Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.11 no.27 Murcia Jul. 2012
https://dx.doi.org/10.4321/S1695-61412012000300008
DOCENCIA-INVESTIGACIÓN
Sleep habits of the children in the Grau de Gandia. A descriptive study
Hábitos de sueño de la población infantil del Grau de Gandía. Un estudio descriptivo
Martínez Sabater, A.*; Martínez Puig, C.**; Marzà Gascón, A.**; Escrivá Aznar, G.**; Blasco Roque, M.**; LLorca, J.**
*Profesor Colaborador. Facultad de Enfermería. Universidad de Valencia. E-mail: Antonio.Martinez-Sabater@uv.es
**Enfermera. Hospital Francesc de Borja. Gandía. Valencia.
ABSTRACT
Insomnia is the most common sleep disorder in chilhood and it may occur to unweaned babies or during the infant period. In order to be able to detect as early as possible this disease, it is useful to make sleep questionnaires, such as the Spanish Version of the Pediatric Sleep Questionnaire (PSQ).
We considered to know the prevalence of sleep disorders in a population from 3 to 6 years old from the "Graude Gandia", using de Spanish Version of PSQ by means of an autofilled survey answered by the parents of thestudents from the different schools.
We performed a cross sectional study, collecting 144 valid surveys, performing data entry in a EXCEL database for further description.
A 23.4% of the children have insomnia based on the responses and it is significant the presence of other parasomnias such as somniloquy (70%), snoring (7.2%), bruxism (22.3%), rhythmic movement disorders (7.1%) and a 4.1% of the children have symptoms of attention deficit regardless of havingr or not symptoms ofhyperactivity. A 2.08% of the survey responded to a combined ADHD and a 6.25% of the children had symptoms of hyperactivity-impulsivity.
Our study provides similar data to other population studies carried out at schools at this age range and also in higher, with regard to insomnia, parasomnias, sleep habits and ADHD, being the lack of education of the habitof sleep the most common etiology, so the role of the nurse is fundamental in the orientation and training for parents.
Key words: Sleep habit; child population; Health Promotion.
RESUMEN
El insomnio es es trastorno de sueño infantil más frecuente y puede aparecer en la edad lactante o en la etapa preescolar, siendo de utilidad para la detección precoz el uso de cuestionarios de sueño, como la versión española del Pediatric Sleep Questionnaire (PSQ).
Nos planteamos conocer la prevalencia de los trastornos de sueño en una población de 3 a 6 años del Grau de Gandía, utilizando para ello la versión española del PSQ mediante una encuesta autocumplimentada por los padres de los alumnos de los diferentes colegios.
Se ha realizado un estudio descriptivo de corte transversal, recogiéndose 144 encuestas válidas, realizándosela entrada de los datos en una base de datos EXCEL para su posterior descripción.
Un 23,4% de los niños presentan insomnio en función de las respuestas dadas, siendo importante la presencia de otras parasomnias como somniloquias (70%), ronquidos (7.2%), bruxismo (22.3%), trastornos por movimientos rítmicos (7.1%) y un 4.1% de los niños presentan síntomas de satencionales independientemente de que se presente o no síntomas de hiperactividad, un 2.08% de las encuestas respondían a un TDHA combinado y un 6.25% sintomatología de hiperactividad-impulsividad.
Nuestro estudio proporciona datos similares a otros estudios poblacionales realizados en el medio escolar, tanto en este rango de edad como en superiores, respecto al insomnio, parasomnias, hábitos de sueño y los TDHA, siendo la etiología más frecuente la falta de educación del hábito de sueño, por lo que el papel de la enfermera es fundamental en la orientación y formación a los padres.
Palabras clave: hábitos de sueño; población infantil; promoción de la salud.
Introduction
Sleep is a complex physiological condition, necessary and inherent to life. Despite occupying about one third of our lives and it's vital function in the brain, there are still many unknown questions about its nature and function (1).
Knowledge of sleep disorders plus normal and abnormal patterns in children have been the subject of numerous studies over the past 10-15 years and are widely documented in literature, resulting in numerous publications (2).
