My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.14 n.37 Murcia Jan. 2015
DOCENCIA-INVESTIGACIÓN
Experiences of human milk donation in Andalucía-Spain: a qualitative study
Experiencias de donación de leche humana en Andalucía-España: un estudio cualitativo
Machado, Raylane da Silva*; Campos Calderón, Concepción P.**; Montoya Juárez, Rafael*** and Schmidt RioValle, Jacqueline****
*Nursing student exchange at the University of Granada-Spain. Intern Program Ciencias sin fronteras of CNPq. University Federal do Piauí. Brazil. E-mail: raylane.s.machado@gmail.com
**Faculty of Health Sciences University of Granada. Spain
ABSTRACT
Introduction: The benefits of feeding human milk to infants have been well-documented. Collecting excess human milk from lactating mothers is an important social service. The Human Milk Banks depend on donors, and knowing the subjective aspects of donors seems quite important.
Objective: Compiling the experiences, beliefs, motivations and difficulties concerning milk donation in a group of donors belonging to the Human Milk Bank of Granada- Andalucia.
Methods: A descriptive qualitative study was conducted from May to June of 2013. The sample consisted of 7 women who donated milk to the Human Milk Bank located in the Virgen de las Nieves hospital of Granada. Data was collected using a semi-structured interview.
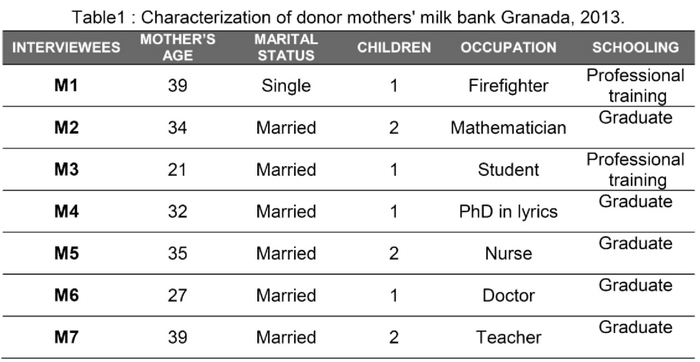
Results: Most of the interviewees were over thirty years old, had completed or were in the process of completing university, married, and had one or two children. During the interview, the following subjects were discussed with the mothers: Decision of becoming a donor, support to the donor, motivation for donating, and difficulties donating.
Conclusion: The results of our study suggest that many mothers are still not aware that there are milk banks present in their location. Expanding the number of milk banks in Spain is essential for hundreds of premature babies who are in need of this necessary resource.
Key words: Human Milk Banks; Human Milk; Breastfeeding; Donation.
RESUMEN
Introducción: Los beneficios de la lactancia materna para los bebés han sido bien documentados. Recoger el exceso de leche humana de madres lactantes es un servicio social importante. Los bancos dependen de las donaciones de madres lactantes, por ello la importancia de conocer los aspectos subjetivos que interfieren en la donación.
Objetivo: Conocer las vivencias, creencias, motivaciones y dificultades respecto la donación de leche de un grupo de mujeres donantes en el Banco de Leche Humano de Granada-Andalucia.
Métodos: Estudio descriptivo, con abordaje cualitativo, realizado en el período de mayo y junio de 2013. La muestra estuvo constituida por 7 mujeres que donaron leche en el banco de leche humana del Hospital Virgen de las Nieves de Granada. Para la recogida de datos se utilizaron entrevistas semi-estructuradas.
Resultados: Las informantes tenían en su mayoría más de treinta años, con nivel universitario, casadas y con uno o dos hijos como máximo. De los discursos de las madres emergieron las siguientes categorías: Decisión de hacerse donante; Motivaciones donación; Apoyo donación y Dificultades donación.
Conclusión: Como se evidencia, el banco de leche es todavía poco conocido. Todavía existen pocos bancos de leche en España, intentar ampliar esa red sería fundamental para cientos de prematuros que necesitan de esa leche.
Palabras clave: Banco de Leche Materna; Leche Humana; Lactancia Materna; Donación.
Introduction
It is proven that breast milk is the ideal food for newborns1. It is the food of choice for the first 6 months of life for all children and should extend at least through the first year and beyond that age if both mother and child desire1-3.
In situations in which breastfeeding is contraindicated or difficult (preterm or low birth weight or cases where pathology of the mother or the infant prevents her to breastfeed him directly), the World Health Organization1, the Unicef 2 and the Spanish Association of Pediatría4 (AEP) set donated human milk as resource of first choice for maintenance of milk intake. In this context, Human Milk Banks (HMB) play a key role in ensuring the food supply.
