Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.15 no.41 Murcia ene. 2016
CLÍNICA
Evidence -and Betty Neuman's model- based nursing care to prevent deilrium in the intensive care unit
Cuidados de enfermería basados en evidencia y modelo de Betty Neuman, para controlar estresores del entorno que pueden ocasionar delirium en unidad de cuidados intensivos
Gómez Tovar, Luz Omaira*; Díaz Suarez, Leticia** and Cortés Muñoz, Fabián***
*Master in Nursing. South Colombian University professor, Nurse Intensive Care Unit of the University Hospital Hernando Moncaleano Perdomo de Neiva - Huila. E-mail: omairagt@gmail.com
**Nursing, Intensive Care Specialist, Master in Education. University Sabana professor. Bogotá.
***Nursing, Master in Epidemiology, Professor of Universidad del Bosque. Bogotá - Colombia.
ABSTRACT
Background: Delirium is a fluctuating disturbance in consciousness that is highly prevalent in the intensive care unit. The adult ICU of the Hospital Universitario de Neiva shows an incidence of 28% of delirium patients, this increases morbidity and mortality rates among critical ones; nonetheless, this can be prevented if intervention occurs.
Objective: Determine the effectiveness of to determine the effectiveness of care applied, according to guide nursing care nursing care to prevent delirium in patients, who were hospitalized in the adult intensive care unit, the patients were exposed to environmental stressors.
Methodology: A quantitative, prospective and pre-experimental study was carried out to 49 patients who received assessment with the help of a nursing care guide. Besides the guide, a pretest and a posttest were carried out to evaluate the patients' perception on environmental stressors.
Results: Three out of the 49 patients experienced delirium; this represents a cumulative incidence of 6.12 delirium cases x 100 patients (CI 95%: 1.67-16.1), evident with the Kaplan-Merier curve. Based on the proportion hypothesis testing (Z 0.05 = -1.65) and in contrast to previous results where the incidence of delirium was of 28%, the statistical evidence suffices to demonstrate that the presence of the syndrome is much less frequent in patients to whom the nursing care guide.
Conclusions: The guide prevented the occurrence of delirium in 94% of the patients, regardless of their deliriogenic history, by controlling the continuous noise and artificial light. This is why, minimizing environmental stressors, which results in a more pleasant environment, is a fundamental part of nursing care for the prevention of such a syndrome.
Key words: Delirium, Nursing Care; Prevention of delirium; evidence-based care; Betty Neuman Model.
RESUMEN
Antecedentes: El Delirium es una alteración del estado de conciencia, frecuente en las unidades de cuidado intensivo. En la UCI adultos del Hospital Universitario de Neiva se tiene una incidencia del 28%, esto aumenta la morbimortalidad; sin embargo es prevenible y requiere intervención.
Objetivo: Determinar la efectividad de los cuidados aplicados, según la Guía de enfermería elaborada con evidencia y en base al Modelo de Betty Neuman, para controlar estresores del entorno que pueden ocasionar Delirium, en pacientes hospitalizados en la unidad de cuidados intensivos adulto.
Metodología: Se realizó un estudio cuantitativo, transversal, pre-experimental, donde se aplicó la Guía de cuidados de enfermería a 49 pacientes. Se utilizó el diseño de preprueba y postprueba para conocer la percepción que tenían los pacientes de los estresores del entorno.
Resultados: Los cuidados aplicados según la Guía propuesta, fueron efectivos, ya que previnieron el delirium en el 94% de los pacientes, sólo tres presentaron el evento, representando una incidencia acumulada de 6.12 casos X 100 pacientes intervenidos (IC 95%: 1.67-16.1), evidenciado en la curva de Kaplan-Meier. La prueba de hipótesis de proporciones (Z0.05= -1.65) indica que la presencia de delirium es significativamente menor a la de 2011 (28%).
Conclusiones: Los cuidados aplicados según la Guía propuesta, lograron prevenir la aparición de delirium en 94% de los pacientes a pesar de sus antecedentes de factores de riesgo desencadenantes de delirium. De tal forma que, al minimizar la presencia de estresores del entorno, se favorece un ambiente creado agradable y familiar, y se constituye en un cuidado de enfermería fundamental para la prevención de delirium en UCI.
Palabras clave: Cuidados de Enfermería; Prevención del delirium; Cuidados basados en evidencia; Modelo de Betty Neuman.
Introduction
Patients admitted to the Intensive Care Unit (ICU) are exposed to experience or develop Delirium or acute confusional state, which is defined by the American Psychiatric Association as a disturbance of consciousness, decreased attention to the environment, reduced ability to focus or keep attention; it appears as a change in cognition such as memory deficit, disorientation, language disturbance or perceptive disturbance not explained by previous or developing dementia. The disturbance develops over a short period of time (usually hours to days) and tends to fluctuate during the course of the day(1).
