My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.15 n.43 Murcia Jul. 2016
REVISIONES
The sexuality of women undergoing treatment for breast cancer
La sexualidad de las mujeres sometidas a tratamiento de cáncer de mama
A sexualidade de mulheres em tratamento para o câncer de mama
Lopes, Juliane da Silveira Ortiz de Camargo*; Costa, Lucimar Lopes de Andrade**; Guimarães, Janaina Valadares*** and Vieira, Flaviana****
*Master' s degree program of post graduation Stricto Sensu of the Federal Nursing University of Goias. Study group of women, teenagers and children' s health. Goiania GO. E-mail: julianelopes@hotmail.com
**Nurse specialist in Oncology for the teaching Center from Goias, research and post graduation (CGESP). Goiania, GO
***Nurse female doctor in Pathology. Joined teacher of the federal Nursing University from Goias. Studies group of women, teenager and children' s health. Goiania, GO,
****Nurse female doctor in nursing. Joined teacher of Nursing University of the Federal University of Goias. Studies group of women, teenager and children' s health. Goiania, GO, Brazil.
ABSTRACT
Breast cancer is one of the main problems related to women's health, and the various forms of treatment can lead to bodily changes and significantly alter women's sexuality. The factors involved in sexuality of these women require a targeted approach, as the treatment of women is based on the diagnosis and treatment of health problems and does not necessarily cover all the complexity that the theme demands.
Objective: To evaluate the scientific evidence of interference treatment of breast cancer on women's sexuality. We found twenty-one publications that met the inclusion criteria.
Method: Integrative review conducted in MEDLINE, PubMed, LILACS and SciELO.
Results: The results showed that women with breast cancer may decrease or interrupt their sexual activity during treatment, and many of them have sexual dysfunction with changes in various areas of sexuality, and these changes vary among women in treatment and women who completed treatment. These differences also arise when comparing different types of treatment, conservative and surgical.
Conclusion: It is considered that this study contributes to the foundation of clinical practice of professionals involved in the health of women with breast cancer and the direction of future clinical trials.
Key words: Sexuality; Breast Neoplasms; Sexual dysfunction.
RESUMEN
El cáncer de mama es uno de los principales problemas relacionados con la salud de la mujer, y las diversas formas de tratamiento pueden dar lugar a cambios en el cuerpo y alterar significativamente la sexualidad de las mujeres. Los factores que intervienen en la sexualidad de estas mujeres requieren un enfoque específico, ya que el tratamiento de las mujeres se basa en el diagnóstico y tratamiento de problemas de salud y no cubre necesariamente toda la complejidad que exige el tema.
Objetivo: Evaluar la evidencia científica del tratamiento interferencia de cáncer de mama en la sexualidad de la mujer.
Método: Revisión Integral realizada en MEDLINE, PubMed, LILACS y SciELO. Encontramos veintiuna publicaciones que cumplieron los criterios de inclusión.
Resultados: Los resultados mostraron que las mujeres con cáncer de mama pueden disminuir o interrumpir su actividad sexual durante el tratamiento, y que muchas de ellas tienen disfunción sexual con los cambios en varias etapas de la sexualidad, y estos cambios varían entre las mujeres en tratamiento y mujeres que completaron tratamiento. Estas diferencias también surgen cuando se comparan diferentes tipos de tratamiento, conservador y quirúrgico.
Conclusión: Se considera que este estudio contribuye a la fundación de la práctica clínica de los profesionales que intervienen en la salud de las mujeres con cáncer de mama y la dirección de los futuros ensayos clínicos.
Palabras clave: Sexualidad; Neoplasias de la Mama; Disfunción sexual.
RESUMO
O câncer de mama é um dos principais problemas relacionados à saúde da mulher, e as diversas formas de tratamento podem gerar mudanças corporais e alterar, significativamente, a sexualidade da mulher. Os fatores envolvidos na sexualidade dessas mulheres necessitam de uma abordagem direcionada, visto que o atendimento à mulher se baseia no diagnóstico e tratamento de problemas de saúde e não necessariamente engloba toda a complexidade que o tema exige.
Objetivo: Avaliar as evidências científicas sobre a interferência do tratamento para o câncer de mama na sexualidade das mulheres.
