Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.15 no.44 Murcia oct. 2016
REVISIONES
Effectiveness of ultrasonography- guided peripheral venous access: an integrative review
Efetividade da ultrassonagrafia na puncao venosa periférica: revisão integrativa Efectividad de la ultrasonografía en la punción venosa periférica: revisión integradora
Efectividad de la ultrasonografía en la punción venosa periférica: revisión integradora Effectiveness of ultrasonography- guided peripheral venous access: an integrative review
Danski, Mitzy Tannia Reichembach*; Oliveira, Andrey Maciel de**; Meier, Marineli Joaquim*** and Pedrolo, Edivane****
*Nurse. PhD in History. Professor of the Graduate Program in Nursing at the Federal University of Paraná. E-mail: mitzyr257@gmail.com
**Nurse. Master of the Graduate Program in Nursing at the Federal University of Paraná.
***PhD in nursing. Docent in Nursing at the Federal University of Paraná.
****Nurse. PhD student of the Graduate Program in Nursing at the Federal University of Paraná. Brazil.
ABSTRACT
Objective: This study aims to identify the found evidence in the literature on the effectiveness of ultrasound technology for success in venipuncture compared to the traditional method for puncture.
Method: An integrative review of literature in Literatura Latino-Americana e do Caribe em Ciências da Saúde (Lilacs) - (Latin American and Caribbean Health Sciences) - and Publicações Médicas (PubMed) - (Medical publications) databases was made from January 2009 to February 2015. Publications in Portuguese, English, or Spanish were included addressing the objectives and/or the research question in the title or abstract and that used systematic reviews, clinical essays, or observational studies as methodology.
Results: Sixteen publications were reviewed presenting a high level of evidence that reinforce the effectiveness of ultrasound for peripheral venipuncture difficult. There was reduction of number of puncture attempts when using ultrasound. The success rate with the use of ultrasound ranged from 70 to 99% and varied with demographic characteristics (sex, age, and skin color), clinical characteristics (diameter and depth of the vein,) and operational characteristics (choice of catheter and skill of the professional performing the procedure).
Conclusion: Ultrasound can increase the success of this procedure, requiring yet more evidence as to the spent time and number of essays for success. The operator ability of the ultrasound equipment as well as clinical, technical, and operational characteristics showed up important factors to be considered for a more effective and safe venipuncture.
Keywords: Ultrasonography; Catheterization peripheral; Technology; Nursing.
RESUMO
Objetivo: Identificar as evidências produzidas na literatura sobre a efetividade da tecnologia ultrassonografia para o sucesso na punção venosa em relação ao Método tradicional de punção.
Método: Realizou-se revisão integrativa de literatura nas bases de dados Lilacs e PubMed, no período de janeiro de 2009 à fevereiro de 2015. Foram incluídas publicações em português, inglês ou espanhol, que contemplaram os objetivos e/ou a questão de pesquisa no título ou resumo e que utilizaram revisões sistemáticas, ensaios clínicos ou estudos observacionais como Metodologia.
Resultados: Compôs-se de 16 artigos, com alto nível de evidência, que reforçam a efetividade da ultrassonografia para a punção venosa periférica difícil. Houve redução do número de tentativas de punção quando do uso da ultrassonografia. A taxa de sucesso com o uso da ultrassonografia ficou entre 70 e 99% e variou de acordo com características demográficos (sexo, idade e cor da pele), clínicas (diâmetro e profundidade da veia) e operacionais (escolha do cateter e habilidade do profissional que realiza o procedimento).
Conclusão: A ultrassonografia pode aumentar o sucesso deste procedimento, necessitando, contudo de mais evidências quanto ao tempo gasto e número de tentativas para o sucesso. A habilidade do operador do equipamento ultrassonográfico, bem como características clínicas, técnicas e operacionais revelaram-se como fatores importantes a ser considerados para uma punção venosa mais efetiva e segura.
Palavras-chave: Ultrassonografia; Cateterismo periférico; Tecnologia; Enfermagem.
RESUMEN
Objetivo: Identificar las evidencias producidas en la literatura sobre la efectividad de la ultrasonografía para el éxito en la punción venosa con relación al Método tradicional de punción.
