Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.14 no.38 Murcia abr. 2015
CLÍNICA
Urinary catheterization delay: clinical practice
Cateterismo urinario permanente: práctica clínica
Cateterismo urinário de demora: prática clínica
Mazzo, Alessandra*; Bardivia, Carolina Beltreschi**; Jorge, Beatriz Maria***; Souza Júnior, Valtuir Duarte***; Fumincelli, Laís***; Mendes, Isabel Amélia Costa****
*RN, Ph.D.
**Nursing undergraduate
***RN. Nursing graduate Program in Fundamental Nursing
****RN, Full Professor. E-mail: iamendes@usp.br
University of São Paulo at Ribeirão Preto College of Nursing (EERP-USP). Brazil
ABSTRACT
Objective: Verify how the urinary catheterization delay procedure has taken place in clinical nursing practice.
Method: Observational, exploratory and descriptive study, undertaken at hospitals in an interior city in the State of São Paulo, Brazil. The ethical premises were complied with (Opinion 233/2008 University of São Paulo at Ribeirão Preto College of Nursing Research Ethics Committee). The data were collected through an interview, using a semi structured script. Nine out of 13 institutions in the city participated in the study.
Results: At the participating institutions, the procedure is performed ritualistically in terms of method and materials.
Conclusion: To practice urinary catheterization delay, greater professional commitment and further investments in research are needed to clarify aspects that cannot be proven yet.
Key words: Urinary Catheterization; Teaching; Nursing; Techniques.
RESUMEN
Objetivo: Verificar cómo el procedimiento de inserción del catéter urinario permanente ha ocurrido en la práctica clínica de enfermería.
Método: Estudio observacional, exploratorio y descriptivo, desarrollado en hospitales de un municipio del interior del estado de São Paulo, Brasil. Las premisas éticas fueron cumplidas (Parecer 233/2008/Comité de Ética en Investigación de la Escuela de Enfermería de la Universidad de São Paulo). Los datos fueron recolectados mediante entrevista, utilizándose un instrumento semiestructurado. De las trece instituciones del municipio, nueve participaron del estudio.
Resultados: En las instituciones investigadas, el procedimiento es practicado de manera ritualista respecto al método y los materiales.
Conclusión: Para practicar el cateterismo urinario permanente es necesario mayor compromiso de los profesionales y mayores inversiones en investigaciones para esclarecer los aspectos que todavía no pueden ser comprobados.
Palabras clave: Cateterismo Urinario; Enseñanza, Enfermería; Técnicas.
RESUMO
Objetivo: Verificar como o procedimento de inserção do cateter urinário de demora tem se dado na prática clínica da enfermagem.
Método: Estudo observacional, exploratório e descritivo, realizado em hospitais de um município do interior paulista. Seguidos os preceitos éticos (Parecer 233/2008/ Comitê de Ética em Pesquisa da Escola de Enfermagem de Ribeirão Preto da Universidade de São Paulo), os dados foram coletados por entrevista, utilizando-se um instrumento semi-estruturado. Dentre as treze instituições do município, nove participaram do estudo.
Resultados: Nas instituições pesquisadas o procedimento é realizado de forma ritualista quanto ao método e materiais.
Conclusão: para realização do cateterismo urinário de demora é necessário maior comprometimento dos profissionais e maiores investimentos em pesquisas para esclarecimento dos pontos que ainda não podem ser comprovados.
Palavras chave: Cateterismo Urinário; Ensino; Enfermagem; Técnicas.
Introduction
Urinary catheterization is used in patients who experience difficulties or are unable to urinate. It consists in the introduction of a probe into the bladder to remove the urine(1,2).
The introduction of instruments in the urethra to remove the urine goes back a long time. Initial records of this practice are found among the Egyptians; at that time, hollow tubes made of copper and lacquer were used. Later, the Greeks, Romans and Chinese used similar equipment. It was only in the Xth century, however, that records of the first flexible urethral probes appear, made out of animal leather. Advances in the confection of urinary catheters can only be observed in the XIXth century, as a result of the rubber treatment and the French urology's innovative techniques (2).
The insertion process of the urinary catheter should be sterile or clean, according to its dwelling time. Risks of trauma and Urinary Tract Infection (UTI) always exist.
In intermittent urinary catheterization, the catheters are removed soon after emptying the bladder, which implies lower UTI rates. In urinary catheterization delay, the risks of UTI are more significant. The UTI the use of urinary catheters delay provokes is closely related to the dwelling time and the increasing number of patients using a catheter. It entails economic repercussions, sequela, complications and immeasurable damage to the population (2,3).
