My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.16 n.46 Murcia Apr. 2017 Epub Apr 01, 2017
https://dx.doi.org/10.6018/eglobal.16.2.229371
Originales
Epidemiologic profile of acquired syphilis diagnosed and notified at a maternal-child university hospital
1Natal School of Nursing. Federal University of Rio Grande do Norte.
2Master in Nursing. Nurse of the Federal University of Rio Grande do Norte and the State Department of Health of Rio Grande do Norte.
3Graduate Program in Nursing. Federal University of Rio Grande do Norte. Brazil.
Method
There was an exploratory and descriptive study of quantitative approach, through secondary data collected in investigation forms / Women's syphilis notification assisted in Maternal-Child University Hospital, in Santa Cruz-RN in 2012. The study was approved by the Research Ethics Committee under report number 772.884.
Results
67% of mothers reported only attended elementary school, 33% are single, 42% undergone less, 58% of them held previous treatment of syphilis, but only 25% of partners joined and held it.
Conclusion
The study shows progress regarding diagnosis of syphilis during prenatal care, but it was pointed out the non-accomplishment of treatment of pregnant women before delivery, as well as of their partners. Therefore, innovative strategies are needed aiming for an early and proper treatment of pregnant women and their partners.
Keywords Syphilis; Women’s health; Treponemal infections; Maternal-child nursing
INTRODUCTION
Syphilis is an infectious disease caused by the bacterium Treponema pallidum. This infection occurs through sexual contact, blood transfusion, organ transplantation, or by congenital transmission. For compulsory notification, the Brazilian Ministry of Health (MoH) classifies it as: acquired syphilis, congenital syphilis (CS) and gestational syphilis, with CS being the most prominent for public health due to the high frequency with which it produces severe outcomes for the gestation and for the child; however, for its prevention it is necessary the early screening of acquired and/or gestational syphilis 1.
Official reports from the World Health Organization (WHO) indicate that about 12 million new cases occur annually in the adult population worldwide, mostly in developing countries. In Brazil, it is estimated that the average prevalence of acquired syphilis in pregnant women varies between 1.4% and 2.8%, with a vertical transmission rate around 25% 2.
In the State of Rio Grande do Norte, there were 399 cases of Acquired Syphilis reported from January 2011 to December 2012 (132 in 2011 and 267 in 2012), of which 56% occurred in women and 44% in men. It is also noted that in the period between 2007 and 2012, 1,309 cases of congenital syphilis were reported in that State, with a growing incidence rate 3.
CS was included in the list of compulsorily notifiable diseases in 1986, and this investigation form has changed over the years in the search for better detection and monitoring of the elimination process signed in international agreements by the Brazilian MoH. In this meantime, acquired syphilis gained this status only in 2005, through the MoH/SVS Ordinance No. 33, and the investigation form was released for typing in the National System of Notifiable Diseases (SINAN) in 2007 4.
With this in mind, the WHO recommends that the eradication of syphilis will contribute to three of the millennium's major goals: reducing child mortality, improving maternal health and combating HIV/AIDS, among other diseases 5.
In view of this proposition, the MoH recommends that during prenatal care every pregnant woman undergoes at least two VDRL tests, one at the time of the first visit and another around the 28th gestational week. A further VDRL test should be performed at the time of delivery to ensure the possibility of early treatment for the newborn if the pregnant woman has not been treated or has been re-infected after treatment. 6
Considering the existence of sensitive diagnostic tests, effective and low-cost treatment, syphilis is a sexually transmitted disease that can be easily controlled. Thus, the following guiding question emerged: what is the epidemiological profile of women diagnosed and reported with acquired syphilis in the puerperium?
Considering that the epidemiologic control of syphilis is one of the greatest challenges in public health in the country and in the world, this research aims to characterize the epidemiologic profile of women with acquired syphilis diagnosed and reported in the puerperium of a Maternal and Child University Hospital in the state of Rio Grande do Norte.