Método: Revisão integrativa realizada na MEDLINE, PubMed, LILACS e SciELO. Foram encontradas vinte e uma publicações que atenderam aos critérios de inclusão.
Resultados: Os resultados mostraram que as mulheres com câncer de mama podem diminuir ou interromper suas atividades sexuais durante o tratamento, e que muitas delas apresentam disfunções sexuais com alterações em diversos domínios da sexualidade, sendo que estas variam entre as mulheres em tratamento e aquelas que completaram o tratamento. Essas diferenças também surgem quando se comparam os diversos tipos de tratamento, conservadores e cirúrgicos.
Conclusão: Considera-se que este estudo contribui para o embasamento da prática clínica dos profissionais envolvidos com a saúde da mulher com câncer de mama e para o direcionamento de pesquisas clínicas futuras.
Palavras chave: Sexualidade; Neoplasia da mama; Disfunção sexual.
Introduction
The breast cancer is one of the biggest problems related to women's health; statistics indicates an increase of its incidence such in developed countries as in the ones still being developed and, according to the world wide organizations of health (WHO), in the decades of 60 and 70 an increase of 10 times were registered in the taxes of incidence, adjusted by age was developed, in the Registers of Cancer of Population-based from several continents(1).
For Brazil, in 2015, was expected 57.120 new cases of breast cancer with an estimate risk of 56,09 cases in every 100 thousand women. It represents the first cause of death from cancer in the feminine population, with 15,93 deaths per 100 thousand women in 2013(2). Associated to a high incidence of breast cancer, they verify physical, psychological and social impacts that compromise even more than women's health (3).
The therapeutics for breast cancer is individual and orientated according to the extension of the disease, its biological characteristics and clinical condition of the woman (4). The chemotherapy and the hormone therapy are the most used types of systemic treatment, the radiotherapy and the surgery for the loco regional treatment (5). Several forms of treatments can generate contradictory feelings between the hope for the cure and fear of confronting corporal changes. These factors can affect the femininity and compromise the relations with the partners, taking the woman to a low self esteem (6) and damage the psychological image that she has of herself and to her sexuality (7). Secondary effects to the treatment as alteration in the production of sexual hormones and precocious menopause can aggravate the picture (8).
Factors involved in women's sexuality with breast cancer necessity of a directed approach, seeing that the service of them is based on the diagnoses and treatment to the health problem and not necessarily include the whole complexity that the subject demands. The highlight from such service happens individually, in the gynecological consultations from the spontaneous demand of each woman who, most times, is restricted to the delimited field of the disease and /or the restoration of the functioning of the organs (9).
Considering that the treatment for the breast cancer can have repercussions on the sexuality, one of the priorities of the public service policies to the women, it becomes necessary the studies about this problematic and to look for scientific evidences for which nurses and other health professionals are guided to supply service of bigger quality in their practice care.
Therefore, the use of integrative revision, with the data lifting about the alterations in the sexuality of women with breast cancer, it becomes of supreme importance in practice of nursing to subsidize the assistance to the women, during and after the treatment, possibly extending the duration of this in benefit to the marital life of the woman with breast cancer.
The use of Practice Based on Evidence (PBE) will incorporate the best scientific evidence for the use of taking decisions in clinical practice and in the individual intervention to the patient (10), just as in the interventions of preventive character to the occurrence of sexual dysfunctions of women in treatment for breast cancer.
Facing the need of analyzing scientific evidences about women's sexuality in treatment for the breast cancer, the following question sustained the study: "what is the interference of the treatment for the breast cancer in the sexuality of women?" Trying to contribute to the enlargement of knowledge for nursing with the impact in teaching, search and assistance, it has as an objective to evaluate the scientific evidences about the interference in the treatment for breast cancer in women's sexuality.
Material and methods
For the reach of the objective proposed in this study, we use the integrative revision as method, which includes the analysis of relevant research that give support for the taking decision and to the improvement of clinical practice This method has six distinct phases, described below: identification of the subject, search for literature, studies categorization, evaluation of the studies included in the revision, interpretation of the results and syntheses of knowledge shown up in the analyzed articles(12).
