Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.16 no.46 Murcia abr. 2017 Epub 01-Abr-2017
https://dx.doi.org/10.6018/eglobal.16.2.245451
Originales
Factors associated with condom use among young men who have sex with men
1Nurse. Specialist in human sexuality. Master student by the Nursing Graduate Program at the State University of Rio de Janeiro (UERJ).
2Nurse. Specialist in Public Health. Veiga de Almeida University.
3Nurse. Veiga de Almeida University.
4PhD in Bioethics. Nurse. Assistant Professor of the Nursing School of the UERJ and of the Nursing Undergraduate Course at Veiga de Almeida University.
5PhD in Public Health. Nurse. Associate Professor of the UERJ Nursing School and Coordinator of the Undergraduate Nursing Course at Veiga de Almeida University.
6PhD in Nursing. Associate Professor at the Nursing School of the UERJ. Rio de Janeiro. Brazil.
Introduction
The increase of HIV infections in Brazil among Men who have Sex with Men (MSM), aged between 15 and 24 years, has the low condom use as one of the factors.
This research aims to describe the factors that are associated or not to condom use among young MSM.
Methodology
Descriptive study, of quantitative nature, using sample for convenience. The scenario was six LGBT nightclubs in the city of Rio de Janeiro - Brazil, selected through a gay nightclub guide. Participants are MSM in the age group between 18 and 24 years who reported having had sex with men. Data collection took place during October 2012. A total of 220 young people were interviewed with the aid of a data collection instrument. Data analysis was performed through the EpiInfo program.
Results
Condom use is associated with disease prevention. The justifications for not using condom in oral sex, in the first and last sexual relation were discomfort, lack of experience/knowledge and confidence in the partner respectively.
Conclusion
This study indicates that the interviewees are susceptible to HIV infection when they abandon or do not use the condom because of their lack of knowledge and/or experience. Guidance and clarification activities with informative material are relevant, considering the vulnerability of this group to STIs.
Keywords Condoms; Sexual Behavior; Male Homosexuality
INTRODUCTION
This study aims at factors associated with the use of condoms among men who have sex with men (MSM) in the young adult age group.
The pandemic caused by Human Immunodeficiency Virus (HIV) is an important challenge for Brazilian and world public health due to its magnitude and extent of damage to populations. Its transmission occurs through unprotected sex, contaminated blood and vertical transmission, and its occurrence is related to individual, collective and social contexts (1.
In Brazil, the epidemic appeared in the early 1980s, being associated with homo/bisexual men, injecting drug users and sex workers2. The supposed selectivity of certain groups to this infection led to the use of the terminology "risk group", so that this denomination marked the historical and social construction of the Acquired Immunodeficiency Syndrome, popularly known by its acronym AIDS 3.
The denomination of risk groups to encompass the population groups most affected by the infection provoked a social response characterized by stigma and discrimination, associating this group with transgressors of social norms, as promiscuous, immoral and addicted people. In Brazil, populations that were not included in this group of individuals considered themselves to be "immune" to the infection, not adopting prevention measures, which led to a change in the epidemiological profile, currently characterized by feminization, pauperization, heterosexualization and interiorization. Thus, the understanding that this disease was restricted to those considered "risk groups" no longer adheres to reality, since all individuals have virtually became vulnerable to it 3.
During the 1990s, the concept of vulnerability was proposed in order to strengthen the response to the HIV pandemic. From this perspective, every individual is exposed and susceptible to HIV infection, and biological, cultural, social, political and behavioral factors are included in addition to epidemiological factors. 4.
The epidemic-spreading process has different impacts on the populations. Identifying and recognizing their differences and specificities become essential actions in the construction of policies directed to the most vulnerable groups.
Behavior is embedded in the concept of individual vulnerability, and the sexual behavior is directly associated with the vulnerability to HIV infection 5. The practice of safe sex is one that adopts, among other measures, the use of condoms, which is the most effective and recommended for the control of sexual infection. Studies show that infrequent use of condoms is the main variable associated with the presence of Sexually Transmitted Infections (STIs)5)(6.
Epidemiological data from the National Department of STD/AIDS and Viral Hepatitis of the Brazilian Ministry of Health show that the population of young gay men is vulnerable. According to research, the prevalence of HIV infection among young MSM aged 17-22 increased between 2002 and 2007 from 0.56% to 1.2%. Regarding the category of exposure of AIDS cases, the age group of MSM aged 15-24 increased from 31.8% in 1998 to 46.4% in 2010. When comparing this group with young people in general, the probability of a young gay to be infected is approximately 13 times greater 2.