METHOD
The methodological support of this study used an exploratory, descriptive, quantitative, documentary and retrospective design on the epidemiologic characterization of congenital and acquired syphilis in the year 2012. The same was done at a University Hospital located in the city of Santa Cruz, in the Trairí Region of the state of Rio Grande do Norte (RN), Brazil. This service provides medium-complexity reference care to maternal and child health, operating in an area that includes the municipalities of the Trairí Region.
The study population consisted of all cases of syphilis among the patients who gave birth in this service in 2012, with notification/investigation forms completed, in the Epidemiological Surveillance Hospital Center (NHVE in Portuguese) of said hospital. Thus, 12 cases were notified in the studied year.
The data were obtained from September to October 2014, from the completed copies of Live Birth Records (LBRs) and the notification/investigation forms of acquired and congenital syphilis of puerperal women and newborns filed in the NHVE sector of the hospital. Researchers performed manual placement of the information recorded in the cited databases. Subsequently, they were organized in electronic database by means of spreadsheets in the Microsoft Excel application, in order to be categorized and classified according to each variable. Thus, the results were analyzed according to the descriptive statistics and they were presented in the form of tables.
The variables used were: age, schooling, race, municipality, area, occupation, marital status, parity, number of abortions, prenatal consultations, beginning of prenatal care, type of delivery, induction of delivery, professional who performed the delivery, knowledge of the diagnosis of syphilis, previous treatment of the pregnant woman, treatment of the partner, titration of the non-treponemic test, and clinical classification.
The access to the forms and medical records was consented by the leaders of the NHVE coordination and general administration. Throughout the process, the reliability of the information and anonymity of participants were respected, preserving the identity of the subjects surveyed and the institutional and ethical responsibility for the information provided.
In accordance with the requirements established by Resolution 466/12 of the Brazilian Health Council (CNS) that guides the practice of research with humans, the study was approved by the Research Ethics Committee (REC) of the Onofre Lopes University Hospital (HUOL), under opinion No. 772,884 and CAAE: 31591514.0.0000.5292.
RESULTS
Characterization of the study participants regarding socio-demographic aspects
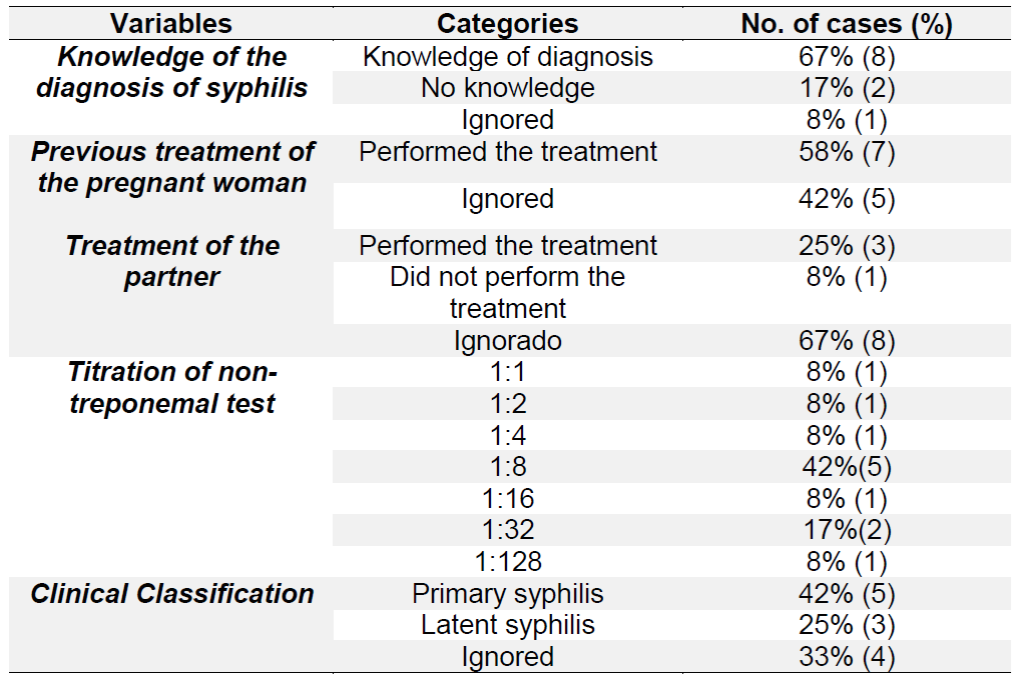
The women with acquired syphilis diagnosed and notified during the puerperium in a Maternal and Child University Hospital in the year 2012 constituted a population of 12 cases in their totality. The predominant age range varied between 19 and 23 years of age with six (50%) cases. As for race, ten (83%) women described themselves as browns. With regard to schooling, eight (67%) had attended only elementary school. According to the area of the municipality where they live, it was found that four (33%) lived in rural areas. Concerning the occupation, nine (75%) were farmers, and in relation to the marital situation, four (33%) were single (Table 1).