The traumas the catheter insertion causes often are not diagnosed, resulting in injuries and false ways, which may or may not come with urethral bleeding and urinary tract infection; they provoke painful manifestations due to the friction of the badly lubricated catheter against the urethral mucosa and/or the aggressive maneuvers deriving from the strength applied to insert it. Traumas are common in male patients and can currently be considered as the main notified causes of urethral stenosis (2,4-6).
In urinary catheterization, like in many other nursing procedures, there is a dichotomy between practices, teaching and scientific evidence on the theme (1,6), putting professionals and patients at risk. The nurse is responsible for performing, training and supervising the nursing tea; in urinary catheterization and maintenance and the Nursing education courses for enabling the students, against the background of the scientific reality, of the constant obligation to reassess practices and conducts, through the development of critical sense and the ability to seek professional qualification.
In that context, the objective in this study is to verify how indwelling urinary catheterization has been performed in clinical nursing practice.
Material and method
Descriptive study, developed to describe and document aspects of the urinary catheter insertion. After receiving authorization from the Research Ethics Committee at the University of São Paulo at Ribeirão Preto College of Nursing - USP (Opinion 0961/2008) and after the signing of the Free and Informed Consent Form, the data were collected through an interview in all hospitals of an interior city in the State of São Paulo. Among the 13 hospitals in the city, nine agreed to participate in the research. At each of the participating hospitals, one nurse was interviewed which the hospital itself had designated. All the nurses participated at their institutions in the establishment and implementation of the urinary catheterization delay protocol.
For the purpose of the interview, a semi structured form was used, consisting of demographic information, data to identify the institution and the professional interviewed, besides specific data on the institutional protocols for urinary catheterization delay. The investigated institutions were described in alphabetical order and classified in terms of size as small, medium and large and in terms of funding regimen as public, private or mixed. The results obtained in this phase were analyzed by means of a literature review, using descriptive statistics, and presented in figures and a discursive report (7).
Results
Among the 13 hospitals in the city, nine agreed to participate in the study, five (55.6%) of which were private, three (33.3%) public and one (11.1%) philanthropic. All investigated institutions have a standardized urinary catheterization procedure.
Urinary catheterization is performed upon medical prescription only and the professionals responsible for its practice are the nurse, the nursing team and the medical team. The medical prescription also determines on whether to suspend to use of the urinary catheter.
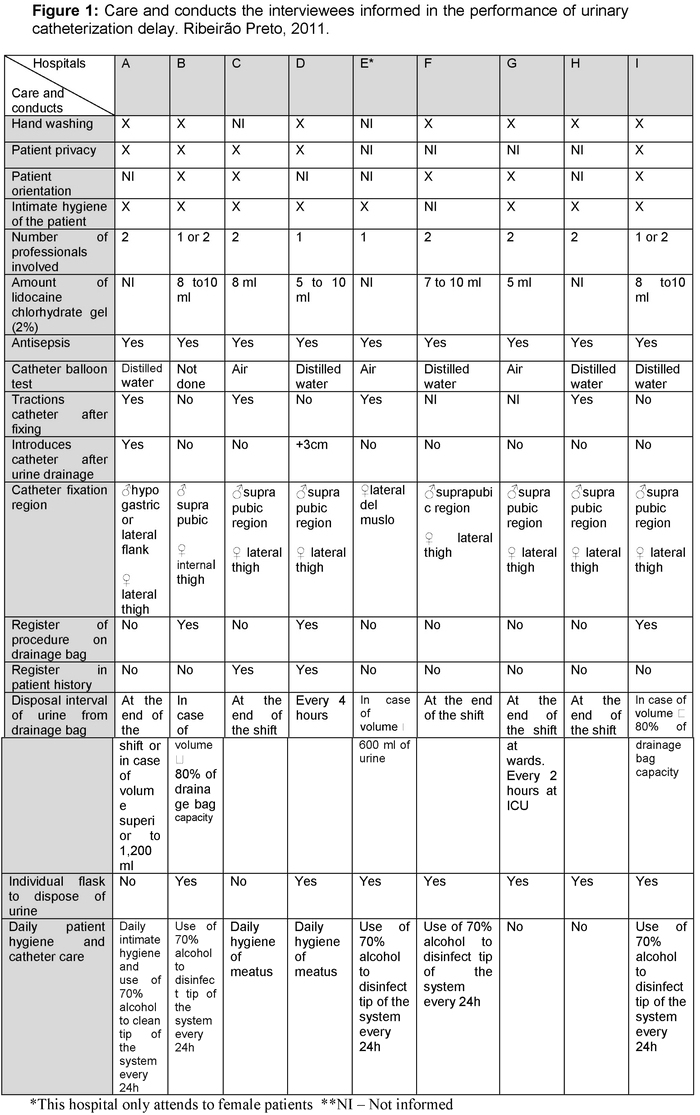
According to the interviewees' description, the following material was described as used to perform the procedure: (9) drainage bag, (9) sterile glove, (9) Foley catheter (12, 14, 16), (8) polyvinylpyrrolidone (PVPI) - topical and anti-germs, (7) round basin, (7) (aqueous, anti-germs) chlorhexidine, (7) tube of lidocaine chlorhydrate gel (2%), (7) distilled water, (6) cotton balls, (6) 20-ml syringe, (5) kidney basin 5, (5) gauze, (4) adhesive tape (plaster, micropore), (3) drape, (3) 10-ml syringe, (2) tray, (1) silicon tube (ICU), (1) pean forceps model, (1) syringe with lidocaine chlorhydrate gel (2%), (1) 70% alcohol. The care and conducts the interviewees performed in the accomplishment of indwelling urinary catheterization have been described in Figure 1.