A systematic review of the national and international literature has identified that vulnerable sexual practices for STIs are common among the homosexual population. The non-use of condom finds its foundation in the fear of losing pleasure and virility, in the belief in the fidelity of the fixed partner and in the meanings attributed to its use in different cultures. The social contexts of financial, age and gender power and the use of unprotected orgasm-related sexual intercourse by the pornographic media have also been addressed as factors that influence the abandonment of condom use 7.
Due to the representativeness of the HIV epidemic in the population of young gay men in the United States, a qualitative study aimed to explore factors that could be associated with the recent diagnosis of HIV in this population and their perspectives and conceptions about the effectiveness of prevention programs. Data analysis showed that four main themes of vulnerability to infection are recurrent in this population, namely personal risks, lack of qualified education, great access to the internet and need for trained professionals 8.
Vulnerability to STIs has been discussed in other studies, and it has been shown that MSM maintain behaviors that include more sexual intercourse with casual partners, multiple partners, and drug use7)(8)(9. As for the knowledge, a study that investigated 36 thousand young men, aged between 12 and 22 years, identified that 97% know that the use of condoms is the best way to avoid HIV infection. However, their adherence on sexual intercourse does not match the level of knowledge of this population 2.
In this context, it was defined as a problem to be studied: what are the factors that interfere with the use of condoms among young MSM? The study aims to describe the factors that are associated with condom use among young MSM.
The relevance of this study is supported by the vulnerability and impact of the HIV/AIDS epidemic among the homosexual population. The lack of studies, actions and policies aimed at this group that socially suffers from prejudice, discrimination and social invisibility is also a reality10. This research aims to contribute with the discussion about the vulnerability of young MSM to the epidemic and with actions to prevent STI/HIV/AIDS in an equitable manner.
METHODOLOGY
This is a descriptive, quantitative and research with sampling by convenience. The scenario of the study was the nightclubs for the Lesbian, Gay, Bisexual, Transvestite and Transgender (LGBT) public of the city of Rio de Janeiro because it is a space for the socialization of young MSM, where people tend not to hide their sexuality and would be more apt to this type of approach.
The subjects selected to compose this study were MSM, a terminology that covers a variety of sexual identities, including those who do not identify themselves as gays or homosexuals11. Young individuals of this population group have higher infection rates when compared to the general population. Thus, the authors delimited the age group between 18 to 24 years to be studied, considering that, due to legal aspects, it is prohibited the entry of people under 18 years old in nightclubs in Brazil. Only those who claimed to have been sexually related to men (penetrative anal intercourse) were selected to compose the study and who answered, minimally, to all closed questions of the data collection instrument. The criteria of ineligibilities adopted were: to be consuming alcoholic beverages and illicit drugs during the approach and people who are illiterate or with intellectual and physical (visual) impairment.
For data collection, a structured questionnaire with open and closed questions was used, addressing the socioeconomic variables and the use of condom. This instrument was elaborated with reference to the research of the Brazilian Interdisciplinary AIDS Association (ABIA), which had already carried out a study on the needs of HIV/AIDS prevention in the homosexual population of Rio de Janeiro 12. Subsequently, this instrument was tested, by verifying its applicability, considering that the research environment is dynamic.
The collection took place in October 2012, by following the schedule of parties of the most frequented nightclubs by the LGBT public. Seven nightclubs were selected according to a road map entertainment for the gay public. Among these, one of the scenarios was excluded due to its location in an insecure and risk-prone place to the researchers involved. Climatic conditions, such as the presence of rain, were also considered as a factor used for non-attendance in the research scenarios. The approach was performed in the waiting queues standing prior to entry. A total of 338 people participated, and 118 questionnaires were excluded due to non-compliance with the eligibility criteria, making a total of 220 young MSM selected. The justification for the high number of discarded questionnaires was due to the approach used, in which we had the participation of people who attend nightclubs but who had never had sex with men and due to the high number of participants that exceeded the delimited age group.
The ethical and legal aspects of research involving human beings were respected, and the resolution in force at the time of the submission of the research was followed, that is, 196/96 of the National Health Council of Brazil, through the favorable opinion of the Research Ethics Committee of the Veiga de Almeida University under number 101.053. Only after reading, clarifying and signing the Free and Informed Consent Form, the questionnaire was delivered to the participants.