Table 1 Distribution of users according to sociodemographic variables, Santa Cruz, RN, Brazil, 2012
Source: research data.
The obstetric profile of study participants
Regarding parity, four (33%) women were in their second pregnancy. According to the number of abortions, one (8%) patient had two episodes of abortion. All patients had records of prenatal consultations, of which, five (42%) had the number of visits below the minimum recommended by the Ministry of Health (six consultations). With respect to the period when each one started prenatal care, nine (75%) started in the first trimester (Table 2).
Table 2 Characterization of the obstetric profile of women affected by syphilis, Santa Cruz, RN, Brazil, 2012

Source: research data.
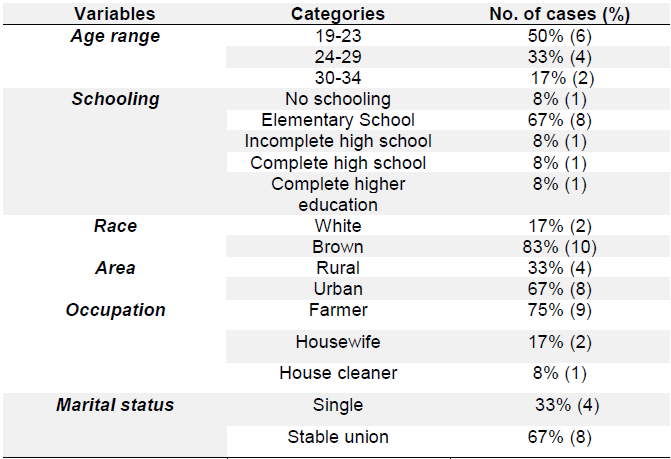
Regarding the history of syphilis, eight (67%) women reported being aware of the diagnosis of the disease. A total of seven (58%) patients had undergone previous treatment. Regarding the treatment of the partner, only three (25%) of the cases were treated. In all cases, the non-treponemal test had a reactive result, and in relation to the titration of this test, five (42%) cases presented a 1:8 infection result. According to the clinical classification of the disease, five (42%) cases were diagnosed as primary syphilis (Table 3).
DISCUSSION
This study showed that the profile of the puerperal women diagnosed and reported with acquired syphilis prevailed in the younger age group, with low level of schooling and predominant occupation of farmer. In addition, we observed in the study a relevant percentage of: single women, who did not perform treatment before delivery and untreated partners. These findings are confirmed by a study carried out in 2014, which points to the risk factors associated with syphilis infection: pregnancy in adolescence, absence of a fixed sexual partner and/or the existence of multiple partners, low educational level and socioeconomic level, multiparity, limited access to health services and presence of other sexually transmitted diseases (STDs) in the woman or in the partner6.