A HMB is a medical device dedicated to collect milk from donors, process, store, and deliver, following all health requirements, for newborns who may need it. Therefore, it is responsible for the donor selection, storage, processing, analysis and milk distribution 2,5
The donors are healthy women in the first semester of their lactation period with milk production higher than her child needs, and who are willing to donate it for free will 6. To be a donor, the mother should undergo a detailed clinical examination, in order to protect her and the recipient's health. Exclusion criteria are smoking, drinking or exciting substances in large quantities, practice risk of communicable diseases, chronic diseases or current use of any medications 7.
The first world's milk bank was established in Vienna in 1909. Since then, milk banks were being implemented in many countries. There are well-established national associations in the United States of America, United Kingdom, Italy and Brazil 5,7,8 The Brazil is the world leader of national network of BLH 8,9,10 and has the largest (213 banks in 2013)10 and more complex network, implemented as a strategy of the Ministry of Health to improve the health of mothers and infants 5,7,11.
In 2008 was created the Spanish Association of Milk Banks. One of its main objectives is promote the creation of milk banks in Spain and facilitate cooperation between national milk banks and European milk banks 5,7 Since the opening of the first BLH in 2001, Spain now has seven milk banks, which aim to feed hundreds of infants12 Virgen de las Nieves Hospital's milk bank in Granada was installed based on the Brazilian model. It started its functioning in May of 2010 and it is the only operating HMB in Andalucía.
This study aims to understand the experiences, beliefs, motivations and difficulties regarding milk donation of a group of women who donate milk in Granada. Knowing these meanings can redirect the practices carried out by the professionals involved with the binomial mother-baby, so there would be more awareness of mothers and the consequent expansion of the number of donors.
Methods
This is a descriptive study, conducted according to the principles of qualitative research, which is characterized by providing the researcher the ability to capture the way in which individuals think and react, allowing understanding of the dynamics and structure of the situation under the terms of who lives it 13 In this regard, the focus of this study was phenomenological and the phenomenon being studied is the milk donation to HMB.
The project was approved by the Ethics Committee for Biomedical Research of the Province of Granada. The population consisted of 7 women who donated milk during May and June 2013 in the Virgen de las Nieves Hospital's HMB in Granada. After they accept and sign the informed consent, semi-structured interviews were conducted in a single meeting with each informant. The interview content consist of the following questions: Why did you decide to become a milk donor?, What did your family and friends think of this decision? Have healthcare workers (nurses and doctors) influenced in your decision to donate?, Did you have any difficulty to donate?.
A structured model adapted from Flick was used for the analysis and interpretation of data14: 1) transcript of the interviews, 2) discovery of codes and development of families or categories of analysis; 3) coding the interviews based on the categories identified; 4) data interpretation in the context in which they were collected.
Atlas-ti 6.2 computer program was used as a tool; designed to facilitate qualitative analysis to provide reliability, accuracy and quality of the results 13.
Results
Table I presents the sociodemographic characteristics of the 7 women who participated in the study.
According to the categories analyzed, we have found the following results:
Decision to become a donor
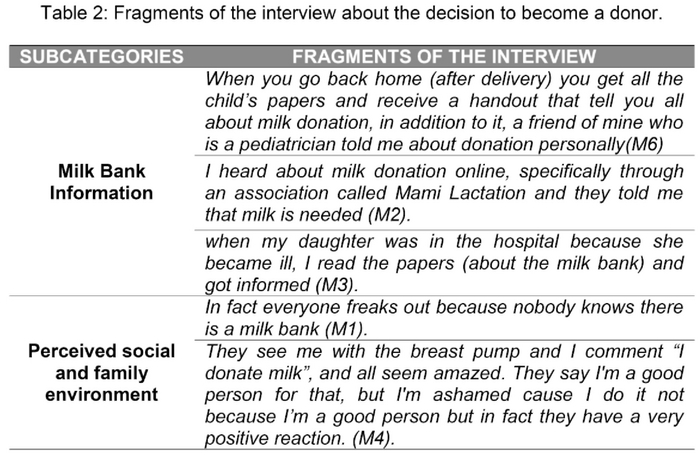
In terms of the factors that influenced the decision to become a human milk donor emerged two subcategories: Milk Bank Information and Perceived social and family environment (Table 2).