The incidence of delirium is high in surgical patients, especially after cardio-thoracic procedures, with prevalence of 32%(2), as well as in orthopedic procedures, such as hip fracture post-surgery phase, with an incidence of 35%(3). In the hospital population, most studies have reported 10% - 20% prevalence. However, in the ICU, studies report rates of more than 50% in mixed medical and surgical patient groups aged more than 60 years(4). In the adult ICU of Neiva Teaching Hospital (Hospital Universitario de Neiva - HUN), the incidence is 28%.
The pathophysiology of Delirium is determined by an imbalance in the synthesis, release and inactivation of neurotransmitters that regulate the control of cognition, behavior and humor. Dopamine, gamma amino butyric acid (GABA) and acetylcholine are the three neurotransmitters involved in the pathophysiology of Delirium. Dopamine increases the activity of neurons, while GABA and acetylcholine decrease the neuronal excitability. The imbalance in these neurotransmitters results in neuronal and neurotransmission instability(5,6).
There are risk factors that may contribute for patients admitted to ICUs to develop delirium, including endotoxin- and cytosine-induced inflammatory abnormalities, such as the tumor necrosis factor, hypoxemia, improper cerebral perfusion, metabolic disorders, medical therapy, e.g. mechanical ventilation and use of sedatives and analgesics(7). Jiménez et al classify the precipitating factors to develop Delirium by their etiology in predisposing, pharmacological and external or environmental factors(8):
Predisposing factors: Aged over 70 years or more; coming from a retirement home; previous history of depression, dementia, stroke, or epilepsy; alcohol abuse, overdose or use or illegal drugs; hypo- or hypernatremia; hypo- or hyperglycemia; hypo- or hyperthyroidism; hypothermia or fever; renal or hepatic disease; history of heart failure; septic or cardiogenic shock; HIV infection; enteral feeding, bladder or renal catheter and central venous catheter; malnutrition.
Administration of drugs: Psychoactive, sedative-hypnotic medications; benzodiazepines.
Precipitating factors: Noise, physical and social isolation, artificial lighting, lack of calendar clock, and use of physical restrictions (immobilizers or lashing).
Features of the Intensive Care Unit such as constant noise from medical devices, mechanical ventilators, infusion pumps, vital signs monitors, recorders, medical staff, and cell phones, together with continuous artificial lighting, cause hospitalization in the ICU to bring about stress and impaired sleep, along with stress evidenced by disorientation, confusion and even psychosis in a patient, all of which trigger Delirium(9).
Also, several authors confirm that impaired sleep, immobilization and physical restrictions cause function or cognition deficit and are common factors in the ICUs, which are triggers for Delirium(5,9-11).
Among the precipitating factors present in this type of environment, Hewitt highlights the sensory impairment by identifying some types of environmental disturbances that may lead to abnormal behavior: as a noise that gets louder and excessive due to the enclosed place of an ICU, caused by infusion pumps, vital signs monitors, mechanical ventilators, alarms, phones, voices and conversations of the health care staff. As it is not possible to properly value a patient's level of cognition and consciousness, he/she may partially or wrongly understand such conversations and feel fear and anxiety, or this could even disturb the quantity and quality of sleep(12).
However, the main reason for disruption of sleep in the ICU is the environmental noise - almost 17% of common awakenings in the iCu patients were caused by noise(13). Studies in the neonatal ICU have proved that noise can range from 64 to 71 decibels, far above from the recommendations for ICUs (i.e. 45 decibels during the day and 35 at night). The main associated sources identified were external traffic, human factors, and medical devices(14-16). In addition, artificial lighting also influences impaired sleep of critical patients. However, its control is under the responsibility of the nurse; therefore, it must be duly managed as studies report that the main light source involved in impaired sleep of patients was unnecessary(17).
Thus, this disorder constitutes a preventable event by identifying the risk factors existing in a patient hospitalized in the ICU, making a prompt diagnosis, and providing nursing care focused on the prevention and treatment participation by the patient(3). Considering that nursing care must be based on scientific knowledge, developing an approach of care from theoretical foundations that strengthen this profession is necessary. For this reason, this study aims to apply the Betty Neuman's systems model, which proposes prevention as intervention and presents identification and control of environmental precipitating factors to help the patient regain its wellbeing state(18). Thus, this is feasible and very useful in the prevention of complications in the patient hospitalized in the ICU, such as Delirium.
Hence, preventing Delirium in ICU reduces risks for patients, decreases their stay in ICU, days of mechanical ventilation, risks for adverse events, and decreases emotional and economic costs for the patient, family, and health system(15).
The general objective of this study was: To determine the effectiveness of care given, according to the Nursing Guide prepared based on the Betty Neuman's model and Evidence-Based Nursing (EBN) to control precipitating factors from the environment, noise and artificial lighting during the day and at night, with subsequent impaired sleep, factors that may cause Delirium in patients admitted to the Adult Intensive Care Unit (AICU) of the Neiva Teaching Hospital (Hospital Universitario de Neiva - HUN).
Two hypotheses were set up:
Ho: Proportion of Delirium in patients intervened with the Nursing Care Guide based on the Betty Neuman's model and EBN is equal to the proportion of Delirium existing in the polyvalent AICU of the HUN.