Defining sleep disorders in childhood is surprisingly difficult for several reasons; there are often sleep problems rather than true sleep disorders, the difference between normal and abnormal is often defined by age and not by sleep patterns since these symptoms can have very different meanings depending on the child's age. In many cases this represents a problem for parents and not for the child (3). Sleep problems could then be defined as unsatisfactory sleep patterns for parents, children or the environment, then there is a close relationship between the problems at night and day time behavioral disturbances. We could then also say that the changes of sleep patterns in children cause family stress and school disorders. On the other hand we define the disorder as a real disturbance and not as avariation of a physiological function that controls sleep and operates over it. Thus, the disorder represents a malfunction while the "problem" may represent it or not (3)(4).
In any case we must take into account that the treatment will be similar whether we refer to it is a disorder or a sleeping problem, because the alteration of specific infant sleep pattern scan cause serious problems, even when there are only normal variations. In addition, sleep disorders, are often associated with various pathologies such as, sleep disturbances in children with gastro esophageal reflux (4), respiratory diseases (such as asthma or obesity) and in the field of neurological processes. We can find children with mental issues or autism and children with neuromuscular problems (5) which can also cause respiratory problems that hinder the sleep process. But we must not forget the relationship between epilepsy and sleep. All these diseases involve the administration of antiepileptic drug treatments, antihistamines, and stimulants, which alter sleep patterns in children. So the dreams of the children can be altered by multiple medical causes and these are the first issues that we must rule out before arriving at a diagnosis of insomnia by incorrect habits.
In the classification of sleep disorders we define two major groups as noted in Table 1 International Classification of Sleep Disorders Revised (taken from American Academic of Sleep Medicine), the first group, dyssomnias, defined as disorders that cause difficulty initiating or maintaining sleep, and which in turn is divided into three subgroups, leading to intrinsic sleep disorders, extrinsic sleep disorders, being the most important in childhood an inadequate sleep hygiene and disorders involving circadian rhythm of sleep, which relate to the timing of sleep over 24 hours. The second group, the parasomnias are the phenomena that occur during sleep characterized by motor and vegetative behaviors, mixed sleep-wake states are more common between three and six years (6) When it comes to sleep disorders is important to differentiate parasomnias (such as sleep walking), night terrors and nightmares, in which etiology are involved maturational and developmental factors (7) of childhood insomnia caused by bad sleep habits. The latter type of insomnia is characterized by difficulty for the child to initiate sleep alone and frequent night time awakenings.
After a literature review, we appreciate that the different diseases and the treatments derived from them can cause different disorders of sleep, but still the bad habit of insomnia is the most common sleep disorder in childhood and may occur in the infant or in the pre-schoolage (8) being the lack of sleeping habits the fundamental etiologic mechanism (6), meaning for the child that the appearance of inappropriate associations derived from the frequent changes made by the parents when they are putting the child to sleep, triggering distortion and disintegration of the habit. Children with this type of insomnia are mentally and physically normal children and the disorder is caused only by a poor acquisition of sleep habits. These children have clear symptoms, children with bright attitudes but no deep sleep are often irritable and restless during the day, they also have great dependence on the caregiver(8) and all this, because throughout the day they haven't slept a suitable number of hours for their age. A fundamental prevention mechanism would be a regular sleeping pattern organized by the parents for their children. It is then easy to understand that sleep is a valuable marker of the health and disease statuses of the child. It is essential to note that sleep disorders may come to affect between 25-45% of children (2), although according to literature, the sleep-related disorders in children are frequent reasons for family consultationin pediatric wards, though in general little attention is paid to prevention, diagnosis and treatment. (10)
An important tool that helps us to detect these disorders are sleep questionnaires, being they very useful both for epidemiological research and for the selection of patients requiring laboratory tests to allow us a more accurate diagnosis of the etiology of these disorders. But we must remember that sleep disorders in general, require a thorough history, a complete physical examination, collaboration of parents in the completion of sleep diaries and if necessary, to carry out the appropriate ancillary tests (9,11)
To understand the evolution of sleep throughout childhood is essential to know, as well as the physiology of sleep, certain specific characteristics of childhood development (11,12). If we keep track of the main characteristics of sleep during the first year of life we would observe that the average length of the sleep cycle in newborn babies is about 30-40 minutes, as brief awakenings are very frequent during the first 2 months of life. During the first 3 months sleep is usually achieved at night with ease, but after this age there is some difficulty in achieving it; this is perhaps related to the desire for relationship with the environment. By the 3rd month the maturation of control systems produces an almost stable distribution of periods of sleep and daytime vigilance so that the diurnal patterns are relatively well established at 12-16 weeks of life. In newborn babies the total sleep duration is usually 16 to 17 hours a day. Total hours of sleep decrease progressively being about 14 to 15 hours by the 16th week and 13 to 14 hours by 6th or 8th month. From the 8th/10th month, the organization and sleep cycles beginto be very similar to those in adults.
