inevitable being especially important in settings with the high burden of RIF-resistant TB18 19. Taking into account that the rate of prison population was stable during the study period, the current finding of significant linear trends towards decrease in the TB rates after introduction of the rapid tests assumes also reduction of TB transmission20-22. TB notification in Azerbaijan has been gradually decreasing since 200923. Our finding of no significant trends towards decrease of TB burden in prisons prior the intervention may be considered as an addition argument for efficacy of introduced practice.
Our study also identified improved outcomes of FLD treatment after introduction of Xpert MTB/RIF and liquid culture to the case finding algorithms in prisons. Specifically, the cases detected by mass screening had better outcomes of treatment with FLD than did those, whose disease was identified by passive case finding. Since the clinical symptoms that urge an inmate to seek for a healthcare serve as the trigger for passive case finding, the benefit of mass screening on the outcomes of the treatment with FLD may be explained by the detection of TB at earlier stages, when there are characteristically less or no symptoms or when the patients are smear-negative or have a BMI over 18.5 kg/m2.10 24 25 Along with the evidence from elsewhere that confirms the cost effectiveness of mass screening in prisons26, our finding supports the routine use of mass screening among inmates.
In our study, the overall outcomes of the treatment with SLD did not significantly change throughout the study. However, the worsened outcomes of the treatment with SLD among the cases that were detected by passive case finding during the post-interventional period represented an exception. It has been proven that the number of effective bactericidal anti-TB drugs in the treatment regimen is the main contributor to the outcomes of the treatment with SLD10 27 28. The worsened outcomes of SLD treatment may primarily be related to an enlarged pattern of drug-resistance observed during the post-interventional period and, consequently, to a very limited number of effective bactericidal drugs in the regimen. Practically, this finding appeals to an urgent need to ensure accelerated access to new and repurposed anti-TB drugs in prisons to allow proper treatment of the cases with extensive drug resistance29.
A recent review showed little empirical evidence of benefit from screening without rapid tests to TB notification and treatment outcomes30. The results obtained during the pre-interventional period of the current study obviously support this conclusion. Further data on the routine use of rapid tests for case finding in prisons is especially needed to advocate and accelerate the uptake of new rapid diagnostic technologies in prisons. In the light of the fact that the rapid tests are available in the public health care of the majority of the high-TB-burden countries, the occasional use of these tests in prison system30 challenges the right of inmates for equal healthcare8 31 32.
According to yet unpublished comprehensive biological and behavioral surveillance survey studies performed in Azerbaijan prisons, the HIV prevalence among inmates decreased from 5,8% in 2011 to 2.8% in 2014, which could have also contributed to the improved epidemiological situation of TB.
The limitation of our study is its retrospective nature and little control of potential confusion factors in the logistic regression models apart from disease TB-related characteristics. Nevertheless, our findings suggest sound arguments for informed decision on introduction of rapid diagnostic tests into mass screening and passive case finding algorithms in analogous settings. Since the baseline TB notification rate in the Azerbaijan prisons was similar to the rates reported by correctional facilities of other countries, our findings evokes reproducibility4.
Conclusión
Introduction of rapid diagnostic tests into the algorithms of annual mass screening, routinely performed passive case finding in prisons and entry screening for active TB in the non-TB prison hospitals lead to a significant decline in the overall TB rate, smear-positivity rate and RIF-resistance rate in high TB- and RIF-resistant TB burden prison settings, as well as significantly improved outcomes of treatment with first-line drugs.