The bibliographical uplifting was done through consultation in bases of data of relevance for the production of knowledge in health: MedLine (Medical Literature Analysis and Retrieval System Online), PubMed (U.S. National Library of Medicine) and LILACS (Latin American Literature in Sciences of Health) and in the library SciELO (Scientific Electronic Library Online).
To define the sample of selected studies for the present article it was established the following criteria: scientific articles that show the sexuality of women in treatment for breast cancer, published in the last five years (2009 to 2014), for the topicality of the publications referring to the subject, in the Portuguese, Spanish and English languages available online.
As the criteria of the exclusion were established: the reports of informal cases, literature reviews, integrative reviews, qualitative studies (which are not considered as a base for classification of the levels of evidence), consensus, guidelines, books chapter, dissertations, theses, report, news, editorials and non-scientific texts.
The strategy of search based using the lathing of the descriptor standardized "sexuality" and non-standardized "Breast cancer". The standardized term was identified in the Descriptors in Science Health (DeCS).
The data bases were accessed during January 2015. In the first phase, for the selection of articles was realized a careful reading of titles and summaries of all publications located, In order to check the adequacy to the criteria of inclusion and its framework with a guiding question of the first selection. The cases in which the titles and the summary were not enough to define its first selection, these were looked in the whole text. The publications which were not available in the full text in the virtual search were commuted for the evaluation of inclusion.
During the second phase, it was done the reading in the full text of each preselected study. The studies evaluations were done concomitant and independent from two researchers. The third researcher was set when there was divergence in the inclusion or not of the studies. The repetitive studies were excluded in this phase.
For a best comprehension about the data collection and selection of the articles, it was elaborated a flow chart (figure 1), and for a better identification, the selected studies received a sequence of alphanumeric code (E1, E2, E3...).
Between 1.178 articles located in the search, 772 (65,5%) were found in PubMed, 359 (30,5%) in MedLine, 27 (2,3%) in LILACS and 20 (1,7%) in Scielo. From the found studies, 1.082 was excluded for not being appropriated to the criteria of inclusion.
The total of preselected articles, 75 (78, 1%) were excluded, because they did not portray what was the interferences of the treatment for breast cancer in the sexuality of the woman.
The selection made, resulted then in: 09 scientific articles in PubMed, 08 in MedLine, 02 in SciELO, 02 in LILACS, completing a total of 21 scientific articles that answered to the inclusion of the criteria established for the present integrative revision.
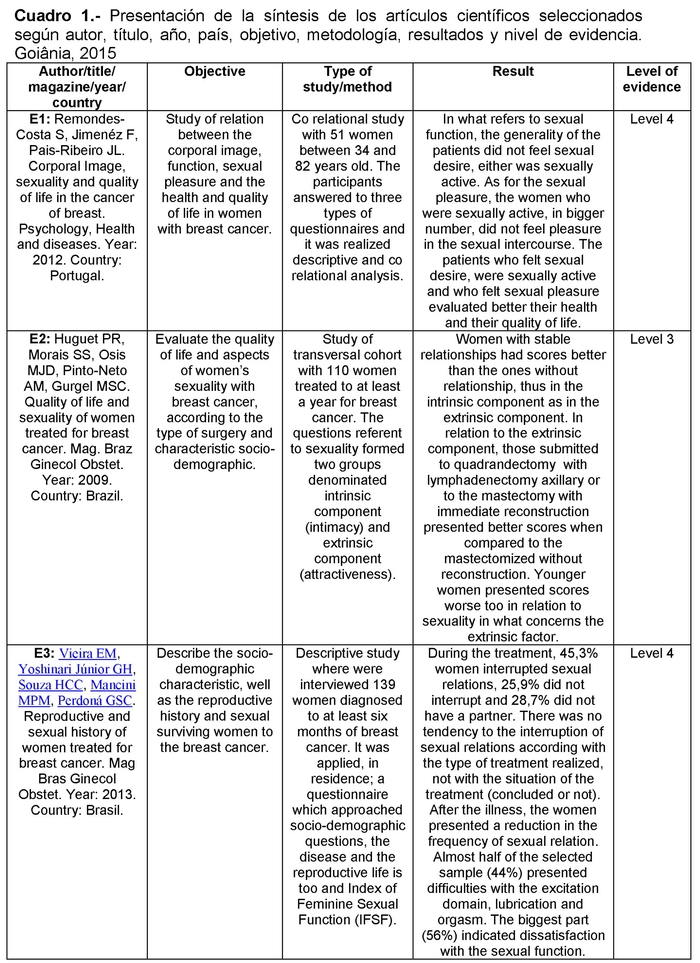
For data extraction a synoptic picture was prepared, with the purpose of categorizing the included studies containing the next information: author/title/magazine/year/country of publication, objective, type of study/method, results and levels of evidence. After that step, it was carried out a careful reading of selected studies, in order to identify possible interference of the treatment for breast cancer in women's sexuality and the levels of study evidence.