The data were analyzed in simple frequency and total percentage, with the aid of the Epiinfo software.
RESULTS
The socioeconomic characteristics of the research participants are presented in Table 1. The data show that the majority of respondents are 20 years of age (21.4%); considered themselves gays (38.7%); Catholics (31.8%); worked (70%); had family income between 3 and 5 minimum wages (31.4%); were attending higher education (50.9%) and were not in a stable relationship (71.8%).
Regarding condom use, 135 (61.4%) interviewees reported using it at all times, 80 (36.4%) use it sometimes and 5 (2.3%) never use it. In oral sex, condom use is the reverse, 175 (79.6%) do not use it, 32 (14.5%) sometimes use it and only 13 (5.9%) respondents use it at all times. The first sexual intercourse occurred on average at 15.74 years old, with a median of 15.5, mode of 16 and standard deviation of 2.35. Condom was used in the first sexual intercourse by 144 (65.5%) participants, while 76 (34.5%) did not use this method of prevention. At the last sexual intercourse, 162 (73.6%) used condom and 58 (26.4%) did not use it. With regard to sexual partners, 86 (39.1%) reported that they had partners in their lifetime who refused to use condoms. When asked about a hypothetical situation of sexual attraction by a person, but who did not have a condom at the moment, the attitude reported by 188 (85.8%) interviewees would be to refuse to have sex.
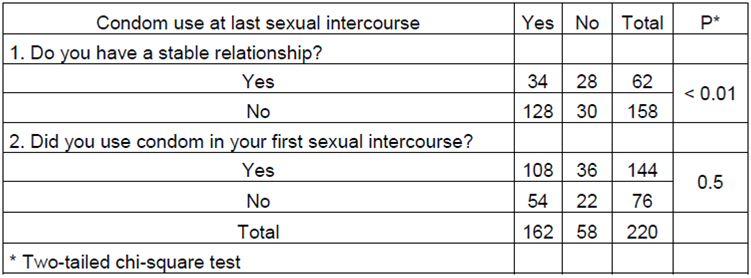
Table 2 shows that there was a significant association between the use of condom in the last sexual relation and the fact of having a stable relationship, whereas the use of condoms at the last sexual intercourse had no significant association when compared to the first sexual intercourse.
Table 2 Association between the use of condoms in the last sexual relation by young men who have sex with men in relation to the first sexual intercourse and stable relationships. Rio de Janeiro, 2012. (n = 220)
Regarding the factors associated with condom use or lack of it among the participants of this research, the results are presented in Table 3 and described below.
Table 3 Factors associated with condom use (or lack of it) in sexual intercourse among young MSM. Rio de Janeiro, 2012. (N=220)

Factors associated with non-use of condoms:
The main factor associated with non-use of condoms, or infrequent use, in oral sex is the discomfort, followed by decreased pleasure, condom taste, trust in the partner and no perceived risk. At the first sexual intercourse the condom was not used due to lack of experience and/or knowledge, due to the moment of the sexual relation, forgetfulness / not having it and trust in the partner. When asked about the use of condom in the last sexual intercourse, the main reasons for the abandonment were trust in the partner, moment, personal preference and forgetfulness/absence of condom.
Factors associated with condom use:
The factors associated with the use of condoms in oral sex were the prevention of STI/AIDS, followed by pleasure. Among the factors related to the use of condoms during the first sexual intercourse are the prevention of STI/AIDS, lack of trust and the imposition by the partner. When questioned about the reason for using it during the last sexual intercourse, the reasons were the prevention of STI/AIDS and the lack of trust in the partner, but some of the interviewees were not able to explain why they had used the condom.
DISCUSSION
Participants in this study were young men who had sex with other men. However, in the questionnaire, researchers let the subjects themselves define their sexual identity, giving them a freedom to tell how they would like to be recognized. Studies point out that certain terminologies have a pejorative meaning, according to the local and personal culture, because of instilled stigma and prejudices. In this study, most interviewees used the terminologies homosexual and gay to define their sexual identity, although the literature considers synonyms of these words13)(14.