Ha: Proportion of Delirium in patients intervened with the Nursing Care Guide based on the Betty Neuman's model and EBN is lower than the proportion of Delirium existing in the polyvalent AICU of the HUN.
Methodology
Quantitative, prospective pre-experimental study. Following the pre-test and post-test design, a single group of patients was recruited, to which the Nursing Care Guide was applied to prevent delirium, and the proportion of delirium in these patients was set out. A simple, random, probabilistic sampling method was applied. For the calculation of the sample size, the experimental studies specific formula was used, as described by Desu and Raghavarao(19). Thus, the adopted sample size was 49 patients, assuming α = 0.05, (β= 0.2 and δ*min = 0.25268026.
Instruments:
The pre-test, post-test and Nursing Care Guide based on concepts of the Betty Neuman's model were prepared, which resulted in the application of her systems theory by means of the secondary prevention for the strengthening of resistance lines and the reconstitution in the ICU patient.
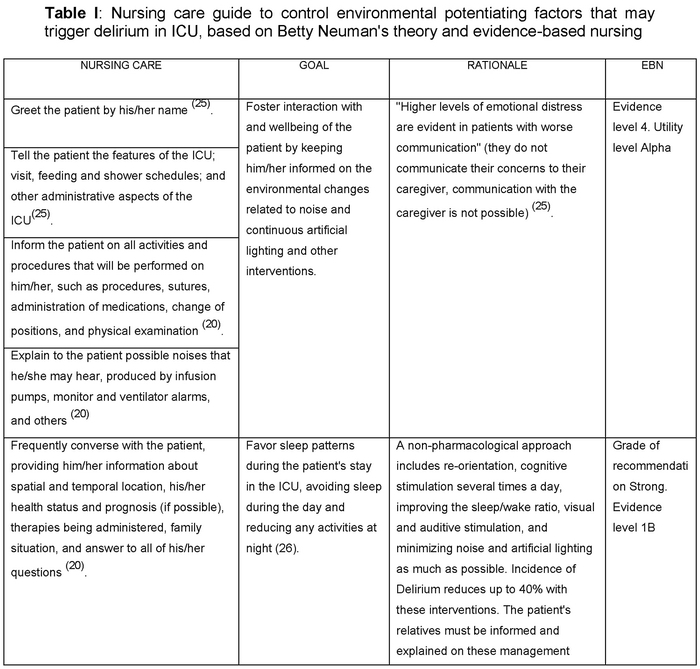
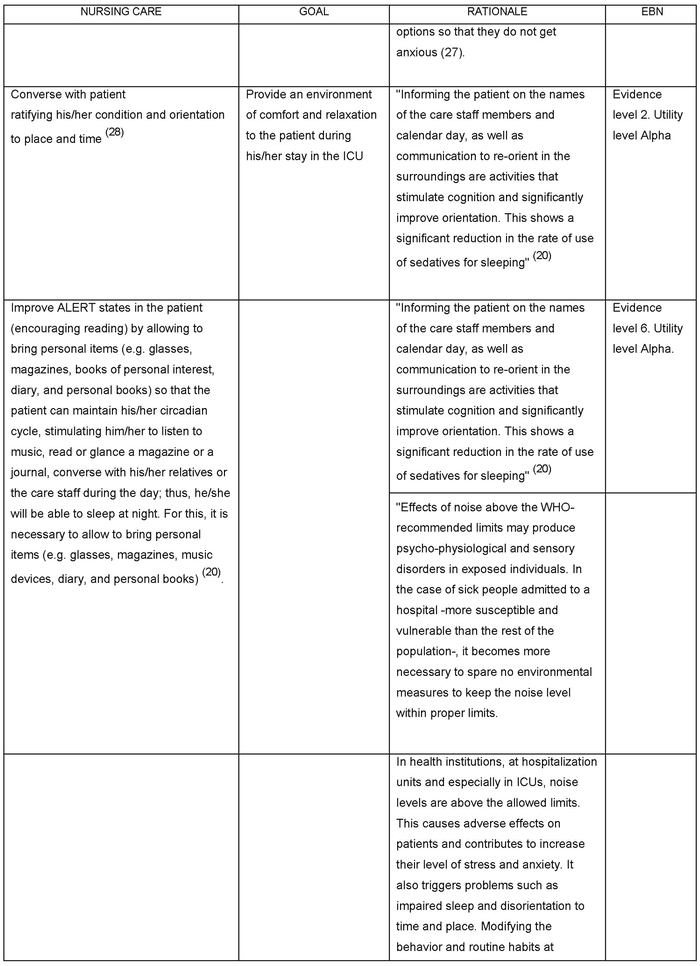
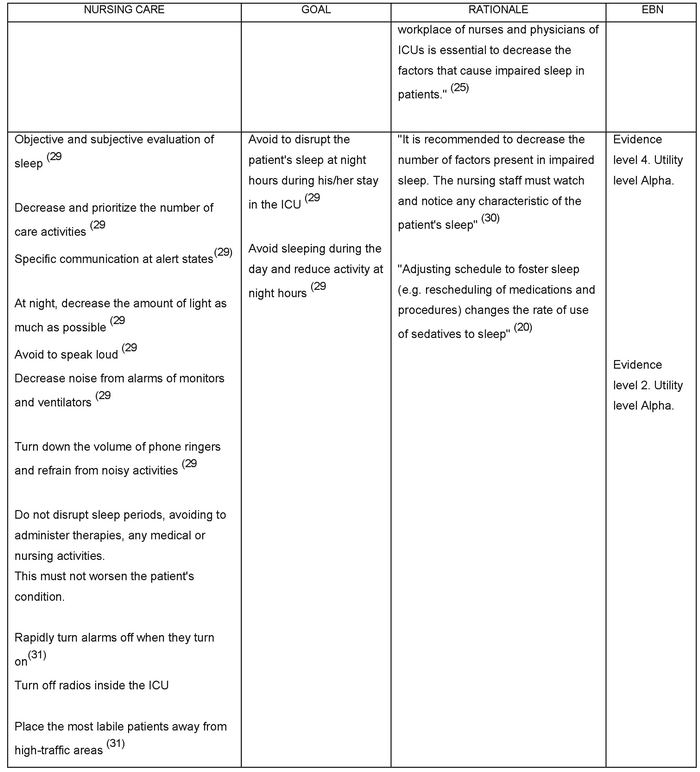
The Nursing Care Guide to control environmental precipitating factors that may cause Delirium is prepared from the Betty Neuman's model, taking account of the environmental precipitating factors noise and day and night artificial light, with subsequent impaired sleep, factors that trigger Delirium. Additionally, scientific evidence was applied with some guidelines taken from the protocol designed by Inouye et al to conduct the research A Multicomponent Intervention to Prevent Delirium in Hospitalized Older Patients(20). Also, other guidelines described by the nurses Rodriguez et al in their research on Acute Confusional state in ICU: Influencing Factors and Nursing Attitude(21) and guidelines taken from the Guide to Diagnosis and Treatment from the Asturias Central Teaching Hospital by Ruiz et al(22) were applied, together with the classification proposed by Alberto Galvez Toro, who adapted the classification used in Evidence-based Medicine to Evidence-based Nursing (EBN), including qualitative research(23). In addition, the classification of evidence according to usefulness and relation to the resolution or no resolution of the problem was taken into account(24).
The Guide is aimed at reducing the environmental precipitating factors noise and continuous artificial lighting, with subsequent impaired sleep, such that its goal is that patients can feel in a created home and pleasant environment that allows them to sleep (see Table I).
Method and Technique
Patients complying with the screening criteria were recruited. These criteria include inclusion and exclusion criteria. The inclusion criteria are the following:
- Have a score between -3 and +3 in the RASS Scale
- Sign the consent form
- Not have Delirium (Negative CAM-ICU)
- Be older than 23 years old
The exclusion criteria are the following:
- Suffer any neurological or psychiatric disorder that prevents him/her from maintaining the state of consciousness.
After this process, the baseline information was collected, and the pre-test to know the perception of the patient regarding the environmental precipitating factors was applied. Subsequently, the Nursing Care Guide was applied, which was performed in a customized manner according to the needs and characteristics of each patient. This Guide was applied together with the RASS and CAM-ICU Scales, continuously, at each shift (morning, afternoon and night) at least for five days. Taking account of these criteria, the total size of the sample is 49 patients.
Finally, on Day 5, after the continuous application of the Care Guide for five days, the post-test was performed, which contained the same items assessed in the pre-test, where the response of patients to the variables intervened with the care guide was evaluated. Gathered information was processed and analyzed with software EpiInfo 3.5.3 and STATA (Version 10 SE; Stata Corporation, College Station, Texas). Statistical tools such as the Kaplan-Meier survival curve was obtained with software Stata for the analysis of the onset of Delirium in participants; analysis of statistical ratios and Shepiro-Wilk test for the age variable.
Results
The study was initiated with the collection of baseline data, that is, concreteness of study patients' physiological and biological characteristics and environment perception. 77.5% of participants were men; the average age was 50 years, ranging from 23 to 92 years of age. Regarding the risk factors for Delirium, 71.4% of participants at recruiting were using medical devices (e.g. central venous catheter, bladder catheter, gastric tube for feeding or drainage, or mediastinal drainage tubes.
Infectious diseases and cardiothoracic surgeries were the main medical history of participants (22.4% each), and the most common diagnoses were post-operative phase of cardiothoracic surgery for myocardial revascularization or valve replacement, and acute coronary syndrome (e.g. acute myocardial infarct) (20.4% each). Regarding the RASS Scale, at recruitment, most patients (67%) scored 0 in the RASS Scale, i.e. alert and calm. The biological variables, noise levels, glycemia, and temperature remained within normal ranges in all participants during the 5 days of follow-up. With respect to the pharmacological factors, 3% of patients were using sedatives, 56% were using analgesics (fentanyl and morphine), and 8% were using vasoactive agents.