Método: Se realizó una revisión integradora de literatura en las bases de datos Lilacs y PubMed, en el período de enero de 2009 a febrero de 2015. Fueron incluidas publicaciones en portugués, inglés o español, que contemplaron los objetivos y/o el tema de la investigación en el título o resumen y que utilizaron revisiones sistemáticas, ensayos clínicos o estudios observacionales como Metodología.
Resultados: Compuesto por 16 artículos, con alto nivel de evidencia, que refuerzan la efectividad de la ultrasonografía para la punción venosa periférica difícil. Hubo reducción del número de intentos de punción cuando se usó la ultrasonografía. La tasa de éxito con el uso de la ultrasonografía quedó entre 70% y 99% y varió de acuerdo con características demográficas (sexo, edad y color de la piel), clínicas (diámetro y profundidad de la vena) y operacionales (elección del catéter y habilidad del profesional que realiza el procedimiento).
Conclusión: La ultrasonografía puede aumentar el éxito de este procedimiento, pero es necesario obtener más evidencias sobre el tiempo gastado y el número de intentos para lograr el éxito. La habilidad del operador del equipo ultrasonográfico, así como las características clínicas, técnicas y operacionales se revelaron como factores importantes que deben ser tenidos en cuenta para una punción venosa más efectiva y segura.
Palabras clave: Ultrasonografía; Cateterismo periférico; Tecnología; Enfermería
Introduction
The success of the intravenous therapy begins with the safe and effective establishment of vascular access considering the assertiveness, permeability, and stability of the catheter. With the advances in science in the medical field, it is found that, currently, most of the therapeutic actions are performed by intravenous therapy. In the United States, about 200 million peripheral intravenous catheters are used each year. More than 70% of hospitalized patients in acute situation need this device(1).
In Brazil, despite the lack of these data, the authors agree that, although direct expenses peripheral catheters in hospital bills are relatively small, complications associated with them reverberate in increased hospital stay and then, the care costs(2).
Also, as a prerequisite for the initiation of therapy, the peripheral venous access is sometimes observed as a challenge difficult to overcome, causing vascular trauma and exposing patients to undesirable outcomes such as phlebitis and bruising, as well as more invasive measures such as central venous access.
The failure and multiple puncture attempts maintain a significant relationship with the occurrence of such outcomes and the pain experienced during the procedure. When assessing peripheral venipuncture in adults, it was found that out of 110 of 200 punches studied (55%) showed vascular injury(3).
Despite the difficulties, and to meet the therapeutic needs of the patient in their care, the nursing professional has the challenge of establishing venous access with skill and efficiency. Therefore, various technologies are available, requiring to guide the choices on the best evidence. High Methodological rigor studies, such as clinical trials and systematic reviews can provide for the evaluation of health technologies and make the most appropriate decision.
Thus, it aimed to the effectiveness of nursing interventions and care quality attribute. Effectiveness is the "probability that individuals in a defined population derive a benefit from the application of technology in health directed to a particular problem in actual use"(4).
Among the technologies available to facilitate the establishment of venous access, there is the ultrasound used for peripheral venipuncture. This technology has the advantages compared to the traditional puncture, fewer attempts for successful puncture, fewer complications, and patient satisfaction. No more, there is evidence to demonstrate successful puncture in time less than the traditional punch(5).
It is a practice still uncommon in the Brazilian nursing scenario, and it appears that such benefits still need to be better exploited, particularly their Results in real conditions of use, and the factors related to the success of venipuncture, justifying this research. Given the above, it was sought to subsidies for safer intravenous therapy, safeguarded by an evidence-based nursing practice. Therefore, it aimed to identify the evidence produced in the literature on the effectiveness of ultrasound technology for successful venipuncture over the traditional Method of puncture.
Method
This is an integrative review, a resource of evidence-based practice that allows a comprehensive review of literature through the collection, categorization, evaluation and synthesis of the subject Results in the study, providing practical application. It allows extensive analysis and Discussion based on Methods and Results(6).
This review was in the period from January 2009 to February 2015, and the six steps of Ganong were followed: 1) elaboration of the guiding question and the research objectives; 2) definition of the inclusion/exclusion criteria of the sample and literature search; 3) data collection; 4) Critical analysis of the Results; 5) interpretation of Results, organization and tabulation of information; 6) presentation of the literature review(7).
The formulation of the research question (step 1) included the PICO strategy(8), seeking to solve the question: "Is the use of ultrasound in adult patients more effective than the traditional Method to the success of peripheral venipuncture?"