The socioeconomic characteristic of the sample is consistent with the Brazilian reality. The Catholic religion is predominant in the country and, despite the Vatican's position against condom use and homosexual relations, it is known that in Brazil the Catholic Church has made important contributions in the prevention of the epidemic and treatment of people living with HIV/AIDS. Research indicates that Brazilian priests seek to propose responses to the epidemic based on the community in which they are inserted, combining the Church's guidelines with their moral conceptions, as they consider the use of condoms as a "lesser evil" than the "greater evil" of death. And with regard to the vision of sexuality, young Catholics assert that the dogmas of the Church are no longer the only principles to guide their conduct15.
However, a study conducted by ABIA with homosexuals from Rio de Janeiro in 2007 found that most of the young people claimed they did not belong to any religion and that this data could be linked to the exclusion of homosexuals by virtue of religious dogmas 12. It is known that religion exerts a strong role of power and moral force, where its foundations normalize and normalize the social structure, interfering in a decisive way in the behavior of its followers. In respect of homossexuality, the violation of rigths still prevails, ans the restriction of citizenship to the LGBT population, perpetuating the individual, social and institutional homophobia that could be reflected in the response of the participants of this research16).
At the time of data collection in the study, Brazil was experiencing a period of economic rise with a heated labor market and a decrease in income inequality, leading to an increase in the middle class. It is noticed that the majority of the participants worked and studied, diverging from a rising reality in the young population, called the "not-not" generation, they not study or work17). Regarding income and schooling variations, a Brazilian survey, conducted in 2008 with 8,000 individuals, found that the higher the income and school level the greater the opportunities for adopting safe sex practices18.
A study in São Paulo, Brazil, with 500 residents of spaces of homosexual sociability, identified that social characteristics were implicated in the use of condoms. Black, low education and poor people had less knowledge about prevention, access to diagnostic tests and condom use19.
Most respondents said they were not in a stable relationship, which can be due to the places where the survey was conducted. A study reveals that MSM prefer meetings in this type of clubs because these places already have their specific public and because they have "dark rooms", which are environments with little or no light, that provide the occurrence of sexual practices, which can be with fixed or casual partners, that have often met each other in that same evening12. The search for casual sexual partners and the use of drugs, which may occur in these spaces, are characterized as risk factors for increasing vulnerability to HIV infection. Studies show that gays and MSM maintain these types of behaviors, which can lead to the abandonment of condom use, especially when it comes to factors such as timing or oblivion19)(20)(21.
Although researches22)(23 diverge on the use of condoms among MSM, comparing them with heterosexuals and indicating that MSM use less condom than heterosexuals, this study could not carry out this projection due to the characteristics of the surveyed sample. However, it is possible to observe that the majority of the interviewees had used condom in the first and last sexual relation. Even so, there is a considerable part that has not been used, exposing themselves to a situation of vulnerability, As evidenced in a study carried out with young gays in Rio de Janeiro, Brazil, in which they identified that 65.5% of the correspondents have already penetrated the anus of a man without even using a condom in their lives12.
Although condom use in the young population group is higher than in any other age group, young people’s sociocultural characteristics make it difficult for them to decide on the use of condoms, such as the belief in invulnerability; the unpredictability of relationships; the moralistic discourses by health/education professionals when they refer to young people’s sexuality; level of knowledge about condom use; emotional and financial dependency; relationship time; difficulties in negotiation; the trust established in affective relationships; the belief that it will diminish pleasure; among others. The non-use of condom in oral sex is linked to the bad taste due to the lubricant, decreased sensitivity and because it "kills the vibe”9)(12)(24.
The use of condoms in the first sexual intercourse is an issue that must be addressed, considering that national data indicate that the it occurs on average at 15 years old25. Adolescence is a period of great transformation and discovery, accompanied by the search for self-identity and the awakening of eroticism. Conducting support and guidance on the various dimensions of sexuality at this stage is still a challenge as it has been a dark, repressed and denied field by society for years. The first relationship involves fear, insecurity and lack of knowledge, factors that may be related to the lack of knowledge or experience for not using the condom as the results of this research points out26.
Nursing as a science that cares for the body and human care faces the multiple facets of caring for population groups, such as those of young adolescents and Young gay people who still lack recognition in care practice, especially in the specific educational and orientation activities for their Age and development, regarding sexuality8. With the creation in 2010 of the National Policy for the Integral Health of Lesbian, Gay, Bisexual, Transvestite and Transsexual people, it is evident for the Brazilian scenario the importance of care that meets the demands and specificities of this group, in addition to summon the professionals of Health, managers and civil society to work together in the perspective of the visibility and access of this population to integral care27.