It is during the first year of life when the child learns several important habits such as eating and sleeping properly. Thus, parents should know that children should "learn" to sleep alone and should not communicate uncertainty (8). From the age of 2 to about 5 years old we find more gradual changes. Dreams begin to take root in a long night's sleep of about 10 hours. During the second and third years there are short daytime naps and between the third and fifth year it is consolidated in a single night period. Between the ages of 2 to 3 children still sleep with cycles of about 60 minutes, with the first REM period starting around one hour after the start (unlike adults). It is between the ages of 4 and 5 when cycles progressively lengthen to the typical adult 90 minutes.
Children at this age usually have 7 cycles of sleep each night. The transition between different cycles is regular and calm, while adults move sharply during the transitions from one cycle to another (3). It is at this stage of life that you should start changing their sleep habits if they haven't acquired them in the first year of life. Creating a bedtime ritual in addition to combining it with diurnal patterns such as some routine maintenance will help us to change spoiled sleeping habits and help us prevent the occurrence of multiple pathological distortions associated with sleep (8) Finally in the last stage, that includes children from 5 to 10 years, the sleep patterns stabilize and completely resemble that of adults being only 2 hours longer. At this age the presence of constant daytime naps it's a warning about the existence of some pathological process (3). The average length of sleep latency is usually around 15 minutes demonstrating a major state of alert and surveillance.
In summary, throughout childhood there is a progressive decreasing of hours devoted to sleep and sleep is unified in one night episode. Sleep disorders in childhood are frequent and sometimes go unnoticed unless the parents make a query to the pediatrician (10)
Given the importance of the problem of insomnia, we set as our objective to determine the prevalence of sleep disorders in childhood from an assumed healthy group 3 to 6 year olds children from in the neighborhood of Grau de Gandia and what are their usual sleep patterns so that we can develop a guide for parents and teachers regarding the proper sleep hygiene.
Materials and methods
It has been suggested to conduct a cross-sectional descriptive study administering surveys to parents of children enrolled in kindergarten in Grau de Gandia. From the municipal census data, we performed sample size estimation with a confidence interval of 90%, a margin of error of 5% and a level of heterogeneity assumption of 50% resulting in a sample size of 140 surveys. The survey was completed voluntarily by parents, maintaining confidentiality at alltimes and without any contact with children, it has been considered unnecessary to consultthe Ethics Committee.
The Pediatric Sleep Questionnaire (PSQ) is an instrument developed for the detection of sleep problems (12) and it has been validated into Castilian, as discussed previously (9). The basis of our study is the questionnaire, a comprehensive questionnaire with a completion time of approximately 10 minutes and the parents who answered it did so without help from professionals. To this questionnaire we have added demographic data, (information of birthand gender) so that in the first section of the survey they ask development data, age and sex,the second section asks about behavior during night and during sleep, (this consists of 46 questions of which 39 have multiple choice answers of "yes", "no" and "do not know"), a third section on day time behavior and other possible problems, again with 21 close-ended questions with "yes", "no", "do not know" answers. In this paragraph, some questions have been deleted from the original questionnaire (Pediatric Sleep Questionnaire. Reliability Analysis) (9) e. g. "Has had your child, since birth, had a "break" in their growth? If it has describe what happened", "How many cans of soda or cups of coffee does he/she drink per day?", "Does your child take some kind of drug? If so, what and how often?", "Does your childsmoke? How many cigarettes does he smoke per day?" Because given his age (3/6 years) these are not relevant questions in the survey. And a fourth section which consists of 18 close-ended questions about inattention and hyperactivity with five multiples choice responses (for example, "never," "sometimes," "often," "almost always" and "N/C").