The initial selection of articles was in October 2014 and considered the following inclusion criteria: be written in Portuguese, English or Spanish; consider the objectives and/or the research question in the title or abstract; and use systematic reviews, clinical trials or observational studies and Methodology. In February 2015, search strategies were repeated to updating the data, adding only four Results by manual search. Thus, there were study designs with a high level of evidence and grade of recommendation, according to the hierarchy of levels of evidence proposed by the Oxford Centre for Evidence-based Medicine and supported by the Cochrane Collaboration(9).
The progress of the research started with the definition of descriptors indexed by the Medical Subject Headings (MeSH) and by the Descriptor of Health Sciences (DeCS). For the searches, PubMed databases for virtual access to the National Center for Biotechnology Information (NCBI); Lilacs and through electronic access to the Virtual Health Library (VHL) were consulted.
From PICO, the following terms related to the selected theme were identified in MeSH: Ultrasonography; Catheterization, Peripheral; Adult. Subsequently, there was a search for the descriptor in PubMed, integrating those words with the following strategy: ((("Adult" [Mesh] OR "Young Adult" [Mesh]) AND "Ultrasonography" [Mesh]) AND "Catheterization, Peripheral" AND (full text [sb] AND "last 5 years" [PDAT] AND (Portuguese [lang] OR Spanish [lang] OR Inglês [lang])).
The search with DeCS identified eight subject descriptors related to the research question: adult; young adult; ultrasound; intervention ultrasound; ultrasound; peripheral catheterization; nursing; effectiveness. With these terms, there were searches conducted integrating them by the Boolean operators "AND" and "OR". Am ong the search Results in the Lilacs, there were only Results for the following strategy selection criteria: ["adult" AND "ultrasound" AND "peripheral catheterization"], from 2009-2014, full text; in Portuguese, English, and Spanish. The search Results in the Lilacs and PUBMED are shown in Figure 1.
The model proposed by Ursi was used as the adopted instrument for data collection (step 3) whose main content describes: "the identification of the original article, Methodological characteristics of the study, assessment of the Methodological rigor of measured interventions and Results found"(10).
This stage has the succeeded critical analysis and synthesis of the articles, which allowed the interpretation and Discussion of the Results to achieve the objectives proposed in this research. Thus, this integrative review is a tool to nursing practice, consolidating the scientific base as an essential element in the decision-making process.
Results
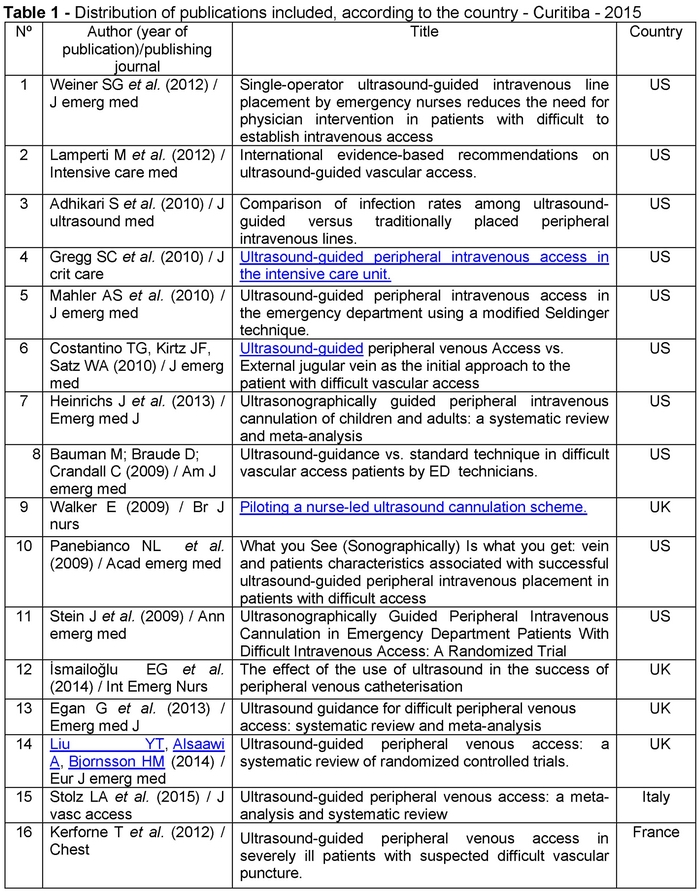
The listed Results, as shown in Table 1 allowed to verify that the United States (US) has most of the publications with the theme discussed in the databases surveyed n=10 (62.5%); followed by the UK with four Results (25%). As for the frequency of authors, only two of 80 authors identified were present in more than one result: Michael Blaivas, 2(11) and 3(12) Results; and Srikar Adhikari: 3(12) and 15(13) results.