It is also incumbent upon nursing professionals to promote a dialogue about homosexuality in the social sphere, such as family and school, legitimates heteronormativity by establishing a symbolic condition of domination and stigmatization. The maintenance of a social structure insensitive to the demands of the LGBT population provides a cycle of vulnerability due to the feelings of exclusion and social contempt7.
A study indicates that trust in the partner is one of the main reasons for dropping condom use. Confidence brings about a sense of security, which can result from a stable and everlasting sexual relationship, and from an emotional involvement at the time of the sexual act. This established feeling towards the partner can be seen as a method of preventing STI/HIV and that proposing their use generates mistrust in the couple12.
A study, with people attending spaces of homosexual sociability, identified that after some time of relationship 25% of the interviewees interrupted the use of the condom with their sexual partners, being the main reasons to trust and to carry out the HIV test. This data reinforces a conception of risk perception and harm reduction by the interviewees, when seeking strategies to abdicate the use of protection against belief in fidelity and non-infection due to sexually transmitted diseases19.
Regarding the abandonment of the condom, due to the moment of sexual intercourse, some studies present data that corroborate this situation. It is believed that the human's inherent need for pleasure and the impulse provoked by momentary desire may be tied to unprotected sexual practice20)(24)(28. Impulsive desire often has the incentive of friends or specific situations such as parties and meetings, sometimes stimulated by the use of alcoholic beverages and drugs, this set of factors leads to a situation of vulnerability to infection29.
There are also factors related to the scenario of sexual intercourse, which may also be implicated in the abandonment of condom use by the current situation. The study found that in scenarios of sexual unpredictability and / or having a difficult structure, there was a greater risk of abandonment of condom use, such as in the darkroom, in the street, in the square, in the park or in the public bathroom19).
Abandonment of condom use in sexual relationships can also be a conscious and desired choice, even knowing the risks involved in STIs. Studies on barebacking (unprotected anal intercourse among men who have sex with men intentionally) evidence that their practitioners refer to the pleasures of unprotected sex because of increased physical stimulation, intimacy, and the feeling of being emotionally closer or connected to the partner. Also, the Internet has been pointed out as a great facilitator for the meeting of people who prefer barebacking practices30)(31. Another study evidenced that the loss of pleasure associated with the use of condoms was considered a fundamental factor for their abandonment28.
The use of condoms in relationships is a challenge for sexual practice as it pervades individual behavior and affects the collective behavior and the full range of historical-cultural contexts in which the couple or individuals are involved. In this investigation, it was possible to observe that the partners acted positively by encouraging the use of the condom and there were no reported situations of abandonment of the condom use by imposition. However, the influence of the partner on the use or not of the condom has already been discussed in other studies and may be an incisive or veiled desire, permeated by affective relationships and power. Power relations between sexual partners were evidenced in MSM relationships. The characteristics of age, socioeconomic, sexual preference and gender are factors of vulnerability in the relationships between MSM. The dependencies, inequalities, oppressions and hierarchies, in these contexts, expose to vulnerable situations those that are in “inferior” circumstances7)(12. MSM have difficulty to negotiating the condom with fixed partners, especially when they assume the passive sexual role, or when they are poorer, feminized, older, or black19.
In a survey carried out in Mexico on factors associated with the inconsistent use of condoms among MSM, it was possible to verify that power relations and the use of psychoactive substances are obstacles to the use of condoms. It was evidenced through the multivariate logistic regression analysis that younger individuals, with middle income and negative attitudes regarding condom use, who had consumed alcohol and drugs, and declared themselves publicly as homosexuals were the most prone to abandoning condom use32. It should be noted that although studies portray the association of psychoactive substances with non-use of condoms, in this research the young people did not verbalize this situation, which prevents us from verifying this association among the young investigated.
CONCLUSION
The findings indicate that condom use is common in the sexual relations of the surveyed public, with the exception of oral sex. At the first sexual intercourse, the main factor pointed to the abandonment of condom use is the lack of experience / knowledge and, in the last sexual relation, the confidence in the partner.
This study is consistent with other investigations in identifying that young MSM abandon condom use for a number of individual, social, and programmatic factors. However, some limitations of this research should be indicated, such as: 1) The instrument chosen for data collection did not favor the capture of subjective aspects about the factors associated with the use of condoms in sexual relations. 2) The study scenario, because it is a dynamic environment, made it difficult to use an objective instrument that favored the participation of the subjects and did not affect the entrance flow in the nightclubs.