Discussion
In the nurse's clinical experience, accomplishing procedures is part of common practice, which permeates patient care, is part of professional education and deserves further research.
In view of the different procedures commonly practiced, the study of urinary catheterization reveals that, in the nursing publications on the theme, the set of topics is small and hardly related to the method, innovation and incorporation of new technologies for its accomplishment.
At the investigated institutions, the method and materials to perform the procedure are part of a ritual, jeopardizing patients and professionals. The elaboration of institutional protocols should be strengthened to enhance the quality and safety in the use of this procedure(8,9).
What the professionals is concerned, measures related to hand washing and numbers of human resources can be highlighted in the sample. Hand washing is a simple and essential measure, used to remove the transitory microorganisms that live on the superficial skin layer. Low-cost and highly valuable to prevent hospital infections, it should take place before and after the insertion of the urinary catheter or the handling of the perineum (3,10), which was not evidenced in this study. Limiting factors are the institutions' deficient physical and material structure, lack of compliance and knowledge and the professionals' activity burden (10,11).
Staff dimensioning issues dictates the possibility of engaging yet another professional in the performance of the procedure, which was discussed at seven of the investigated institutions, and is directly linked to the quality of patient care, the reduction of hospital infection rates and financial matters in the organizations
With regard to the patients, the nurse is responsible for guaranteeing their privacy when the procedures are performed, avoiding unnecessary exposure and watching over their comfort. Privacy is both a need and a fundamental right of individual patients, but four subjects did not mention it. When violated, it can cause negative feelings and anguishing experiences (3,12-13). On the other hand, when linked to orientations before the urinary catheterization, it contributes to reduce the anxiety, constraint, to increase the confidence and information exchange with the professional, minimizing risks, discomfort and urethral traumas. The exchange of information on the risks, costs and benefits of the procedures indicated is a patient right and a professional duty (14).
One of the interviewed subjects did not mention hygiene before the introduction of the urinary catheter. This is an important measure to prevent UTI, as it avoids the entry of microorganisms into the urethra. Lukewarm water and soap should be used, without causing any traumas, so that all perineal areas are clean. At the end, the soap should be completely removed and the area should be dried (5,15).
As regards the use of antiseptics, differently from the data the subjects mentioned, these substances should only be used in the aqueous form due to contact with mucous tissue. Neither myths nor rituals are needed concerning how they are administered, although further research is necessary, as no consensus has been reached yet regarding the efficacy of their use (5,16-17).
The use of an appropriate caliber is fundamental to avoid urethral traumas. The internal diameter should always be chosen [corresponding to 1/3 of the catheter number on the French (Fr) scale] according to the patient's comfort and safety. Thinner catheters reduce the risks and the patients' painful feelings (3,14). The use of latex catheters of the types 10 Fr, 12 Fr and 14 Fr was mentioned, besides the use of silicon catheters for intensive care patients at one institution. Although silicon catheters are more expensive, their characteristics are superior as they do not conduct electricity, are resistant to water and to oxidant factors.
To minimize the patients' sensitivity during the procedure, either lubricant or a combination of lubricant and anesthetic substance is needed. The first lubricants and anesthetic substances used in urethral procedures data back to the late XVIIIth and early XIXth century. These were produced based on olive oil, aqueous gels made of vegetable gum which, when associated with anesthetic agents, resulted in great advances in the urethral procedures (18-20).