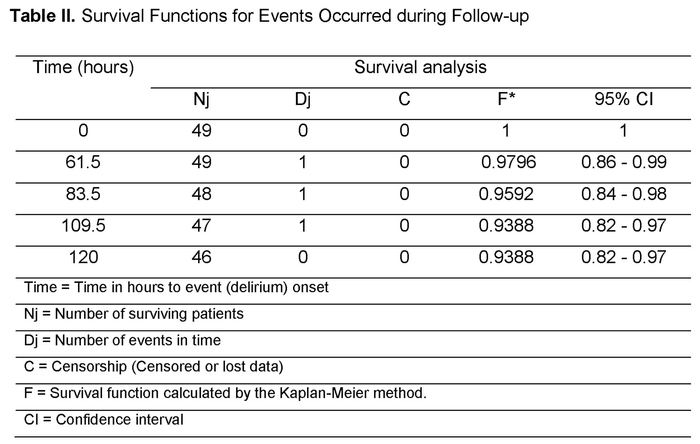
Of the 49 patients to which the Guide was applied, 3 experienced Delirium, representing an accumulative rate of 6.12 Delirium cases X 100 intervened patients, and a density of 5.19 cases X 10.000 patient days (95% CI: 1.67 - 16.1), as shown in Table II. The probability of not experiencing Delirium given that patients were under the application of the Nursing Care Guide at baseline was 97.9%, a figure that decreased to 93.8% at Day 5 of application of the Care Guide. In general, although there were cases of Delirium under the application of the Care Guide, onset of the event was prevented in 94% of patients. This risk behavior is evidenced in the Kaplan-Meier survival curve chart (Table II).
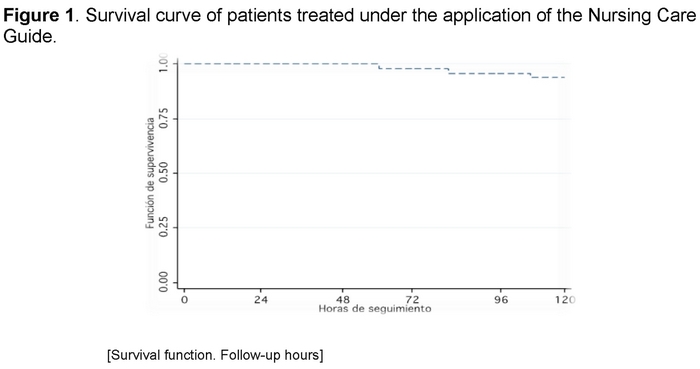
Table II describes the time survival function, understanding survival as the absence of Delirium. Thus, Table II describes the time to event occurrence for the 3 patients
In the Kaplan-Meier survival curve, the time until patients experienced the event is shown. Due to the little presence of Delirium, little decrease in the curve is observed. Therefore, the Nursing Care Guide did prevent Delirium.
In addition, considering the null and alternative hypotheses proposed in this study, a testing of hypotheses of ratio was performed, result of which was Z 0.05= -1.65. This is sufficient statistical evidence to establish that the presence of Delirium is much lower in the 49 patients to which the Nursing Care Guide was applied vs. the previous Delirium percentage (i.e. 28%).
Regarding the environmental precipitating factors, at pre-test, 89.7% of patients had problems to fall asleep. However, upon the application of the Care Guide, there was a great reduction to 24.48%. This shows that the Guide improved the amount of sleep in intervened patients. Only 12 patients remained with difficulties to fall asleep, 2 of which experienced Delirium.
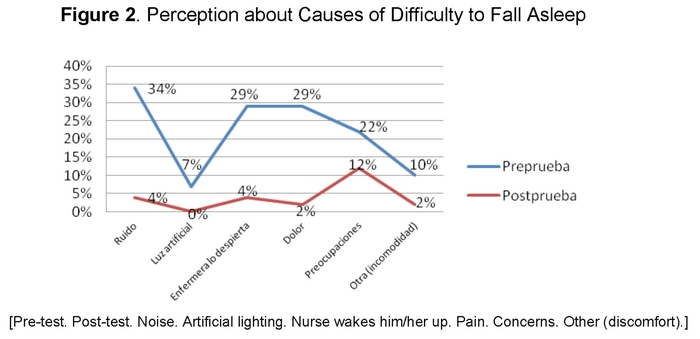
It was found that noise is the main trigger of impaired sleep, as evidenced by the participants at pre-test. However, a significant reduction of noise and artificial lighting is observed at post-test upon the application of the ICU environment-modifying care, by controlling the precipitating factors noise and continuous artificial lighting. Thus, by reducing noise and artificial lighting, patients could sleep and did not experience Delirium. In Figure 2, a significant reduction of noise and continuous artificial lighting perception is evidenced in participants at post-test as precipitating factors that prevent them from sleeping.