It is concluded that strategies are needed to encourage condom use and attendance at health facilities to perform tests for the early diagnosis of STI / HIV or post-exposure prophylaxis and are considered important tools to minimize the spread of new infections. However, actions aimed at the homosexual population are still timid, corroborating the vulnerability of this group.
Nursing care in the integral care of adolescents and young people should be based on the new social arrangements and the specificities of individuals and groups. It is up to nursing as a profession to act in the planning, execution and evaluation of health care and educational plans that promote the prevention of STI / HIV / AIDS, with emphasis on the most vulnerable groups. Therefore, it is necessary to intensify prevention actions with distribution of condoms, allocation of banners and informative materials, minimally, in the spaces of socialization of this population group; Use of the internet and telephone applications as technological resources for health promotion; Implementation of health policies in schools; Accessibility and humanization of services for young gay men, homosexuals and MSM; To provide visibility to the LGBT population in the social setting, in health policies and institutions.
REFERENCIAS
1. Lima TC, Freitas MIP. Comportamentos em saúde de uma população portadora do HIV/Aids. Rev bras enferm.2012; 65(1): 110-5. [ Links ]
2. Brasil. Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento Nacional de DST/Aids e Hepatites Virais. Boletim Epidemiológico AIDS/DST. Brasília: Ministério da Saúde, 2011. [ Links ]
3. Gomes AMT, Silva ÉMP, Oliveira DC. Social representations of AIDS and their quotidian interfaces for people living with HIV. Rev Latino-Am Enfermagem. 2011; 19(3): 485-92. [ Links ]
4. Ayres SJRCM, Calazans GJ, Saletti F, Haraldo C, França JR. Risco, vulnerabilidade e práticas de prevenção e promoção da saúde. In: Campos GWS, Minayo MCS, Akerman M, Drumond M Jr, Carvalho YM,organizadores. Tratado de saúde coletiva. Rio de Janeiro (RJ): Fiocruz; 2006. p. 375-417. [ Links ]
5. Cruzeiro ALS, Souza LDM, Silva RA, Pinheiro RT, Rocha CLA, Horta BL. Comportamento sexual de risco: fatores associados ao número de parceiros sexuais e ao uso de preservativo em adolescentes. Ciênc saúde coletiva. 2010; 15 (suppl 1): 1149-58. [ Links ]
6. Griensven FV, Wijngaarden JWLV. A review of the epidemiology of HIV infection and prevention responses among MSM in Asia. AIDS. 2010; 24 (suppl): 30-40. [ Links ]
7. Cunha RBB, Gomes R. Os jovens homossexuais masculinos e sua saúde: uma revisão sistemática. Interface (Botucatu) [Internet]. 2015 Mar [cited 2015 Nov 29]; 19(52): 57-70. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1414-32832015000100057&lng=en [ Links ]
8. Flores DD, Blake BJ, Sowell RL. "Get them while they're young": reflections of young gay men newly diagnosed with HIV infection. J Assoc Nurses AIDS Care. 2011; 22(5): 376-87. [ Links ]
9. William L, Jeffries IV. The number of recent sex partners among bisexual men in the United States. Perspect Sex Reprod Health. 2011; 43(3): 151-157. [ Links ]
10. Chonody JM. Measuring Sexual Prejudice Against Gay Men and Lesbian Women: Development of the Sexual Prejudice Scale (SPS). J Homosex. 2013; 60(6): 895-926 [ Links ]
11. Unaids. Action framework: universal access for men who have sex with men and transgender people. Geneva: Unaids, 2009. [ Links ]
12. Associação Brasileira Interdisciplinar de Aids (ABIA). Levantamento de necessidades em HIV/AIDS na população homossexual do Grande Rio: Jovens de 18 a 24 anos e homens soropositivos. Rio de Janeiro: ABIA, 2008. [ Links ]
13. Rios K. Right-wing authoritarianism predicts prejudice against "homosexuals" but not "gay men and lesbians". J Exp Soc Psychol. 2013; 49(6): 1177-83. [ Links ]
14. Knauer NJ. Identity/Time. Laws. 2013; 2: 362-75. [ Links ]