Within the questionnaire, there are questions that refer to different parasomnias such as rhythmic movement disorders, bruxism, sleepwalking, bedwetting, somniloquy, nightmares and night terrors. These sleeping habits are measured by four variables: "What time does your child usually go to bed on weekdays?", "What time does he/she goes to bed on weekends or holidays?", "What time does he/she wake up during the week?", "What time does he/she wake up on weekends?". The questionnaire in its last part, as we have outlined before, consists of 18 variables that will determine ADHD (attention deficit and hyperactivity disorder) (2) To define ADHD there are several possibilities, one of them, the one we extract from the questionnaire basing it on similar studies (9), is the existence or not of a combined subtype, at least six of the first nine questions and six of the last nine must be affirmative and answered as "often" or "almost always", the negative responses are answered as "never". Also we'll obtain presence of hyperactive-impulsive symptoms when at least six of the last nine questions are affirmative and inattentional symptoms if at least six of the first nine are affirmative.
We wrote and delivered a letter to the directors of the three schools surveyed, explaining the purpose of the project and thanking them for their collaboration, also 333 questionnaires were provided and a new letter of introduction and explanation of the study were sent to the parents of each student of the three schools surveyed, giving a margin of one week to ten days for completion and subsequent collection. Subsequently the results were transcribed into an EXCEL© database, which has allowed a description and the construction of graphsof the results.
Results
We collected 144 completed surveys of the 333 spread over three schools representing a response rate of 43.24%. The responses were from parents of 70 girls (49%) and 73 boys (51%), since one of the surveys did not include data on age or sex. To summarize the results in a more practical way and to avoid excessive discourse a table has been constructed (Table 2; Table 3, and Table 4 with the percentages of all qualitative and quantitative variables of our questionnaire.
Table 2 Resultados en porcentajes de la encuesta sobre los hábitos de sueño
de los alumnos de infantil del Grau de Gandia en el curso escolar 2010-2011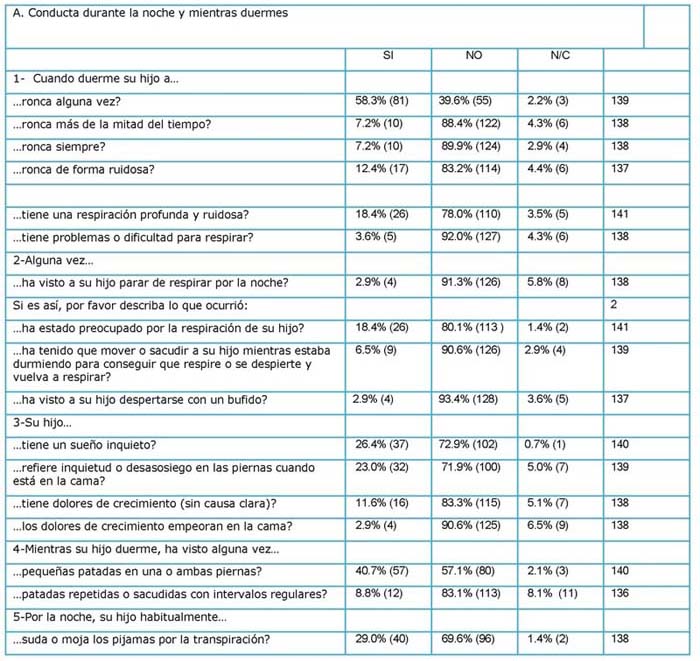

Table 3 Resultados en porcentajes de la encuesta sobre los hábitos de sueño
de los alumnos de infantil del Grau de Gandia en el curso escolar 2010-2011 (y 2)
Table 4 Resultados en porcentajes de la encuesta sobre los hábitos de sueño
de los alumnos de infantil del Grau de Gandia en el curso escolar 2010-2011 (y 3)

However it should be noted, that regarding to sleep habits (Illustration 1 Sleep time in childhood Grau de Gandia.) of the 55 students born in 2005 (6 years old), the average weekday bedtime is 21:30 h (ranging from 20:30 to 23:30) and for weekends is the 22.30h. (Ranging from 20:30 to 23:30 h). The average time that they get up during the week is 8 am (ranging from 7:30 to 8:30 pm) and at weekends, 9 am (ranging from 7:30 to 10:30 am). There is therefore no difference between the average duration of night time on weekdays and weekends or holidays, both of 10 hours and 30 minutes. Of the 50 students born in 2006 (5 years old), the average time that they go to bed on weekdays is 21:30 pm (ranging from 21:00 pm to 23:00 pm) and at weekends is 22:30 pm (with a range of 20:00 pm to 24:00 pm). The average time that they get up during the week is 8:00 am (ranging from 6:30 to 9:00 am) and weekends is 9:00 am (ranging from 6:30 to 10:00 am). There is therefore no difference between the average duration of night time on weekdays and weekends or holidays, both of 10 hours and 30 minutes. Of the 34 children born in 2007 (4 years old) the average time they go to bed on weekdays is 21:30 pm (ranging from 20:00 pm to 23:30 pm) and at weekends is 22.30 pm (ranging from 21:00 to 23:30 pm) the average time they get up during the week is 8:00 am (ranging from 7:00 to 8:00 am) and at weekends is 9:00 am (ranging from 8:00 to 10:00 am). There is therefore no difference between the average duration of night time on weekdays and weekends or holidays, both of 10 hours and 30 minutes.