Regarding the approach taken on the subject in each publication, it was observed that four articles contain elements of the objectives and/or the question of this research in its title, two of which have the use of vascular ultrasound for nursing explicitly: 1(14), 8(15), 9(16), 12(17).
Regarding the frequency of publications during the period surveyed, it was found that 2009 and 2010 were the most often years, with four publications in each of them; in 2011 there were not publications. Among the Results, two journals had a higher frequency: Emergency Medicine Journal, with three articles; and Annals of Emergency Medicine, with two articles; all other periodicals had found frequency equal to a publication (TABLE 1). It was found that most of the Results were investigated focus of research published in journals in the field of medical emergencies.
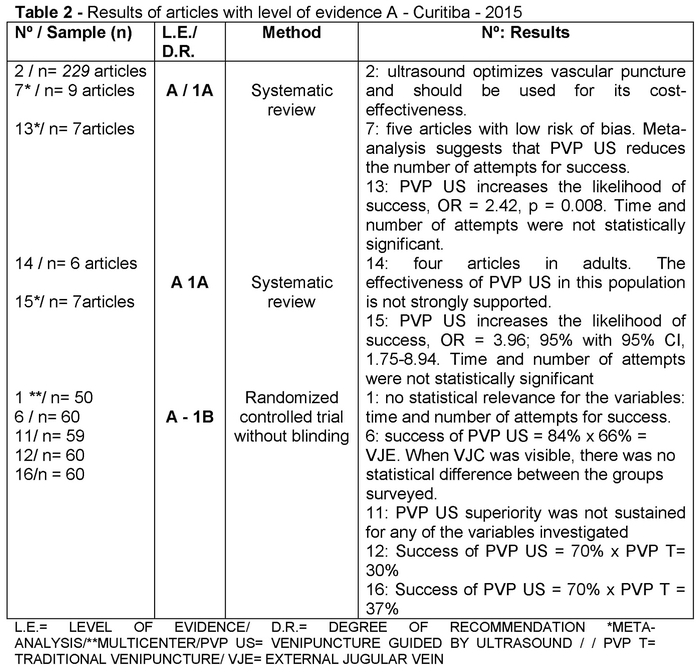
According to the Oxford Center of classification level of evidence, ten studies were classified as level of evidence A (Table 2); six with the level of evidence B (Table 3). When classified according to the Method/result, there were ten publications classified to the level of evidence A, five are systematic reviews, three of which with meta-analysis: 7*(18), 13*(19), 15*(13), all with grade 1A recommendation; five are randomized clinical trials without blinding, a multicenter pilot study (1**), all clinical trials with grade 1B recommendation. Of the 16 Results in the sample, 13 found benefits of ultrasound in peripheral venipuncture.
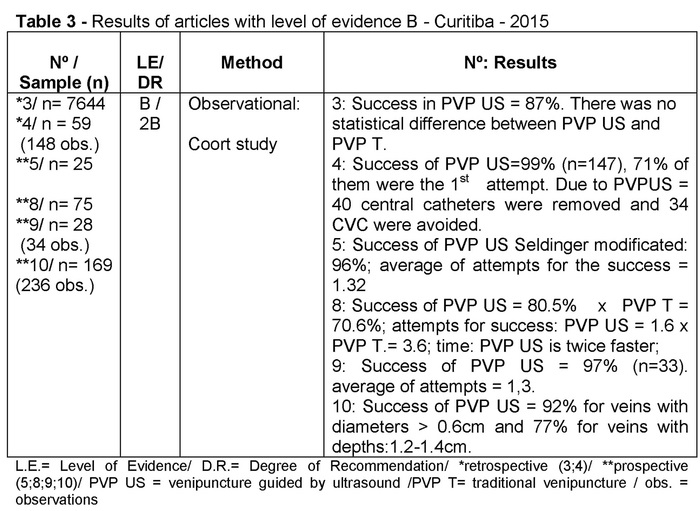
In Table 3, all six articles classified as Level of Evidence (LE) B showed the same degreee of recommendation (DR): 2B.