15. Rios LF, Aquino FL, Muñoz-Laboy M, Oliveira C, Parker R. Católicos, fidelidade conjugal e Aids: entre a cruz da doutrina moral e as espadas do cotidiano sexual dos adeptos. Debates NER. 2008; 9(14): 135-56. [ Links ]
16. Trindade Mesquita D, Perucchi J. Não apenas em nome de Deus: discursos religiosos sobre homossexualidade. Psicol Soc. 2016; 28(1): 105-114. [ Links ]
17. Camarano AA, Kanso S. O que estão fazendo os jovens que não estudam, não trabalham e não procuram trabalho? In: Instituto de Pesquisa Econômica Aplicada (IPEA). Mercado de Trabalho. Brasília: IPEA; 2012. p. 37-44. [ Links ]
18. Brasil, Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento Nacional de DST, Aids e Hepatites Virais. Pesquisa de conhecimentos, atitudes e práticas na população brasileira 2008. Brasília: Ministério da Saúde, 2011. [ Links ]
19. Antunes MC, Paiva VSF. Territórios do desejo e vulnerabilidade ao hiv entre homens que fazem sexo com homens: desafios para a prevenção. Temas psicol. [Internet]. 2013 Dez [citado 2016 Abr 16]; 21(3): 1125-43. Disponível em: http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1413-389X2013000300019&lng=pt [ Links ]
20. Balán IC, Carballo DA, Ventuneac A, Remien RH. Intentional condomless anal intercourse among Latino MSM who meet sexual partners on the Internet. AIDS Educ Prev. 2009; 21(1):14-24. [ Links ]
21. Grov C. HIV risk and substance use in men who have sex with men surveyed in bathhouses, bars/clubs, and on Craigslist.org: venue of recruitment matters. AIDS Behav. 2012; 16(4):807-17. [ Links ]
22. Widman L, Golin CE, Grodensky CA, Suchindran C. Do Safer Sex Self-Efficacy, Attitudes toward Condoms, and HIV Transmission Risk Beliefs Differ among Men who Have Sex with Men, Heterosexual Men, and Women Living with HIV? AIDS Behav. 2013; 17(5): 1873-82. [ Links ]
23. Casalino E, Choquet C, Leleu A, Hellmann R, Wargon M, Juillien G, et al. Trends in Condom Use and Risk Behaviours after Sexual Exposure to HIV: A Seven-Year Observational Study. PLoS ONE. 2014; 9(8): e104350. [ Links ]
24. Alves CA, Brandão ER. Vulnerabilidades no uso de métodos contraceptivos entre adolescentes e jovens: interseções entre políticas públicas e atenção à saúde. Ciênc saúde coletiva. 2009; 14(2): 661-70. [ Links ]
25. Paiva V, Calazans G, Venturi G, Dias R. Age and condon use at first sexual intercourse of brazilian adolescents. Rev Saúde Pública. 2008; 42(1):45-53. [ Links ]
26. Almeida ACCH, Centa ML. Parents experience with the sexual education of their children: implications for nursing care. Acta paul enferm. 2009; 22(1):71-6. [ Links ]
27. Ministério da Saúde (BR). Política nacional de saúde integral de lésbicas, gays, bissexuais, travestis e transexuais. Brasília: Ministério da Saúde; 2010. [ Links ]
28. Calabrese SK, Reisen CA, Zea MC, Popen PJ, Bianchi FT. The pleasure principle: the effect of perceived pleasure loss associated with condoms on unprotected anal intercourse among immigrant Latino men who have sex with men. AIDS Patient Care STDS. 2012; 26(7):430-5. [ Links ]
29. Barreto ACM, Santos RS. A vulnerabilidade da adolescente às doenças sexualmente transmissíveis: contribuições para a prática da enfermagem. Esc Anna Nery Rev Enferm. 2009; 13(4): 809-16. [ Links ]
30. Silva LAV. Barebacking e a possibilidade de soroconversão. Cad Saúde Pública. 2009; 25(6): 1381-9. [ Links ]
31. Carballo-Diéquez A, Ventuneac A, Bauermeister J, Dowsett GW, Dolezal C, Remien RH, et al. Is 'bareback' a useful construct in primary HIV-prevention? Definitions, identity and research. Cult Health Sex. 2009; 11(1): 51-65. [ Links ]
32. Mendoza-Pérez JC, Ortiz-Hernández L. Factores asociados com el uso inconsistente de condón em hombres que tienen sexo com hombres de Ciudad Juárez. Rev Salud pública. 2009; 11(5): 700-12. [ Links ]
Received: December 04, 2015; Accepted: May 14, 2016











 texto en
texto en 