We note that 23.4% of the children have insomnia (Table 5 Cross of positive responses tothe questions set for the prevalence of insomnia.) and with respect to one of the most significant parasomnias we find that 70% of children show sleep-talking. In relation to the presence of snoring in our students (table 2), it is noted that a 58.3% (81 children) sometimes snore, while only 10 (7.2%) always snore or do it more than half of the time.
Table 5 Cross of positive responses to the questions set for the prevalence of insomnia.
Of the 139 students who answered the question ... "you grind your teeth at night?" There are 105 (75.5%) students do not, compared with 31 students 22.3% who suffer from bruxism. As for the variable that gives us data on respiratory pauses, only 2.9%, i. e. 4 students, have been detected by their parents with breathing pauses at night. 26.4% of the surveys report that children have a restless sleep pattern, showing restlessness in the legs when in bed in 23%. 40.7% are reported to have observed small kicks in both legs, only 8.8% of the cases have them at regular intervals. 39.6% indicated that their child gets up every night for some reason. Regarding to the question "Does your child have nightmares once or more than once a week?" the variable that will determine the prevalence of nightmares, it gets a positive response in 20 students (14.4%) this disorder usually appears between the 4th and 8th years (13), we also observed that it is slightly higher in girls, 12 (17.9%) compared to 8 boys, 11.3%.
Referring to the question "...Does he/she hit his head against something or balance his body when falling a sleep?" That would give us the prevalence of rhythmic movement disorders, it is important to note that 129 students of the respondents (92.1%) do not have this condition as opposed to 10 students, 7.1% who do suffer from it. 15.2% of the parents responded that their children wake up tired in the morning and 25% report that it they find it difficult to wake them up in the morning.
Only 2.2% of the parents indicated that their child has a hyperactivity disorder. However, the latter part of the questionnaire includes 18 variables that will indicate the prevalence of attention deficit disorders and hyperactivity (ADHD), as well as sleep disorders. So we've categorized the positive responses (often, almost always) with a value of "1" and what we think of as negative responses (never, sometimes) with a value of 0. Thus we have obtained, from the 144 surveys that 6 (4.1%) had responded positively to six or more of the first nine variables, which indicates the presence of innatentional symptoms regardless of whether or not they have symptoms of hyperactivity and of these six, 3 (2.08%) coincided with six or more positive answers on the last nine variables, indicating a combined type ADHD (which coincides with the answers given by parents). Nine students (6.25%) had hyperactivity-impulsivity symptoms.
Discussion
Sleep problems are common during childhood and depending on the age and the size of the group that has been investigated we find changes in the prevalence of the different studies. We found no studies that validate the period of school aged children (aged 3-6), that made it difficult to compare, but if we consider other geographical areas and different age groups it allows us to give an approximation of health status on our children.
As for the insomnia, which is defined as "difficulties falling a sleep and / or maintain it, including early awakenings, resulting from this drowsiness or poor daytime functioning." (8) It is one of the variables to consider in this study. Of the 144 students surveyed it has caught our attention that 33 of them meet the requirements to determine the prevalence of insomnia, a significant finding because it confirms that 23.4% of students in the Grau de Gandia suffer from insomnia. By using the PSQ as a questionnaire, like other authors (14) to test for the presence of insomnia in our students, we value the existence of at least two of the four affirmative questions that refer to the inability to sleep, nighttime awakenings, difficulty to go back to sleep after an awakening and early awakenings (Table 5 Cross of positive responses to the questions set for the prevalence of insomnia).