Figure 2 shows the significant change of patients in their perception of the atmosphere, corresponding to the ICU's environment. This improved upon the application of the Nursing Care Guide, providing a better environment for patients, which encouraged sleep and prevented Delirium.
Discussion
By analyzing the information obtained, an answer to the research question is found, and the proposed alternative hypothesis is proved. This shows that the Nursing Care Guide to prevent Delirium in ICU was effective despite the presence of risk (pharmacological and predisposing) factors for Delirium.
Risk factors for Delirium, such as sodium disorders, glycemia disorders, infectious disease, severe disease, hyperthermia, and the administration of sedatives (e.g. midazolam), analgesics (e.g. morphine and fentanyl), medical devices, history of cancer, history of cardiothoracic and orthopedic surgery, were taken into account when collecting information and at baseline for each patient. It is then confirmed what has been widely described by Inouye(5), Wesley(10), among others, as causes of Delirium. Therefore, the presence of these factors in patients makes them vulnerable to experience this event. This has been proved in this study since the 3 patients that experienced Delirium had these factors. However, with the Nursing Care Guide it was possible to prevent Delirium in patients with these risk factors, as it was possible to control environmental factors that reduced the possibility of sleep in patients.
Thereby, in this research, the reduction of the precipitating factors noise and continuous artificial lighting, with subsequent impaired sleep, could improve sleep in patients. Eighty percent (80%) of patients stated they had difficulties for sleeping at pre-test, but after applying the Care Guide, this percentage reduced to 24%. This shows that minimizing the sources of noise and continuous artificial lighting favor sleep in ICU-hospitalized patients, as expressed by patients and evidenced in their long periods of sleep and their attitudes of good mood, cooperation and calmness. Thus, stress and likelihood to experience Delirium were reduced. This is described by Blanco et al, and other authors, who confirm that impaired sleep bring about a deficit in function and cognition and are triggers for Delirium(9,10,20).
The 3 patients that experienced Delirium had important predisposing factors at onset, such as multiple medical devices (e.g. central venous catheter, arterial line and bladder tube) for hemodynamic monitoring and administration of drug therapy. This is confirmed by Jiménez(8), who classify it as a patient's predisposing factor that may bring about Delirium, such that the presence of multiple factors increases the likelihood to experience Delirium.
Results found evidence that it is possible to prevent Delirium in ICU by controlling environmental precipitating factors, i.e. guaranteeing long sleep periods to the patient. Although the Nursing Care Guide was continuously applied, at each shift during the 5 planned days, it was not possible to assess for more days the occurrence of the event in long-stay patients in order to confirm the effectiveness of the Guide. Furthermore, other factors that cause Delirium were not controlled, such as patient's predisposing and pharmacological factors, which was a constraint for this study. However, as described in the Betty Neuman's model, maintaining a created pleasant environment reduced the probabilities of affecting the resistance lines, and maintaining secondary prevention -as in this study- may prevent Delirium.
Conclusions
Nursing care applied as per the Guide prepared on the basis of Betty Neuman's theory and Evidence-based Nursing might prevent the onset of Delirium in 94% of patients despite their history of risk factors. Thus, when minimizing the presence of environmental precipitating factors, a created, pleasant and home environment is favored, and basic nursing care is constituted for the prevention of Delirium in ICU.
It is possible to apply the nursing theory, Betty Neuman's in this case, as the basis for Nursing Care, such that this is a great contribution to the discipline as it structures care that resolves patients' needs.
Recommendations
Application of the Nursing Care Guide to prevent Delirium in ICU is convenient, taking account of patients' needs, i.e. customize the care on the Guide, such that these needs are satisfied. This was achieved in this study by managing pain, concerns, stress, and discomfort. Research must continue so that Nursing may contribute with more care guidelines to control other deliriogenic variables, such as reduction of opioids and benzodiazepine, and sodium, glycemia and temperature control.