The number of abortions, as presented in Table 2, shows that exposure to syphilis has implications for the mother and her child, among them spontaneous abortion, since 16% of the interviewees reported having suffered interruption of previous pregnancies. Thus, studies indicate that women with syphilis, even after treatment, present a higher risk of adverse outcomes, such as prematurity, fetal and perinatal or neonatal death7)(8.
Thus, the results presented in Table 3 indicate that 67% of these women had the diagnosis of syphilis, 58% had undergone treatment prior to delivery, and only 25% of the partners had been treated. On the other hand, another study carried out in Brazil, with data from the Department of Informatics of the Unified Health System, in 2008, shows that only 24% had a diagnosis of syphilis before delivery and even the partner had been treated9. This shows advances in diagnosis during prenatal care; however, it is suggested that pregnant women have been re-infected by untreated partners, and that these treated partners have been re-infected through sexual contact with other infected and untreated women10)(11.
The resistance faced by health practitioners to perform the treatment of the sexual partner of patients with STIs is most often related to the historically excluding construction of public policies aimed at the men’s health, which causes a low demand for health services by the male audience. This fact may also be related to the role that has always been assigned to man as provider of the family, so they have been viewed as strong and unshakable beings, whereas the role of caring was always left to the woman. And yet, it is perceived the difficulty of the service itself to welcome this individual in his uniqueness12.
To detect the disease, non-treponemal tests are quantitative flocculation tests whose titration refers to the disease activity and they are used to monitor treatment. The VDRL (Venereal Disease Research Laboratory) is the most commonly used test because it has good sensitivity and specificity, and can remain reagent even after healing the infection (serological scar), but with progressive decline in titrations 6)(13)(14.
Regarding the treatment, in order for the pregnant woman with syphilis to be considered adequately treated, excluding the possibility of infection of the child, she must be medicated with penicillin G benzathine at the appropriate doses for the stage of infection, have finished the treatment at least 30 days before the birth, and her partner must have been concomitantly treated with the same therapeutic regimen as hers. Even if the woman is treated properly, the non-treatment of the partner implies a high risk of re-infection of the pregnant woman, consequently increasing the probability of vertical transmission of the disease 15.
Thus, a higher prevalence of syphilis in women of low socioeconomic status, with a risk obstetric history and with difficulty accessing health services indicates the greater social and reproductive vulnerability of these women, which makes the control of syphilis more complex in this population 16)(17.
Thus, in order to emphasize the control of this disease, there is need of a quality prenatal care, with wide coverage and innovative strategies for the early identification of pregnant women; assurance of the diagnosis of the disease during pregnancy and in the shortest possible time, allowing the women to be treated before the 24th to the 28th gestational week, which is the most effective period for the fetus; appropriate clinical management of the pregnant woman and her partner (s), including advice on the disease and forms of prevention. Thus, there may be increased adherence to treatment and reduction of the vulnerability of women and their partners to STDs16)(18)(19.
However, despite the increasing number of prenatal visits carried out over the years, the incidence of syphilis has also increased. These data may reveal both the quality of the prenatal care, which remains below the desired level, and increase in reported cases, which, even though it is still lower than expected, has been showing advances20, as evidenced in Table 1, which revealed that 75% of women started prenatal care in the first trimester of pregnancy and 58% attended more than 6 visits.
The importance of reporting in SINAN as one of the means of controlling acquired and congenital syphilis is emphasized, since, by collecting, transmitting and disseminating data on the obligatory reporting diseases, SINAN becomes a relevant instrument in the setting of priorities for intervention and allows the impact of these diseases to be evaluated.
CONCLUSION
The study of the profile of women with acquired syphilis was characterized by a low level of schooling, a significant percentage of single pregnant women, advances in the early beginning of prenatal care, number of visits and diagnosis during pregnancy. However, it was emphasized that pregnant women have not performed treatment before delivery, nor their partners have been treated.