Of the five systematic reviews, four had ultrasound benefits for peripheral venipuncture. Meta-analysis, result 7(17), held from studies with adults attending critical sectors suggests that the PVP US reduces the number of attempts for success (mean: 0.43; 95% CI.81-.05), with a risk of failure of reason in an attempt to puncture the favorable PVP US (risk ratio: 0.47; 95% CI: 0.87 to 0.26). Results 2 13(19) and 15(13) corroborate these findings.
There were the clinical benefits of PVP US and its satisfactory cost-effectiveness(11); outcomes, however, not repeated in the result 14(20), in which the sample heterogeneity prevented meta-analysis and PVP US did not appear strongly supported.
Among the five trials, three presented Results favorable to the use of peripheral venous puncture guided by ultrasound. This group studies showed that the sample size was similar, one investigated a sample of 50 subjects(14), another with 59, and three studies with 60 participants(07,21,22).
They are observational research with cohort study design, two of which were retrospective, and four were prospective. In only one of these articles were not proven the benefits of PVP US(12).
Other findings, such as demographic, clinical, technical and operational data were found in the analysis and some Results contributed to the effectiveness analysis and decision making, although they were not the objective of this research.
In this sense, the most successful for veins was with diameters greater than 0.6 cm (92%) and depth of 1.2-1.4cm (77%)(23). The Results regarding the choice of the vessel, the basilica veins: 3(12), 5(24), 6(21), 8(15), 11(22), brachial: 3(12), 5(24), 6(21), 8(15), 11(22), and forearm: 3(12), 4(25), 6(21), 7(18), 9(16), 11(22) were found in higher frequencies in the descriptions of veins and puncture sites used, and also featured in the jugular: 7(18), 11(22),antecubital: 3(12), 6(21), 7(18), wrists and hands: 7(18); and feet: 3(12). In Systematic Reviews, 2(11), 7(18), 13(19), 14(20), 15(13) and Results 1(14), 12(17) and 16 was not possible to identify this data.
As the diameter of the catheter, it was found that the most used was 20 gauge (Results nº:1(14), 4(25), 5(24), 9(16), 10(23), 12(17)), followed by 18 gauges: 1(14) 6(21), 3(12), 8(15), not being possible to identify this data in systematic reviews, 2(11), 7(18), 13(19), 14(20), 15(13) and 11(22) and 16(5).
Analysis of complications were observed in three observational studies, found that the occurrence of phlebitis/cellulitis 0.7% inadvertent removal (2.7%) and infiltration (3.4%)(25); the use of ultrasound did not increase the risk of infection related to venipuncture(12); hematomas as 100% of PVP T complications, inadvertent arterial puncture equal to 9.8% in the PVP US and pain (2.4%) also for this Method of blood collection. For this latest study, complications with venous puncture guided by ultrasound are smaller than the traditional Method: 41.5% vs. 64.7%, with higher patient satisfaction with the use of ultrasound: 7.7 x PVP T = 4.4 (P = 0.0001)(15). With the result 12, it was found that the complaint of pain caused by the puncture was smaller with the use of ultrasound: 4.77 ± 1.74 x 6:00 ± 1.98(17).
Discussion
The Results for the success rates of the PVP US showed variations. In a clinical trial, it was found 70% success rate in the group using ultrasound(17); while another study found rates of 84%(21), this one closer to the values found in observational studies. In this group, the success rates ranged from 80.5 to 99%, of which four showed success rates from 92%. Close values were also found in previous studies, Keyes et al., 1999 performed the first study described the use of ultrasound for peripheral venipuncture and found 91% success(26).
In most of the analyzed Results, the average attempts for a success PVP US were less than two. The Results 11(22) and 12(17), the average, was 2.07 attempts. Regarding the number of attempts, it was found in studies presented by the result 7, ultrasound superiority over the traditional Method of puncture.
When comparing the two puncture Methods in adults, the result 8 had a favorable difference to PVP US, averaging 1.6:3.6 attempts(15), similar to another study 1.7:3.7(27). However, for the other Results that used a control group, there was no statistically significant difference in the number of attempts between the two groups. By studying 7, a meta-analysis of the three clinical trials in adults, it was shown that the US reduces the number of attempts for success, although with low statistical significance(18).