The percentage of insomnia obtained in our study is slightly higher than the study carried out by Pin et al. of children up to 6 years old in Spanish families, which showed that 18.6% of children interrupted the family sleep at least three times a week, and significantly superior to the 2005-2006 school year study in students in primary and secondary education of the cityof Gandia (15) which showed a prevalence for the age group under 12 years of 9.2%. But we must remember that preschoolers and children up to 5 years have a prevalence between 10-30% (6) in disorders of sleep bad habits so that our study, framed in this age group, would be within the normal range.
Regarding the qualitative variable of the sex of the children surveyed, it is important to note that in our case this does not significantly influence the results of the percentages of the different variables. In the reviewed studies on sleep disturbance in school children, we found no gender differences except in the study of sleep disorders in school children in Gandia heldin 2005-2006 (15), citing a higher prevalence of daytime sleepiness and somniloquy in girls, while in boys more frequent bruxism, enuresis and observation by the parents of pauses in breathing during the night. It should be noted that the studies surveyed are variables with statistical significance of age, when studying the whole period of childhood and adolescence. In our case, since we focused our study on a specific period (3-6 years), it has not been possible to compare the results with other studies.
In our study, 22.3% of parents report that their children have symptoms characteristic of bruxism. When compared to a July 2003 (11) national study of children attending schools in urban areas at kindergarten and primary level between the ages of 3 and 8 years it was showed that bruxism is the second most common parasomnia with a prevalence of 26.5%. While in the Gandia study in the group aged under 12 the observed frequency was 14.8% (15). Given that this parasomnia can eventually cause significant wear on teeth and particularly in the molars (16), assuming a level of nursing, which is important to influence oral health education and proper dental hygiene, and that if the contracture is very important, disruption can be avoided with dental prosthesis protection during the night, therefore, we must explain to parents what is the importance of prevention and detection of thisproblem. The information found in the literature indicates that children can often reach 15% prevalence and that it may be based on family medical history (17). However, we note thatbruxism may be a sign of the presence of pinworm parasites in the gut, so we should insiston the education of the parents.
The variable that we will determine the presence of somniloquy, very common phenomenon that occurs during sleep, normally in the morning and that is characterized by expressing verbal sounds with little semantic content that can become intense, with laughter and tears and that the child does not remember the next day (6). It gives a positive result of 98 (70%) students surveyed, prevalence slightly higher than the 62.9% of children under 12 years that had in Gandia in 2005-2006. Although this parasomnia does not imply any specific disease, this disorder is a very typical of starting school age children and may be more evident infeverish conditions (commonly known as "delusions").
During the nightmares the child has dreams that make him/her scared and that wake him/her up frightened, thus making it more difficult to go back to sleep afterwards. In our study, this variable affects 14.4% of the students surveyed. The prevalence in children under 12 in the school year 2005-2006 in Gandía was 13.4%, while in other studies of similar age groups (3 to 8 years) conducted in other countries(11) it was of 25.5 %.
But, with in nightmares we must differentiate from night terrors, a condition that usually occurs during the 2nd and 3rd year and will decrease with increasing age (16). In our study, 47.5% of students have night terrors, compared to 22.2% of those younger than 12 years during 2005-2006 in Gandia. It is the most common parasomnia, with 33.7% of children aged 3 to 8 years of studies outside Spain affected. On the subject of night terrors we encourage parents totake a conservative approach to avoid injury to the child, e. g. falls out of bed, but it is advisable not to wake the child, as the episode will go away with in 4-5 minutes and then the child will go back to sleep without problems.
Parasomnia disorders are easier to interpret and although we have previously mentioned the difficulty of this questionnaire and the different age groups covered, we thought it interesting to compare our results with publications from other countries. (Table 6 Comparison of the frequency of parasomnias with other studies from the study of Thomas et al.)
Table 6 Comparison of the frequency of parasomnias with other studies from the study of Thomas et al.