The analysis was done in a careful way based in five levels of evidences and four degrees of recommendation from Oxford (13). The levels of evidence are classified in: 1 - Systematic revision of controlled clinical tests and randomized; 2 - Clinical randomized test or observational study; 3 - Cohort study with control group not randomized/sequential study; 4 - Series of cases, case-control study or historically controlled studies; 5 - Mechanisms based in reasoning (opinion without critical explicit evaluation or based in basics principles - physiologic studies or animals studies).
The degrees of recommendations: A (studies level 1); B (studies of level 2 and 3); C studies of level 4); and D (studies of level 5 or problematically inconsistent or inconclusive). The degree of recommendation A represents a higher level of evidence, B moderated, C and D minor level of evidence.
The studies E2, E4, E7, E10, E12, E13, E14, E16, E18, E20, E21, represent the level of evidence 3 with degree of recommendation B (14-24). And the studies E1, E3, E5, E6, E8, E9, E11, E15, E17, E19 presented level of evidence 4 with degree of recommendation C (25-34).
This demonstrates the studies about the sexuality of women with breast cancer have a moderate and weak degree of recommendation, being necessary the realization of new studies about the subject, where the methodology can show levels of evidence with a degree of higher recommendation, making possible for us a better and bigger analyses of the subject, incorporating a better scientific evidence in the use of taking decisions in clinical practice and in the individual intervention in the patient.
The location of the texts in the full text was possible with the access to the Electronic Libraries for 86, 07% of the works at the University of Nursing, and in the Central Library from the Federal University of Goias. Others 13, 93% were commuted.
Results and discussion
Among the twenty articles included, seventeen have predominantly doctors as authors and four are of psychologist's authorship. It becomes evidently the need for a bigger involvement of nurses and nursing academics in this area of knowledge production.
As for the language, we have that 80, 9% (17) from the articles were published in English and only 19, 1% (4) in Portuguese. The predominance of English denotes an intention from most of the authors in spreading their products in a world-wide level.
The syntheses of the twenty one selected articles for the present review are presented considering information referring to the author, scientific title article, name of the magazine, year of publication, country of publication, objective, type of study/method, results and levels of evidence (Chart 1).
Through studies analysis, we have the women with breast cancer reported that they were sexually active before the diagnoses and after; important parcel ceased (22), or decreased the frequency of sexual relation (26).
It is verified that the percentage of women who showed sexual dysfunctions increased according to the elapse of the treatment (23), and there is a deterioration of the corporal image and the sexuality of women with breast cancer, until 6 years after the diagnoses(17).
Women with breast cancer presented lubrication disturbs, satisfaction, desire and excitement, besides the problems related to orgasm and pain during the sexual act (19,33), even though the sexual satisfaction is the domain that presents a higher reduction through the time (24).
The main complaints related to the changes in the sexual well-being are in relation to the alterations of corporal image after the mastectomy, absence of desire, vaginal dryness or painful sex (27), tiredness, confrontation, and feeling less attractive (30), and between those who face such problems, only a small part look for help or external information (27). However, only the perception that has available resources to face the disease provokes a positive influence about the sexual functioning (21).
Many sexually active women present less frequency of sexual activity, reduction of pleasure and discomfort associated to the feeling of emotional separation of the couple or the fear of the partner for the sexual relation (31).
Through the evaluation of the sexuality with the questionnaire Index of Feminine Sexual Function (IFSF) we observed that most women with breast cancer were classified with sexual dysfunction (32), and the scores most affected were the domain of desire, lubrication and orgasm (22), but the women also related a reduction in the frequency of sexual relation, the energy and interest in sex (30).