From the Results found, those assessed the success in the first attempt with ultrasonography showed mostly hit percentage between 60% and 74% (4:71%, 10:69%; 13:60-74%)(19,23,25). The Results 12:20%(17), 6:50%(21) and 7:57%(18) differ in each group.
As the time is taken to puncture, it was observed a significant difference between the Results. As for the result 11(22), PVP US needed an average of 13 minutes more than the traditional Method. In the analysis of 5(24) and 8(15), this variable was favorable to the investigated intervention: with 68sx420s; and that PVP US twice faster: 26,8sx74,8s(24,15,22). These Results are corroborated by the study that demonstrated an advantage of 11 minutes to the PVP US(27).
The example of the result 13, in which the sample heterogeneity prevented metaanalysis, and PVP US did not appear strongly supported(19), it was found that such heterogeneity also became present in other income and is characterized by Methodological differences and sample.
In the inclusion criteria, for example, the article 12(17) included patients with the venous network without the possibility of palpation or visualization; difficult peripheral venipuncture history (factors such as obesity, edema, dehydration and chronic diseases such as cancer, diabetes, and renal failure). To Articles 1(14) and 11(22), the inclusion criteria adopted was to hold two attempts to PVPT without success; and Article 6(21) had three attempts.
Moreover, the result 8(15) investigated a specific technique of PVP US (Seldinger); 9(16) and 10(23) did not perform the control group; 10 aimed at the effectiveness of PVP US specifically given the clinical characteristics of the patients and their veins(23).
Although not contemplating the purpose of this research, the analysis of the investigation Results weighed clinical, demographic and operational characteristics that may interfere with the success of the puncture. Clinical variables: a history of difficult venous network; wear venous network; edema; pregnancy status; states of shock; dehydration; morbidities such as bleeding disorders, obesity and chronic diseases such as renal failure and vascular disorders, especially related to diabetes mellitus, depth and diameter of the vein 10 - diameter equal to or greater than 3 mm vein(17,23,25).
Demographic variables: gender; age, with greater difficulty given the extremes of age (children and elderly); and skin color. While for the operating characteristics, there were raised information for choosing the catheter and the experience and skill of the professional performing the venipuncture procedure guided by ultrasound(17,23).
The development of skills for the improvement of professional practice requires the rethinking of nurses do every day and has the incorporation of technological innovations an opportunity to overcome difficulties and bring theory and practice(28). Although the result 2(11) submits that the PVP US can improve success for novice equipment operators (level of evidence B with a strong degree of recommendation), it appears that their effectiveness remains relationship with the variable ability of the equipment operator. In this sense, the result 10 states that PVP US requires considerable skill and coordination with the hands and eyes of the performer, suggesting that it use the puncture Method with which they are more familiar(23). However, the author points out that the learning of PVP US is necessary in the absence of PVP US for patients with difficult venous access may expose them to multiple attempts blindly, giving them the perception of technical disability(29).
When assessing the PVP US learning curve by nurses, the authors found that to achieve proficiency nurses needed on average 25 attempts, and security stemmed experience after 50 punch(30).
Conclusion
This review found that there is ultrasound effectiveness of evidence for the success of peripheral venipuncture concerning reducing the number of attempts and with the increase in puncture success rate. The ability of the equipment operator is a factor that affects the success of the procedure, and the result of their learning curve.
A full reading of the analyzed publications showed factors related to the success of peripheral venipuncture, knowledge necessary for choosing the most effective Method for performing this procedure. Although there are studies that prove the benefits of ultrasound for venipuncture, future Brazilian studies are needed to further elucidation of peripheral venous catheterization by nurses.
There are issues to be resolved as time spent and some attempts for success, especially with strong evidence studies, such as clinical trials with solid samples and designs to support the professional decision making.
One of the reasons for conducting research and investment in the qualification of professional nurses to puncture with ultrasound is the possibility of increased safety and patient satisfaction with the difficult venous network.