According to the classification of sleep disorders (18) we differentiate three sleeping disorders as dyssomnia, which in our case we detailed as questionnaire variables. In the case of obstructive sleep disorders, we know that approximately 10-12% of children snore, and many of them have what we call "simple snoring" it is the snoring not associated with apnea (19) In this case only 7.2% always refers snoring or more than half the time. From the nursing point of view, as a preventive measure of the risk of OSAS in children is knowing that the prevalence of childhood obesity is increasing in Spain and that approximately one third of overweight children have sleeping disorders related to breathing and that obesity in children with OSA ranges between 13 and 36% (20). We note that although the respondents to the question... "Is your child overweight?" 126 of the children surveyed (92%) answered negatively, education in healthy eating habits in children will help prevent this condition on infant sleep.
Regarding habits, most publications refer to the hours of sleep in early childhood and adolescence, so the analysis and comparison of results becomes even more complex. A previous population study (21) shows that sleep duration among children of up to 6 years old is approximately 10.9 hours, while another (22) gives figures of 9.5 to 13.3 hours in children up to 5 years old. Our data shows that in the period between the ages of 3 to 6 children sleep 10.30 hours, this data is very similar to other publications, showing no differences between sleep during the week and weekends. However in order to maintain the number of hours of sleep on weekends they have to delay the time they get up.
In most publications we see an important relation ship between sleep impairment and drowsiness with school performance, cognitive functioning and emotional disorders (15), hence the importance of promoting proper sleep habits from an early age and prevent future sleep disorders.
In the final part of our questionnaire we analyzed ADHD, which is the most common neuro developmental disorder in childhood and the most prevalent in children of school age, between 3-5% (23) In other population studies conducted in schools the overall data rate of ADHD had a prevalence ranging between 5.5 and 8.5% (2) Consistent with the percentages obtained in our study that would fall between 2.08 and 6.25%. There is great variety of literature and different criteria for diagnosing ADHD, however we believe it to be of interest to obtain this data because the children who have ADHD in childhood may continue to have symptoms during adolescence and adulthood, therefore early diagnosis and treatment could modify their educational and social development, along with improving the quality of life of the child and his/her family.
Conclusions
Note that in our study, the results are similar to other population studies in schools, both in the parasomnias and sleep patterns and ADHD.
We are reminded that the results of the prevalence of insomnia, (23.4%), is the most common cause is a lack of education of sleeping habits in children, and that guiding the parents to acquire proper guidelines for their children sleep helps prevent future sleep disorders.
The most common parasomnias are sleep-talking, night terrors, bruxism and nightmares.
Although our results show that our students are in the correct percentages for their age groups when compared to different studies of teenagers, they present a gradual decrease of the nocturnal hours of sleep and a slight increase in day time sleepiness (15), data of concern because it is clearly associated with school performance, cognitive functioning, emotional disorders ... that indicates the need to promote healthy lifestyles.
The existence of ADHD that is directly related to an increase in sleep disorders is highlighted along with its detection and prevention leading to positively influence the quality of life of the children and their families.
And we must not forget that while this study provides data only on the population prevalence and age group studied, with the difficulty of carrying out comparative studies, it is a step towards the greater understanding of sleep disorders in terms of epidemiological investigation
With all this the figure of the school nurse is considered essential. The nurse has an important role, both in terms of the promotion and education of healthy habits plus the detection of problems with parents, teachers along with direct contact with the health center of reference. This forms a suitable combination that allows us to detect and prevent future sleep problems in our schools.
For future research we will consider a number of improvements, such as sample size increases (to a greater age range) and the use of statistical techniques to provide greater reliability.