Received: October 28, 2014
Accepted: 16 January 2015
References
1. APA. American Psychiatric Association. (Internet) Washington Diagnostic and statistical manual of mental disorders, 4th ed. Washington DC: 1994. (citado marzo 2011 ) Disponible en: http://psycnet.apa.org/psycinfo/1994-97860-000. [ Links ]
2. Rincon Hg, Granados M, Unutzer J, Gomez M, Duran R, Badiel M, et al. Prevalence, detection and treatment of anxiety, depression, and delirium in the adult critical care unit. Psychosomatics (Internet). 2001; (citado abril 2011); 42(5):391-396. Disponible en: http://www.sciencedirect.com/science/article/pii/S0033318201704707. [ Links ]
3. Litaker D, Locala J, Franco K, Bronson Dl, Tannous Z. Preoperative risk factors for postoperative delirium. Gen Hosp Psychiatry (Internet). 2001; (citado abril 2011);23(2):84-89. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/11313076. [ Links ]
4. Florez P. Velasquez J. Frecuencia y factores de riesgo del delirium en población geriátrica de la unidad de cuidados intensivos de la clínica Reina Sofía en Bogotá. Revista médica Sanitas (Internet). 2009. (citado Mayo 2012);12(3):66-73. Disponible en: http://www.unisanitas.edu.co/Revista/9/quinto.pdf. [ Links ]
5. Inouye S. Delirium in Older Persons. Review article. The New England of Medicine. Massachusetts (Internet). 2006; (citado agosto 2011); 354:1157-1165. Disponible en: http://www.jewishhospital-cincinnati.com/files/Delirium in Older Persons.pdf. [ Links ]
6. Martinez G. Delirium respuestas pendientes. Revista Hospital clínico Universidad de Chile. (Internet). 2008 (citado marzo 2012);19:330-8. Disponible en: http://www.redclinica.cl/HospitalClinicoWebNeo/Controls/Neochannels/NeoCH6258/deploy/delirium.pdf. [ Links ]
7. Caceres A. Alva J. Manual de psiquiatría. Trastornos mentales orgánicos (Internet). 2a Ed capítulo 10. Lima: UNMSM, 1998 (Actualizado 2002-2008; citado marzo 2011) Disponible en: www.sisbib.unmsm.edu.pe/bibvirtual/libros/psicologia/manualpsiquiatría/cap-10.htm. [ Links ]
8. Jimenez M, Santeadoro A, Lanchado E. Delirium o síndrome confusional agudo. Tratado de geriatría para residentes. Sociedad española de geriatría y gerontología. (Internet) pdf. (citado marzo 2012); Capítulo.18.Pag189. Disponible en: http://www.segg.es/download.asp?file=/tratadogeriatria/PDF/S35-052018II.pdf. [ Links ]
9. Ayllon N. Garrido M. Álvarez M. Gonzalez G. Incidenciais del delirium en cuidados intensivos y factores relacionados. Enferm intensiva, (Internet). 2007; (citado junio. 2011); 18(3):138-43. Disponible en: http://zl.elsevier.es/es/revista/enfermeria-intensiva-142/incidencia-delirio-cuidados-intensivos-factores-relacionados-13109377-originales-2007. [ Links ]
10. Wesly E., Ayumi S., Truman B., Speroff Th., Gordon S, Delirium as a Predictor of Mortality in Mechanically Ventilated Patients in the Intensive Care Unit. United States. JAMA, (Internet). 2004; (citado mayo 2011);291(14):1753-1762. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/15082703. [ Links ]
11. Raul Carrillo E, Sosa García J. Delirium en el enfermo grave. Medicina interna México. (Internet) 2010; (citado zomar 2012);26(2):130-139. Disponible en: http://www.slideshare.net/sandrakitty/48077693-deliriumenelenfermograve1. [ Links ]
12. Hewitt J. Psyco-affective disorder in intensive care units: a review. Journal of clinical Nursing (Internet) 2002, (citado abril 2012);11,(5):575-584. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/12201884. [ Links ]
13. Freedman N, Gazendam J, Levan L, Pack A, Schwab R. Abnormal Sleep/Wake Cycles and the Effect of Environmental Noise on Sleep Disruption in the Intensive Care Unit. American Journal of respiratory and critical care medicine. (Intertet). 2001. (citado sep. 2011);163(2):451-457. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/11179121. [ Links ]
14. Centeno D, Apac A, Sánchez J, Raffo M, Centeno C. Niveles de ruido y fuentes asociadas en una Unidad de Cuidados Intensivos Neonatal. Revista Peruana de Pediatría (Internet). 2005. (citado Mayo 2012);58.(1):12-14. Disponible en: http://sisbib.unmsm.edu.pe/bvrevistas/rpp/v58n1/pdf/a03.pdf. [ Links ]
15. Lawson N, Thompson K, Saunders G, Saiz J, Richardson J, Brown J, Ince N, Caldwell M, Papa D. Sound intensity and noise evaluation in a critical care unit. American association of critical-care nurses (Intertet). 2010. (citado Sep. 2011);19.(6):88-98. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/21041190. [ Links ]
16. Fajardo D, Gallejo S, Argote L. Niveles de ruido en la Unidad de Cuidados Intensivos Neonatal "CIRENA" del Hospital Universitario del Valle, Cali - Colombia. Colombia Médica (Internet). 2007. (citado Ene. 2012);38(4). Disponible en: http://www.bioline.org.br/pdf/Prc07077. [ Links ]