Received: September 4, 2015
Accepted: October 17, 2015
References
1. Rickard CM, Webster J, Wallis MC, Marsh N, McGrail MR, French V, et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet (Internet). 2012 (cited 2014 nov 4);380:1066-74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22998716. [ Links ]
2. Martins TS, Silvino ZR. The costs of peripheral intravascular device in the values of hospitalization in a pediatric unit. Rev enferm UFPE on line (Internet). 2010 (cited 2014 nov 11);4(2):557-567. Available from: http://www.rese archgate.net/profile/Zenith_Rosa_Silvino/publication/47498466_The_costs_of_peripheral_intravascular_device_in_the_va lues_of_hospitalization_in_a_pediatric_unit/links/02bfe510ac4f81b0a0000000.pdf Acess. [ Links ]
3. Krempser P, Arreguy-Sena C, Barbosa APS. Defining characteristics of peripheral vascular trauma in urgent and emergency: occurrence and types. Esc. Anna Nery (Internet). 2013 (cited 2014 dec 2);77(1):24-30. Available from: http://www.scielo.br/pdf/ean/v17n1/04.pdf. [ Links ]
4. OTA. Office of Technology Assesment. Assessing the efficacy and safety of medical technologies. Washington, DC: U. S. Government Printing Office. 1978. [ Links ]
5. Kerforne T, Petitpas F, Frasca D, Gouget V, Robert R, Mimoz O. Ultrasound-guided peripheral venous access in severely ill patients with suspected difficult vascular puncture. Chest (Internet). 2012 (cited 2014 dec 9);141(1);279-80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22215844. [ Links ]
6. Mendes KDS, Silveira RCCP, Galvão CM. Integrative literature review: a research method to incorporate evidence in health care and nursing. Texto Contexto Enferm (Internet). 2008 out/dez (cited 2015 jan 15); 17(4):758-64. Available from: http://www.scielo.br/pdf/tce/v17n4/18.pdf. [ Links ]
7. Souza MT, Silva MD, Carvalho R. Revisão integrativa: o que é e como fazer. Einstein (Internet). 2010 (cited 2015 feb 2);8(1):102-106. Available from: http://apps.einstein.br/revista/arquivos/PDF/1134-Einsteinv8n1_p102-106_port.pdf. [ Links ]
8. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration (Internet). 2011 (cited 2014 Oct 7) Available from: www.cochrane-handbook.org. [ Links ]
9. OCEBM levels of evidence working group. The Oxford 2011 levels of evidence. Oxford centre for evidence-based. 2011 (cited 2015 mar 3). Available from: http://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf. [ Links ]
10. Ursi ES, Galvão CM. Perioperative prevention of skin injury: an integrative literature review. Rev Latino-Am Enfermagem (Internet). 2006 jan-fev (cited 2014 dec 5); 14(1):124-31. Available from: http://www.scielo.br/pdf/rlae/v14n1/v14n1a17.pdf. [ Links ]
11. Lamperti M, Bodenham AR, Pittiruti M, Blaivas M, Augustides JG, Elbarbary M, et al. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med (Internet). 2012 (cited 2014 nov 5);38:1105-17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22614241. [ Links ]
12. Adhikari S, Blaivas M, Morrison D, Lander L. Comparison of infection rates among ultrasound-guided versus traditionally placed peripheral intravenous lines. J Ultrasound Med (Internet). 2010 may (cited 2014 nov 22);29(5):741-747. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20427786. [ Links ]
13. Stolz LA, Stolz U, Howe C, Farrell IJ, Adhikari S. Ultrasound-guided peripheral venous access: a meta-analysis and systematic review. Emerg Med J (Internet). 2015 feb (cited 2015 mar 10);16(4):321-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25656255. [ Links ]
14. Weiner SG, Sarff AR, Esener DE, Shroff SD, Buchram GR, Switkowski KM, et al. Single-operator ultrasound-guided intravenous line placement by emergency nurses reduces the need for physician intervention in patients with difficult-to-establish intravenous access. J Emerg Med (Internet). 2013 (cited 2014 dec 11);44(3):653-660. Available from: Single-operator ultrasound-guided intravenous line placement by emergency nurses reduces the need for physician intervention in patients with difficult-to-establish intravenous access. [ Links ]
15. Bauman M, Braude D, Crandall C. Ultrasound-guidance vs standard technique in difficult vascular access patients by ED technicians. Am J Emerg Med. 2009 Feb (Internet). 2009 (cited 2014 nov 23);27(2):135-40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19371518. [ Links ]