References
1. Pin Arboledas G. Bases fisiológicas y anatómicas del sueño. Pediatria Integral. 2010; 14(9). [ Links ]
2. Tomas Vila M, Miralles Torres B, Beseler Soto M, Revert Gomar M, Sala Langa M. Relación entre el trastorno por déficit de atención e hiperactividad y los trastornos del sueño. Resultados de un estudio epidemiológico en la población escolar de la Ciudad de Gandía. Anales de Pediatria. 2008;(69 (3)): p. 251-7. [ Links ]
3. Escalera Gamiz A. Trastornos del sueño infantil. Innovación y experiencias educativas. 2009 febrero 15; 15. [ Links ]
4. Didden R, Korzilius H, Van Apperlo B, Van Overloop C, de Vries M. Sleep Problems and daytime problem behaviours in children with intellectual disability. 2002;(46): p. 537-47. [ Links ]
5. Gharem M, Amstrong K, Trocki O, Ceghorn G, Patrick M, Sheperd R. The Sleep patterns of infants and young children with gastro esophagcal reflux. J. Pediatr. Child Healh.1998;(34): p. 160-3. [ Links ]
6. Richdale A, Prior M. The sleep-Wake rhythm in children with autism. Eur Child Adoles Psychiatry. 2000; 3(4): p. 175-86. [ Links ]
7. Estivill E. Trastornos del sueño en la infancia. In Psicología conductual.; 1994. p. 347-362. [ Links ]
8. Peralta R. Semiología, evaluación y diagnóstico de los trastornos de la vigilancia y del sueño en la infancia. Revista neurológica. 1997;(25): p. 1429-33. [ Links ]
9. Estivill E, Segarra F. Insomnio infantil por hábitos incorrectos. Rev Esp Neurol. 2000;(30): p. 188-191. [ Links ]
10. Villó Sirerol N, Kheiri Amin I, Mora Rodríguez T, Saucedo Frutos C, Prieto Yebra M. Hábitos del sueño en niños. An Esp Pediatr. 2002; (2)(57): p. 127-30. [ Links ]
11. Tomás Vila M, et al. Versión española del sleep questionnaire. Análisis de fiabilidad. 2007; 2(66): p. 121-8. [ Links ]
12. Minde K, Popiel K, Leos N. The Evaluation and treatment of sleep distubances in young children. 1993;(34): p. 21-533. [ Links ]
13. Aldana A, Samundio D, Irala E, Rodas N. Trastornos del sueño: prevalencia en población pediátrica en edad preescolar y escolar de área urbana. Pediatr. (Asuncion). 2006; 33(1). [ Links ]
14. Mindell J, Owens J. A clinicinal guide to pediatric sleep diagnosis and management of sleep problems. 2003. [ Links ]
15. Chervin R, Hedger K, Dilon J, Pituch K. Pediatric Sleep Questionnaire (PSQ): Validity and reliability of scales-disordered brrea thing, snoring, sleepiness and behavioral problems. Sleep Medicine. 2000;(1): p. 21-32. [ Links ]
16. López SA. Trastornos del sueño en la infancia. In Trastornos del sueño en el niño: identificación y herramientas para su manejo. [ Links ]
17. Archold K, Pitach K, Panabi P, Chervin R. Symptoms of sleep distrurbances among children at two general pediatric clinics. J pediatr. 2002;(140): p. 97-102. [ Links ]
18. Vila M, Torres A, Miralles A, B S, Beseler B, Gomar M, et al. Patrones normales y trastornos del sueño entre la población escolar de la ciudad de Gandía. An Pediatr. 2008;3(68): p. 250-6. [ Links ]
19. Puñal J, Gay L, Castro-Cago M. Principales trastornos del sueño. In Libro de Ponencias Madrid; 2010; Madrid. p. 55-59. [ Links ]
20. Castro-Cago M, Novo-Rodríguez M, Eiris-Puñal J. Trastornos paroxísticos y síntomas episódicos no epilépticos en relación con el sueño. Anales Esp. Pediatría. 2001;(54(Supl. 4)): p. 193-202. [ Links ]
21. American Academic of Sleep of Medicine. Classification of sleep disordars, revised: Diagnotic and coding manual. In. Chicago, Illinois: American Academy of Sleep Medecine. International; 2001. [ Links ]
22. Pin G. Trastornos respiratorios obstructivos del sueño en el niño. In PCF S, editor. Propuesta de Ponencia oficial Congreso Nacional. [ Links ]
23. Llorente E, Meltrana J, Vicente E. Obesidad y trastornos respiratorios obstructivos del sueño en el niño. In Propuesta de Ponencia Oficial Congreso Nacional del 2013:PCF, SEORL. [ Links ]
24. I I, Jenni O, Molinari L, Largo R. Sleep duration from infancy to adolescence: reference values and generation trends. Pediatrics. 2003;(115): p. 1774-86. [ Links ]
25. Jenni O, Molina L, Caflisch J, Largo R. La duración del sueño de las edades de 1 a 10 años: la variabilidad y la estabilidad en comparación con el crecimiento. Pediatría. 2007 noviembre; 120(4): p. 769-76. [ Links ]
26. Valdizan JR. Trastornos generalizados del desarrollo y sueño. Rev. neurológica. 2005;41(supl. 1): p. 135-138. [ Links ]











 texto em
texto em 