17. Dunn H, Anderson M, Hill P. Nighttime lighting in intensive care units. American association of critical-care nurses (Internet). 2010. (citado Sep. 2011);30.(3): 31-37. Disponible en: http://ccn.aacnjournals.org/content/30/3/31. [ Links ]
18. Neuman B. Fawcett J. The Neuman Systems Model. Vol 1. 4th edition. Boston-Massachusetts: Prentice Hall; 2002. [ Links ]
19. M.M. Desu, D. Raghavarao. Sample Size Methodology. Statistical Modeling and Decision Science. Vol 1.New York: Academic Press, Inc.1997. [ Links ]
20. Inouye S, Bogardus S, Charpentier P, Summers L, Acampora D, Holford T, Cooney L. A Multicomponent Intervention to Prevent Delirium in Hospitalized Older Patients. The New England Journal of medicine. Massachusetts medical society (Internet). 1999; (citado marzo 2011); 340(9):669-676. Disponible en: http://www.nejm.org/doi/full/10.1056/NEJM199903043400901#t=article. [ Links ]
21. J. J. Rodriguez Mondéjar, R. Martín Lozano, R. M. Jorge Guillem, J. Iniesta Sánchez, C. Palazón Sánchez, F. Carrión Tortosa, F. Parra Dormal, A. López Amorós, M. Martínez Huéscar. Síndrome confusional agudo en UCI: factores que influyen y actitud de enfermería. Enferm intensiva, (Internet). 2001; (citado abril 2011);12(1):3-9. Disponible en: http://zl.elsevier.es/es/revista/enfermeria-intensiva-142/sindrome-confusional-agudo-uci-factores-que-influyen-12003852-articulos-originales-2001. [ Links ]
22. Ruiz M, Mateos V, Suarez H, Villaverde P. Síndrome Confusional Agudo (Delirium), Diagnóstico y tratamiento. Hospital universitario Central de Asturias Oviedo. (internet) 2010. (citado mayo 2012) pdf, Pag 10. Disponible en: http://www.hca.es/huca/web/contenidos/websdepartam/pqe/GUIASINDROMECONFUSIONALAGUDO.pdf. [ Links ]
23. Galvez Toro Alberto. Un enfoque crítico para la construcción de la enfermería basada en la evidencia. Rev. Investigación y educación en enfermería. (Internet) 2003, (citado agosto 2012);21(1):50-63. Disponible en: http://aprendeenlinea.udea.edu.co/revistas/index.php/iee/article/viewFile/3037/2805. [ Links ]
24. Orellana A. y Paravic T. Enfermería basada en evidencia. Barreras y estrategias para su implementación. Revista Ciencia y Enfermería de Chile. (Internet) 2007, (citado agosto 2012); 13 (1). Disponible en: http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0717-95532007000100003. [ Links ]
25. Perea Baena Mc. El silencio en la UCI ¿Una utopía? Evidentia. (Internet) 2006 (citado abril 2012); 3(10). Disponible en: http://www.index-f.com/evidentia/n10/241articulo.php (ISSN: 1697-638X). [ Links ]
26. Archury D y Archury L. Sueño en el paciente crítico: una necesidad insatisfecha en la Unidad de Cuidados Intensivos. Investigación en Enfermería: Imagen y desarrollo (Internet) 2010 (citado abril 2012); Vol. 12 No1. Disponible en: http://www.redalyc.org/pdf/1452/145216903003.pdf. [ Links ]
27. Celis E, Besso J, Birchenallc, De La Cal M, Carrillo R, Castorena G, Ceraso D, Dueñas C, Gil F, Jiménez E, Meza J, Muñoz M, Pacheco C, Palizas F, Pinilla D, Raffan F, Raimondi N, Rubiano S, Suarez M y Ugarte S. Guía de práctica clínica basada en la evidencia para el manejo de la sedo-analgesia en el paciente adulto críticamente enfermo. Medicina intensiva Madrid, (Internet) 2007 (citado abril 2012);31 (8). Disponible en: http://www.fsfb.org.co/sites/default/files/guiasdesedacionyanalgesia.pdf. [ Links ]
28. DUEÑAS C, ORTIZ G, MARTINEZ A. Sueño y Delirium en el paciente crítico. Acta Colombiana de Cuidado intensivo. (Internet) 2009 (citado junio 2012); 9(1). Disponible en: http://www.anestesianet.com/actacci/ActaColCuidadoCriticoMar09.pdf. [ Links ]
29. GONZALEZ AGUDELO Marco Antonio. Intervenciones para evitar la deprivación del sueño en los pacientes críticamente enfermos en la unidad de cuidados intensivos. Acta Colombiana de Cuidado intensivo. (Internet) 2010 (citado julio 2012); 10(4). Disponible en: http://www.medintensiva.org/es/guia-practica-clinica-basada-videncia/articulo/S0210569113000855/. [ Links ]
30. COHEN Ana Maria. Calidad del sueño en los pacientes que ingresan en la unidad de cuidados intensivos. Maracaibo. (Internet) 2003 (citado mayo 2012). Disponible en: http://tesis.luz.edu.ve/tde_arquivos/17/TDE-2011-04-25T15:35:52Z-833/Publico/cohen_ana_maria.pdf. [ Links ]
31. Siddigi N, Stockdale R, Britton AM, Holmes J. Intervenciones para la prevención del delirio en pacientes hospitalizados (Revisión Cochrane traducida). (Internet) 2008 (citado marzo 2011) Número 4. Disponible en: http://www.update-software.com/BCP/BCPGetDocument.asp?DocumentID=CD005563. [ Links ]











 texto en
texto en