16. Walker E. Piloting a nurse-led ultrasound cannulation scheme. Br J Nurs (Internet). 2009 jul (cited 2014 dec 5);18(14):854-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19633595. [ Links ]
17. ismailoglu EG, Zaybak A, Akarc FK, Kiyan S. The effect of the use of ultrasound in the success of peripheral venous catheterization. Int Emerg Nurs (Internet). 2014 (cited 2015 mar 12). Available from: http://ac.els-cdn.com/S1755599X14002559/1-s2.0-S1755599X14002559-main.pdf?_tid=3457ad2c-c36e-11e4-b089-00000aab0f6b&acdnat=1425584062_0a0003c20aea74da0172804bc775ca73. [ Links ]
18. Heinrichs J, Fritze Z, Vandermeer B, Klassen T, Curtis S. Ultrasonographically guided peripheral intravenous cannulation of children and adults: a systematic review and meta-analysis. An Emerg Med (Internet). 2013 (cited 2014 nov 7);61(4):444-454. Available from: http://www.slredultrasound.com/Filesandpictures/Vascular19.pdf. [ Links ]
19. Egan G, Healy D, O'Neill H, Clarke-Moloney M, Grace PA, Walsh SR. Ultrasound guidance for difficult peripheral venous access: systematic review and meta-analysis. Emerg Med J (Internet). 2013 jul (cited 2015 mar 25);30(7):521-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22886890. [ Links ]
20. Liu YT, Alsaawi A, Bjornsson HM. Ultrasound-guided peripheral venous access: a systematic review of randomized-controlled trials. Eur J Emerg Med (Internet). 2014 (cited 2015 mar 6);21(1):18-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23880981. [ Links ]
21. Costantino TG, Kirtz JF, Satz WA. Ultrasound-guided peripheral venous access vs. the external jugular vein as the initial approach to the patient with difficult vascular access. J Emerg Med (Internet). 2010 oct (cited 2014 nov 4);39(4):462-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19303238. [ Links ]
22. Stein J, George B, River G, Hebig A, McDermott D. Ultrasonographically guided peripheral intravenous cannulation in emergency department patients with difficult intravenous access: a randomized trial. Ann Emerg Med (Internet). 2009 jul (cited 2014 dec 10);54(1):33-39. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18824276. [ Links ]
23. Panebianco NL, Fredette JM, Szyld D, Sagalyn EB, Pines JM, Dean AJ. What you see (sonographically) is what you get: vein and patient characteristics associated with successful ultrasound-guided peripheral intravenous placement in patients with difficult access. Acad Emerg Med (Internet). 2009 (cited 2014 dec 20);16(12):1298-1303. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1553-2712.2009.00520.x/epdf. [ Links ]
24. Mahler SA,Wang H, Lester C, Conrad SA. Ultrasound-guided peripheral intravenous access in the emergency department using a modified Seldinger technique. J Emerg Med (Internet). 2010 sep (cited 2014 nov 9);39(3):325-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19303241. [ Links ]
25. Gregg SC, Murthi SB, Sisley AC, Stein DM, Scalea TM. Ultrasound-guided peripheral intravenous access in the intensive care unit. J Crit Care (Internet). 2009 (cited 2014 nov 27);25(3):514-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19836193. [ Links ]
26. Keyes LE, Frazee BW, Snoey ER, Simon BC, Christy D. Ultrasound-guided brachial and basilic vein cannulation in emergency department pacients with difficult intravenous access. Ann Emerg Med (Internet). 1999 (cited 2014 nov 5);34(6):711-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10577399. [ Links ]
27. Constantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med (Internet). 2005 (cited 2014 dec 3);46(5):456-61. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16271677. [ Links ]
28. Mendes IAC, Godoy S, Silva EC, Seixas CA, Nogueira MS, Trevizan MA. Educação permanente para profissionais de saúde: a mediação tecnológica e a emergência de valores e questões éticas. Enfermería Global (internet). 2007 (cited 2015 jun 26);10:1-8. Available from: http://revistas.um.es/eglobal/article/viewFile/211/247. [ Links ]
29. Moore C. An emergency department nurse-driven ultrasound-guided peripheral intravenous line program. JAVA (Internet). 2013 (cited 2014 dec 7);18(1):45-7. Available from: http://www.avajournal.com/article/S1552-8855(12)00179-1/abstract. [ Links ]
30. Aulto MJ, Tanabe R, Rosen BT. Peripheral intravenous access using ultrasound guidance: defining the learning curve. JAVA (Internet). 2015 (cited 2014 nov 25);20(1):32-36. Available from: http://www.sciencedirect.com/science/article/pii/S1552885514002128. [ Links ]











 texto en
texto en