The sexual desire demonstrates an overthrown in women with breast cancer who are not sexually active, and this rate is predominantly important between older women (25), besides that domain, women with more than 55 years old demonstrated worse results than the younger patients, in the domain of excitement, lubrication and pain (22). In the meantime, younger women presented scores worse than in relation to sexuality concerning the factor of attractiveness (14).
As for sexual pleasure, many women with breast cancer do not feel in sexual relation, but it is noticed that women with more years of schooling show better rates during sexual relation (25).
In relation to the stage of the tumor, we know that women with advanced breast cancer present worse scores of the IFSF and the significant differences were found in the domains of desire and excitement (22). The alterations to the levels of cortical are also associated to the alterations in the dimension of sexual excitement (19).
Women with breast cancer in treatment have lower quantity for sexual fantasies; they masturbate with less frequency, present bigger sexual stress, are less satisfied with their sexual life, have more feelings of guilty about their sexual behavior and have low sexual self-esteem (28).
We notice that women also report problems related to lubrication, orgasm, desire and pain during the sexual act, but in women who finished the treatment they show problems with lubrication, orgasm and pain during the sexual act. Another study demonstrates that the domains of desire and lubrication are the ones which show higher fall in the score in the evaluation powders-treatment (23).
In relation to sexual dysfunction we know that, the trouble with hypoactive sexual desire, the subjective excitement, the genital excitement, orgasm perturbation and dyspaurenia occur most frequently in women in treatment; however the nuisance of sexual aversion and vaginismus are more prevalent in women who completed the treatment (28).
After chemotherapy, the proportion of women who reported sexual problems increase significantly (24), it is noticed there is an important reduction in the scores of IFSF after the conclusion of a chemotherapy cycle which all the domains are affected, with a special reduction in the domains of discomfort/pain, sexual satisfaction (22), lubrication and excitement (24).
The hormone therapy produces higher probability of sexual dysfunction in women with breast cancer, and the therapies associated to radio/chemotherapy and hormone therapy were associated to a risk six times bigger than the disturbance of lubrication and sexual satisfaction (33). The women in use of aromatase inhibitors and with symptoms of vasomotor presented more chance to show problems with sexual function, but the women who use the tamoxifen do not present this propensity (18).
Women who were submitted to surgical treatment for breast cancer and in stable relationship demonstrated better scores than the ones without relationship, in relation to intimacy and sexual attractiveness (14), even so they refer that the mastectomy impacted negatively in marital relation, mainly in relation to the frequency of activities, attraction, satisfaction and sexual pleasure (34).
The quadrantectomyzed or mastectomized and submitted to breast reconstruction presented better sexuality than those mastectomized without reconstruction (14-16). However, independently of the age, the women reported covering their body during the intimate contact after the surgery (34).
The mastectomy creates problems in the domains of sexual desire, excitement and the capacity to reach orgasm, which can last six months to a year after the surgery, but in women who were submitted to breast conservative surgery refer more problems with sexual excitement when compared to a situation before the surgery (20).
Conclusion
The present study demonstrated the women with breast cancer can decrease or interrupt their sexual activities during the treatment, and that many of them show sexual dysfunction with alterations in many domains of sexuality.
It is noticed the advanced age and the stadium of the tumor are factors of risk for the appearance of sexual alterations. And women with a better degree of schooling present better index in relation to sexual pleasure.
There is a difference between the domains of affected sexuality and the sexual dysfunction more prevalent when compared to women in treatment and those who completed. These differences also appear when they are compared to various types of treatment, conservative, and surgical. However, independently of which or how many domains are affected, it is noticeable the sexuality of women with breast cancer is changed significantly during and after the treatment.
This study contributed for the basement of clinic practice from the professionals involved with the health of women with breast cancer and for the direction of future clinic researches. It is possible to notice a scarcity of randomized clinical rehearse and the national studies that address the alteration of sexuality in women with breast cancer.
It is noteworthy the fact the nurse must take the technical orientation responsibility and the attendance from those women in relation to the alteration in sexuality which can appear during the treatment of breast cancer developing actions of promotion to health aiming to a better experience of the sexuality in those women.