- Milk Bank Information: how women get to know the milk bank or knew of the possibility of human milk donation. They are aware of the milk bank, at first, through handouts delivered to them after discharge postpartum. Subsequently, they develop curiosity about the subject and do a personal quest for information on how they can become donors.
- Perceived social and family environment: refers to the opinion that family and friends have over the decision of being a human milk donor. Donors report that their immediate environment (family and friends) tend to have a very positive reaction after knowing that they contribute with their milk, since many of them do not know about the existence of the milk bank and its purpose.
Motivations to Donate
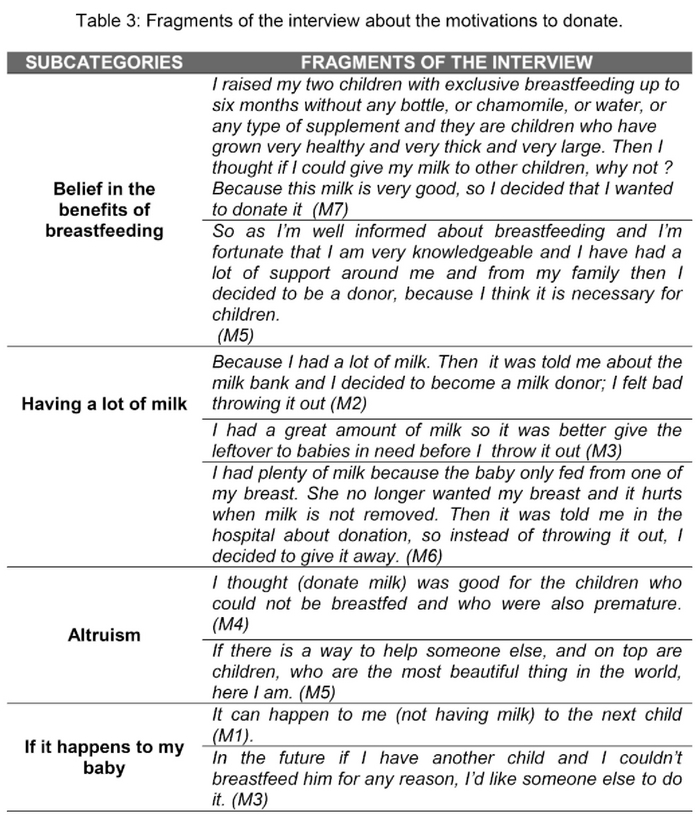
After analyzing the speeches of mothers about the motivations that led them to become milk donors, four sub-categories emerged (Table 3).
- Belief in the benefits of breastfeeding: female participants attribute a number of positive meanings to breastfeeding. The mothers believe that breast milk is the best food that one can give to children, based on their own experience as mothers.
- "Having a lot of milk": mothers expressed that one of the main motivations for donating milk was overproduction, which caused them engorgement, with consequent pain and discomfort. The donation is then converted into an opportunity to relieve the symptoms of engorgements.
- Altruism: another motivation of donors was act selflessly for the benefit of another, in this case, benefit of babies in difficult conditions, as most children are premature receptors.
- "If it happens to my baby': In addition to altruism, some mothers said they decided to donate because they think that one of their future children may need it and would be great if someone could donate milk for their children too.
Support to donation
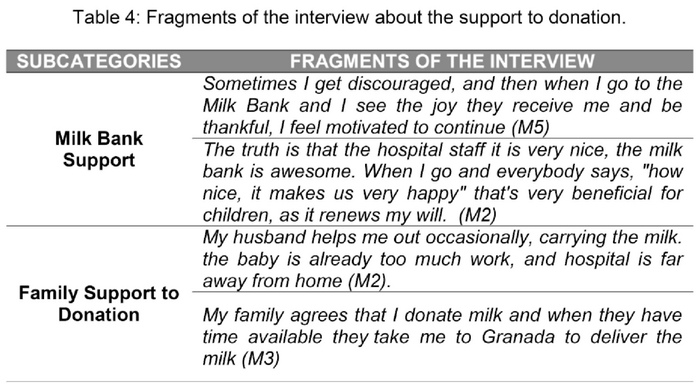
The environment of the mothers has a positive influence on the willingness of participants to continue with the donation (Table 4). In this regard, we have found the following support elements:
- Milk Bank Support: support given to mothers by the milk bank staff to remain donors. The donors report that they feel reinforced by health professionals. They also attribute great importance to the constant effort they made to keep them motivated.