The basic function of the lubricants is to protect the urethral mucosa through excellent lubrication to reduce the friction. They are assessed better when they permit optical visibility, control of the microbial flora, high electrical conductivity and anesthetic effects. In that sense, they can be used alone or in combination with anesthetics (2% lidocaine) and antiseptics (chlorhexidine). When associated with chlorhexidine, they are of help in contamination processes, but normally cause enhanced sensitivity. When combined with 2% lidocaine, they seem to reduce the sensitivity of the mucosa, although controversies remain in the literature concerning its anesthetic effect. In these situations, care is due because of the adverse effects the absorption of the anesthetic agent causes in injured mucosa (18-20).
Differently from the results found, despite discussions among the authors, in case of urinary catheterization, the use of 20 ml of lubricants is recommended, associated with anesthetics for ten to twenty minutes before the procedure in men and children; for female patients, only the lubricant is recommended.
Testing the balloon in advance serves to confirm its integrity, preventing traumas and the accidental escape of the catheter. This test should always be done with the help of a syringe and distilled water, according to the volume indicated in the manufacturer's instructions (21). After introducing the catheter, the balloon should be inflated safely, that is, after urine draining appears, which is a source of controversy regarding the recommendations (3) on the use of a closed system when inserting the catheter.
The catheter should be fixed using hypo-allergic tape. Correct fixing prevents it from moving in the urethra, preventing undesirable ways and/or accidental removal. In male patients, it should preferably be fixed on the abdomen to prevent the device from pressuring the peniano escrotal angle. In female patients, it should be fixed to the antero-lateral region or internal thigh (22,23).
In the maintenance of indwelling catheters, perineal hygiene has showed to be an effective strategy to reduce the incidence of UTI (24-26). Daily hygiene of the urethral meatus is necessary, using water and soap. During the procedure, the catheter should be mobile, guaranteeing that all areas are cleaned and preventing tissue trauma (3,5,16).
To minimize the risk of urinary infection, closed urinary drainage systems are recommended. These use disposable plastic bags that should be kept below the bladder and without touching the floor. The urine should be disposed of according to the patient's clinical condition, at periodical intervals and using individual recipients, preserving the hygiene measures and standard precautions for the patients and professionals' integrity.
Records of this activity reflect the quality of nurses' work and permits tracking the information. They should contain data on the time, the professionals involved, reasons for the catheterization, material used, procedures accomplished, the patient's response and possible problems. It can be further strengthened through the registering of information on the drainage bag (3,14).
Conclusion
Urinary catheterization delay is a complex procedure that involves the management of material, equipment, staff and processes, besides actions related to respect and patient safety, procedure and documentation, which are closely related to the institutions, their training processes, protocols and funding.
At the investigated institutions, the procedure has been accomplished distinct and not uniformly, unsafely and without complying with the method. As this procedure takes place routinely in patient care, it needs further commitment from the professionals in terms of respect for patient rights and technical precision, besides greater investment in research to clarify aspects for which no evidence is available yet.
Received: November 19, 2013
Accepted: December 22, 2013
References
1. Lenz LL: Cateterismo vesical: cuidados, complicações e medidas preventivas. ACM Arq Catarin Med. 2006; 35:82-91. [ Links ]
2. Mazzo A, Godoy S, Alves LM, Mendes IAC, Trevizan MA, Rangel EML: Cateterismo urinário: facilidades e dificuldades relacionadas à sua padronização. Texto & Contexto Enferm. 2011; 20:333-9. [ Links ]
3. Center for Disease Control and Prevention (CDC): Guideline for prevention of catheter-associated urinary tract infections. Atlanta, EUA. 2009. [ Links ]