Received: June 11, 2015;
Accepted: October 8, 2015
References
1. OMS. Organização mundial da saúde. CID-0: classificação internacional de doenças para oncologia. 3. ed. São Paulo: Editora da Universidade de São Paulo: Fundação Oncocentro de São Paulo, 2005. 239 p. [ Links ]
2. INCA. Instituto nacional de câncer. Atlas da mortalidade. Rio de Janeiro (Brasil): Inca; 2014 (cited 2015 set 27). In: Instituto nacional de câncer (Internet). Available from https://mortalidade.inca.gov.br/MortalidadeWeb/. [ Links ]
3. Ministério da Saúde. Instituto Nacional de Câncer. Estimativa 2014: incidência de câncer no Brasil / Instituto Nacional de Câncer José Alencar Gomes da Silva, Coordenação Geral de Ações Estratégicas, Coordenação de Prevenção e Vigilância. Rio de Janeiro (Brasil): Inca; 2014. 124 p. [ Links ]
4. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Controle dos cânceres do colo do útero e da mama / Ministério da Saúde, Secretaria de Atenção à Saúde, Departamento de Atenção Básica. -2. ed. Brasília (Brasil): Editora do Ministério da Saúde; 2013. 124 p. [ Links ]
5. INCA. Instituto nacional de câncer. Controle do câncer de mama: documento de consenso. Rio de Janeiro (Brasil): Inca; 2004. 39 p. [ Links ]
6. Fabbro MRC, Montrone AVG, Santos S. Percepções, conhecimentos e vivências de mulheres com câncer de mama. Rev. Enfermagem UERJ. 2008;16(4):532-7. [ Links ]
7. Silva LC. Câncer de mama e sofrimento psicológico: aspectos relacionados ao feminino. Psic em Estudo. 2008;13(2):231-7. [ Links ]
8. Santos MCL, Sousa FS, Alves PC, Bonfim IM, Fernandes AFC. Comunicação terapêutica no cuidado pré-operatório de mastectomia. Rev Bras Enferm. 2010;63(4):675-8. [ Links ]
9. Trindade WR, Ferreira MA. Sexualidade feminina: questões do cotidiano das mulheres. Texto Contexto Enferm. 2008;17(3):417-26. [ Links ]
10. Silva AA. Pratica clinica baseada em evidencias na área de saúde. 1st ed. São Paulo: Santos; 2009. 306 p. [ Links ]
11. Mendes KDS, Silveira RCCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto contexto enferm. 2008;17:758-64. [ Links ]
12. Pompeo DA, Rossi LA, Galvão CM. Revisão integrativa: etapa inicial do processo de validação de diagnóstico de enfermagem. Acta Paul Enferm. 2009; 22:434-8. [ Links ]
13. Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, et al. Oxford Centre for Evidence-based Medicine Levels of Evidence. Evidence-based Medicine Levels of Evidence. Developed by University of OXFORD. (Internet). 2011 (cited 2015 fev 23). Available from: http://www.cebm.net/mod_product/design/files/CEBM-Levelsof-Evidence-2.1.pdf. [ Links ]
14. Huguet PR, Morais SS, Osis MJD, Pinto-Neto AM, Gurgel MSC. Qualidade de vida e sexualidade de mulheres tratadas de câncer de mama. Rev Bras Ginecol Obstet. 2009; 31(2): 61-7. [ Links ]
15. Moreira JR, Sabino Neto M, Pereira JB, Biasi T, Garcia EB, Ferreira LM. Sexualidade de mulheres mastectomizadas e submetidas à reconstrução mamária. Rev. bras. mastologia. 2010; 20(4): 177-182. [ Links ]
16. Sabino Neto M, Menezes MVA, Moreira JR, Garcia EB, Abla LE, Ferreira LM. Sexuality after breast reconstruction post mastectomy. Aesthetic Plast Surg. 2013; 37(3):643-7. [ Links ]
17. Lam WW, Li WW, Bonanno GA, Mancini AD, Chan M, Or A, et al. Trajectories of body image and sexuality during the first year following diagnosis of breast cancer and their relationship to 6 years psychosocial outcomes. Breast Cancer Res Treat. 2012; 131(3):957-67. [ Links ]