- Family Support to donation: donors also receive support from their family, especially their partners. In most cases, it was embodied by transferring them to the milk bank, or delivering the milk themselves
Difficulties to donate
This category describes the obstacles that mothers noticed to start and remain a milk donor. Participants identified four main barriers (Table 5):
- Lack of knowledge of other health professionals: lack of information about the existence of milk banks by health professionals who care for women in other units (hospital, health center), resulted in twice the trouble for many women, first to locate the milk bank and then to become a donor.
- Distance from the milk bank: one of the complicating factor for milk donation is the distance, in most cases, one have to travel from their homes in the interior of the province to deliver the milk to the center.
- Incomprehension at Work: many mothers report that they receive no support in their workplace, on the contrary, even receive insinuations about stop breastfeeding or at least introduce a complementary food supply earlier, so they could perform better at work without having to leave to breastfeed.
- Reduction of milk by the process of breastfeeding itself: women also highlight the fact that, eventually, they no longer produce as much milk as the moment when they decided to become donors, so they begin to decrease the frequency in donations. Although this is a natural process, in this case, women face it as a challenge to remain donors.
Discussion
The results of this study present an approach to the subject of human milk donation in Andalucía, providing the perspective of donors and the dynamics with which this practice is developed in Spain.
The informants were mostly over thirty years, with university education, married and with a child or two at most, these data are similar to those handled by 12 de Octubre Hospital (the largest milk bank in Spain) which indicate that donors usually have about 30 years, donate with their first child, have a stable partner and about half of them went to college6.
Despite the importance of human milk collected in BLH for the survival of newborns, disclosure on the subject is still very limited. The information is provided mainly in the process of hospitalization for childbirth in maternity, not covering prenatal care network or health centers (Table 2). The same factor can be observed in other studies14,15 pointing misinformation as one of the major problems for mothers decide not to donate milk.
It can be hypothesized that many potential donors have frustrated their intentions, not getting to implement their role as donors. Our data indicate that although they are aware of the existence of BLH through associations to support breastfeeding or online, personal desire is the main factor to be a donor.
It is pertinent to suggest that milk collection routines are reconsidered, with the establishment of milk collection in the donor's own home, as a solution to one of the major difficulties pointed out by the donors: the distance they have to travel to bring the donated milk. This system is now operational in Brasil16 and achieved great success by expanding the number of donors and the frequency of donation.
Currently, there is only one milk bank in Andalucía, which is localized in Granada. The participants themselves request the implementation of more HMB units. This would facilitate a rapprochement with the donor population and increase coverage to children who need donated milk.
An important aspect of our results concerns the recognition of donors in relation to the benefits and nutritional quality of breast milk. Altruism emerges as the main motivation for our participants, and acknowledge that the decision to donate, relates exclusively to women. The second most cited reason is excess milk production, when they realize that they can make a good use of the extra milk and avoid loss.
Another issue pointed out by the donors, and that makes them appear more sensitive to donating milk is put themselves in the place of mothers who experience difficulties breastfeeding their children, and even the thinking that this might occur to them in the future.
In other studies in Brazil14,15,16 and Guatemala8 the following reasons and feelings involved in donating milk are highlighted: solidarity, love, comfort, value of milk, personal satisfaction, retribution and altruism. In studies of Francia17 and USA18mothers who had breast engorgement were led to donate their milk guided by health professionals.
Conclusion
As evidenced, the milk bank is still poorly known, mainly due to the lack of disclosure. Expand the network of milk banks in Spain would be essential for hundreds of premature babies that need milk and cannot access them due to the distance from their homes.
The need for greater promotion and guidance is shown on donation of human milk, with particular emphasis on the reasons given by the women in this study (altruism, benefits of breastfeeding, "Having a lot of milk," to take the place of other mothers), and also promote the support from relatives and health care professionals.
The conclusions that can be drawn from this study are limited by the use of convenience sample of donors, it is not known how representative their views and experiences are of the total population of donor milk.
To encourage the recruitment of new human milk donor, should be conducted educational / informative activities in prenatal care services, maternity, childcare and strengthen the system of communication with other health sectors.
Therefore an investment in research and scientific production should be increased in order to improve and ensure the life quality of children whose mothers cannot breastfeed.