4. Canales BK, Weiland D, Reardon S, Monga M: Urethral catheter insertion forces: a comparison of experience and training. Int Braz J Urol. 2009; 35:84-9. [ Links ]
5. Mundy AR, Andrich DE: Urethral trauma. Part I: Introduction, history, anatomy, pathology, assessment and emergency management. BJU Int. 2011; 310-27. [ Links ]
6. Mazzo A, Gaspar AACS, Mendes IAC, Trevizan MA, Godoy S, Martins JCA: Cateter urinário: mitos e rituais presentes no preparo do paciente. Acta Paul Enferm. 2012; 25:889-94. [ Links ]
7. Polit DF, Beck CT, Hungler BP: Fundamentos de Pesquisa em Enfermagem. Métodos, avaliação e utilização. 2004, Porto Alegre, Artmed. [ Links ]
8. Lima LS, Araújo EC,Bezerra SMMS, Linhares FM, Lima AKA. Infecciones del tracto urinario en pacientes con sonda vesical de demora internados en una Unidad de Vigilancia Intensiva en Recife (PE), Brasil. Enfermería Global, 2007; 6(2): 1-11. [ Links ]
9. Torres Alaminos, Ma Angustias. Medidas preventivas para evitar complicaciones de salud derivadas del uso de sondajes vesicales en pacientes lesionados medulares. Enfermería Global, 2013; 12(30): 370-378. [ Links ]
10. Neves ZCP, Tipple AFV, Souza ACS, Pereira MS, Melo DS, Ferreira LR: Hand hygiene: the impact of incentive strategies on adherence among healthcare workers from a newborn intensive care unit. Rev Latino-Am Enfermagem. 2006; 14:546-52. [ Links ]
11. Oliveira AC, Cardoso CS, Mascarenhas D: Precauções de contato em Unidade de Terapia Intensiva: fatores facilitadores e dificultadores para adesão dos profissionais. Rev Esc Enferm. USP. 2010; 44:161-65. [ Links ]
12. Magalhães AMM, Riboldi CO, Dall'Agnol CM: Planejamento de recursos humanos de enfermagem: desafio para as lideranças. Rev Bras Enferm. 2009; 62:608-12. [ Links ]
13. Pupulim JSL, Sawada NO: O cuidado de enfermagem e a invasão da privacidade do doente: uma questão ético-moral. Rev Latino-Am Enfermagem. 2002; 10:433-438. [ Links ]
14. Gasparino RC, Guirardello EB: Sentimento de invasão do espaço territorial e pessoal do paciente. Rev Bras Enferm. 2006; 59:652-55. [ Links ]
15. Geng V, Emblem EL, Gratzel S, Incesu O, Jensen K: European Associattion of Urology Nurses. Good practices in health care. Uretheral catheterization. Section 2. Male, female and paediatric intermittent catheterization, 2006. [ Links ]
16. Leaver RB: The evidence for urethral meatal cleansing. Nurs Stand. 2007; 21:394. [ Links ]
17. Webster J, Hood RH, Burridge CA, Doidge ML, Phillips KM, George N: Water or antiseptic for periurethral cleaning before urinary catheterization: a randomized controlled trial. Am J Infect Control. 2001; 29:389-94. [ Links ]
18. Al-Farsi S, Oliva M, Davidson R, Richardson SE, Ratnaplan S. Peri-uretheral cleaning prior to urinary catheterization in children: sterile water versus 10% povidine-iodine. Clin Pediatr. 2009; 48:656-60. [ Links ]
19. Tzortzis V, Gravas S, Melekos MM, Rosette, JJ: Intraurethral Lubricants: a critical literature review and recommendations. J Endourol. 2009; 23:821-6. [ Links ]
20. Aaronson DS, Walsh TJ, Smith JF, Davies BJ, Hsieh MH, Konety BR: Meta-analysis: does lidocaine gel before flexible cystoscopy provide pain relief? BJU International. 2009; 104:506-10. [ Links ]
21. Gordetsky J, Bendana E, O'Brien J, Rabinowiz R. (Almost): Painless surgery: A historial review of the evolution of intraurethral anesthesia in urology. Urology. 2011; 77:236-7. [ Links ]
22. Perry AG, Potter PA. Guia completo de procedimentos e competência de enfermagem. Rio de Janeiro, Elsevier. 2012; p. 640. [ Links ]
23. Napoleão AA, Caldato VG, Petrilli Filho JF. Diagnóstico de enfermagem para o planejamento da alta de homens prostatectomizados: um estudo preliminar. Rev Eletrônica Enferm. 2009; 11: 286-94. [ Links ]
24. Camara F. R: Cateterismo vesical: enfoque urológico. Departamento de Urologia da FMB/UNESP, 2009. Disponible en: http://www.urologiabotucatu.com.br/cateterismo.asp. [ Links ]
25. Oliveira R, Azevedo N, Cruz I, Andrade M, Santo F.: Urinary tract infection: searching evidence for nursing care. Online Braz J Nurs. 2008; 7. [ Links ]
26. Tsuchida T, Makimoto K, Ohsako S, Fujino M, Kaneda M, Miyazaki T, et al.: Relationship between catheter care and catheter-associated urinary tract infection at Japanese general hospitals: a prospective observation study. Int J Nurs Stud. 2008; 45:352-61. [ Links ]











 texto en
texto en