18. Panjari M, Bell RJ, Davis SR. Sexual function after breast cancer.J Sex Med. 2011; 8(1):294-302. [ Links ]
19. Vaidakis D, Panoskaltsis T, Poulakaki N, Kouloura A, Kassanos D, Papadimitriou G, et al. Female sexuality after female cancer treatment: a clinical issue. Eur J Gynaecol Oncol. 2014;35(6):635-40. [ Links ]
20. Aerts L, Christiaens MR, Enzlin P, Neven P, Amant F. Sexual functioning in women after mastectomy versus breast conserving therapy for early-stage breast cancer: a prospective controlled study. Breast. 2014;23(5):629-36. [ Links ]
21. Quintard B, Constant A, Lakdja F, Labeyrie-Lagardère H. Factors predicting sexual functioning in patients 3 months after surgical procedures for breast cancer: the role of the Sense of Coherence. Eur J Oncol Nurs. 2014;18(1):41-5. [ Links ]
22. Cavalheiro JA, Bittelbrunn A, Menke CH, Biazús JV, Xavier NL, Cericatto R, et al. Sexual function and chemotherapy in postmenopausal women with breast cancer. BMC Womens Health. 2012; 11:12-28. [ Links ]
23. Harirchi I, Montazeri A, Zamani Bidokhti F, Mamishi N, Zendehdel K. i Sexual function in breast cancer patients: a prospective study from Iran. J Exp Clin Cancer Res. 2012; 9:31-20. [ Links ]
24. Webber K, Mok K, Bennett B, Lloyd AR, Friedlander M, Juraskova I, et al. If I am in the mood, I enjoy it: an exploration of cancer-related fatigue and sexual functioning in women withbreast cancer. Oncologist. 2011; 16(9):1333-44. [ Links ]
25. Remondes-Costa S; Jimenéz F; Pais-Ribeiro JL. Imagem corporal, sexualidade e qualidade de vida no cancro da mama. Psic., Saúde & Doenças. 2012; 13(2):327-339. [ Links ]
26. Vieira EM; Yoshinari Júnior GH; Souza HCC; Mancini MPM; Perdoná GSC. História reprodutiva e sexual de mulheres tratadas de câncer de mama. Rev. bras. ginecol. obstet. 2013; 35(2):78-83. [ Links ]
27. Wang F, Chen F, Huo X, Xu R, Wu L, Wang J, et al. A neglected issue on sexual well-being following breast cancer diagnosis and treatment among Chinese women. PLoS One. 2013; 8(9): e74473. [ Links ]
28. Kedde H, Van de Wiel HB, Weijmar Schultz WC, Wijsen C. Subjective sexual well-being and sexual behavior in young women with breast câncer. Support Care Cancer. 2013; 21(7):1993-2005. [ Links ]
29. Kedde H, Van de Wiel HB, Weijmar Schultz WC, Wijsen C. Sexual dysfunction in young women with breast cancer. Support Care Cancer. 2013; 21(1):271-80. [ Links ]
30. Ussher JM, Perz J, Gilbert E. Changes to sexual well-being and intimacy after breast câncer. Cancer Nurs. 2012; 35(6):456-65. [ Links ]
31. Brédart A, Dolbeault S, Savignoni A, Besancenet C, This P, Giami A, et al. Prevalence and associated factors of sexual problems after early-stage breast cancer treatment: results of a French exploratory survey. Psychooncology. 2011; 20(8):841-50. [ Links ]
32. Raggio GA, Butryn ML, Arigo D, Mikorski R, Palmer SC. Prevalence and correlates of sexual morbidity in long-term breast cancer survivors. Psychol Health. 2014;29(6):632-50. [ Links ]
33. Safarinejad MR1, Shafiei N, Safarinejad S. Quality of life and sexual functioning in young women with early-stage breast cancer 1 year after lumpectomy. Psychooncology. 2013; 22(6):1242-8. [ Links ]
34. Andrzejczak E, Markocka-Mączka K, Lewandowski A. Partner relationships after mastectomy in women not offered breast reconstruction. Psychooncology. 2013; 22(7):1653-7. [ Links ]











 text in
text in