Received: February 9, 2014
Accepted: April 4, 2014
References
1. World Health Organization. Infant and young child nutrition: global strategy on infant and young child feeding. Geneva: World Health Organization; 2002. [ Links ]
2. García-Lara N R, García-Algar O, Pállas-Alonso C R. Sobre bancos de leche humana y lactancia materna. An Pediatr (Barc). 2012;76(5):247-249. Disponible en: URL: http://zl.elsevier.es/es/revista/anales-pediatria-37/sobre-bancos-leche-humana-lactancia-materna-90132447-editorial-2012?bd=1. [ Links ]
3. WHO/UNICEF. Protecting, promoting and supporting breastfeeding: the special role of maternity services. Geneva: World Health Organization; 1990. [ Links ]
4. Hernández-Aguilar MT, Aguayo-Maldonado J. La lactancia materna. Cómo promover y apoyar la lactancia materna en la práctica pediátrica. Recomendaciones del Comité de Lactancia de la Asociación Española de Pediatría. An. Pediatr (Barc). 2005;63(4):340-56. Disponible en: URL: http://zl.elsevier.es/es/revista/anales-pediatria-37/articulo/la-lactancia-materna-como-promover-13079817. [ Links ]
5. Gormaz M, Roqués V, Dalmau J, Vento M, Torres E, Vitoria I. Actividad de un banco de leche humana implantado en una unidad neonatal. Acta Pediatr Esp 2011; 69 (6): 283-287. [ Links ]
6. Sierra Colomina G, et al. Características de las mujeres donantes de un banco de leche materna y relación con el tiempo de donación. An Pediatr (Barc). 2013. Disponible en: URL: http://dx.doi.org/10.1016/j.anpedi.2013.05.017. [ Links ]
7. Vázquez-Román S, Alonso-Díaz C, Medina-López C, Bustos-Lozano S, Martínez-Hidalgo MV, Pallás-Alonso CR. Puesta en marcha del banco de leche materna donada en una unidad neonatal. An Pediatr (Barc) 2009; 71 (4): 343-348. [ Links ]
8. De León Soto J F, Arreaga Fion G L. Conocimientos, actitudes y percepciones de madres Lactantes respecto a la donación de leche materna al Banco de leche humana del Hospital Nacional Pedro de Bethancourt (tesis doctoral). Guatemala: Universidad de San Carlos de Guatemala; 2008. [ Links ]
9. Da Silva SL. Alegações maternas para doação de leite (tesis doctoral). Recife: Universidade Federal de Pernambuco; 2010. [ Links ]
10. Brasil. Ministerio da Saúde. A Rede Brasileira de Bancos de Leite Humano: Bancos de Leite Humano - Localização e Relatórios. Disponible en: http://producao.redeblh.icict.fiocruz.br/portalblh/blh_brasil.php. [ Links ]
11. Da Silva Machado R, Soares LS, Da Silva Freitas GR. Red brasileña de bancos de leche humana: revisión de los aspectos históricos y políticos. Nutr. Hosp. (revista en la Internet) 2012;(Supl. 3)27:1-87 (citado 2013 Sep 06). [ Links ]
12. Asociación Española de Bancos de leche Humana. Tu banco de leche. Disponible en: http://www.aeblh.org/tu-banco/. [ Links ]
13. Flick, U. Introdução pesquisa qualitativa. 3aed. Porto Alegre: Artmed; 2009. [ Links ]
14. Galvão M T G, Vasconcelos SG, Paiva SS. Reasons Women donate breast milk. Acta paul. enferm. (serial on the Internet). 2006 June (cited 2013 Sep 06); 19(2): 157-161. Available from: http://www.scielo.br/scielo.phb?script=sci arttext&pid=S0103-21002006000200006&lng=en.http://dx.doi.org/10.1590/S0103-21002006000200006. [ Links ]
15. Dias RC, Baptista IC, Gazola S, Rona MSS, Matioli G. Human milk bank donors' profile at Hospital Universitário de Maringá, State of Paraná, Brazil. Acta Sci Health Sci. 2006;28(2):153-8. [ Links ]
16. Tomaz ACP, Loureiro LVM, Oliveira TS, Montenegro NCMF, Junior EDA, Soriano CFR, Cavalcante JC. The human milk donation experience: motives, influencing factors and regular donation. Journal of Human Lactation. 2008; 24(1):69-76. [ Links ]
17. Azema E, Callahan S. Breast Milk in France: A Portrait of tropical donor and the utility of milk banking in the French breastfeeding context. Journal of Human lactation. 2003; 19(2): 199-202. [ Links ]
18. Osbaldiston R, Mingle LA. Characterization of Human Milk Donors. Journal of human lactation. 2007; 23(4):350-7. [ Links ]











 text in
text in