Thus, the increase in the incidence of congenital and acquired syphilis in the gestational period and the consequent increase in its cases can only be minimized and controlled when the prevention and control measures are satisfactorily applied. To this end, it is necessary that both health practitioners and managers are committed to the quality of services provided in prenatal care with a view to screening through VDRL, early and appropriate treatment of pregnant women and their partner (s).
Finally, it is considered as limitation of the study the amount of data ignored in the notification forms. Thus, the importance of the quality of records related to the follow-up of pregnant women is emphasized, with the purpose of improving the prenatal care of the triad mother-family-baby. In addition, we suggest new studies with primary data that complement this information, with a view to improving health care for women and controlling this disease.
REFERENCIAS
1. Brasil. Ministério da Saúde. Diretrizes de Controle da Sífilis Congênita. Brasília (MS): 2005, p.7-53. [ Links ]
2. Holanda MTCG, Barreto MA, Machado KMM, Pereira RC. Perfil Epidemiológico da Sífilis congênita no Município do Natal, Rio Grande do Norte - 2004 a 2007. Epidemiol. Serv. Saúde. 2011;20(2):203-12. [ Links ]
3. Boletim Epidemiológico - DST/Aids e Hepatites Virais. Governo do Estado do Rio Grande do Norte. Secretaria de Estado da Saúde Pública - SESAP. Coordenadoria de Promoção a Saúde. Programa Estadual DST/AIDS e Hepatites Virais, 2012. [ Links ]
4. Saracemi V, Miranda AE. Relação entre a cobertura da Estratégia Saúde da Família e o diagnóstico de sífilis na gestaçãoe sífilis congênita. Cad. Saúde Pública. 2012; 28(3):490-6. [ Links ]
5. Silva MRF, Brito ESV, Freire LCG, Pedrosa MM, Sales VMB, Lages I. Percepção de mulheres em relação a ocorrência de sífilis congênita em seus conceptos. Rev. APS. 2010;13(3):301-9. [ Links ]
6. Damasceno ABA, Monteiro DLM, Rodrigues LB, Barmpas DBS, Cerqueira LRP, Trajano AJB. Sífilis na gravidez. Revista hupe. 2014;13(3):89-95. [ Links ]
7. Mesquita KO, Lima GK, Filgueira AA, Flôr SM, Freitas CASL, et al. Análise dos Casos de Sífilis Congênita em Sobral, Ceará: Contribuições para Assistência Pré-Natal. DST-J Bras Doenças Sex Transm. 2012;24(1),20-7. [ Links ]
8. Qin JB, Yang TJ, Hong FC, Lan-Lan LN, Zhang CL, Yang F, Mamady K, Dong W. Risk Factors for Congenital Syphilis and Adverse Pregnancy Outcomes in Offspring of Women With Syphilis in Shenzhen, China: A Prospective Nested Case-Control Study. Rev. Sexually Transmitted Diseases. 2014;41(1):13-23. [ Links ]
9. Araújo CL, Shimizu HE, Souza AIA, Hamann EM. Incidência da sífilis congênita no Brasil e sua relação com a Estratégia Saúde da Família. Rev. Saúde Pública. 2012; 46(3):479-86. [ Links ]
10. Magalhães DMS, Kawaguchi IAL, Dias A, CAlderon IMPL. Sífilies materna e congênita: ainda um desafio. Cad. Saúde pública. 2013; 29(6):1109-20. [ Links ]
11. Brasil, Ministério da Saúde. Secretaria de Vigilância em Saúde. Boletim Epidemiológico - AIDS e DST. Brasília (MS): 2012. [ Links ]
12. Campos ALA, Araújo MAL, Melo SP, Andrade RFV, Gonçalves MLC. Sífilis em parturientes: aspectos relacionados ao parceiro sexual. Rev. Bras. Ginecol. Obstet. [online]. 2012;34(9):397-402. [ Links ]
13. Wokowski KA, Berman SM. Diasese Control and Prevention. Sexually transmitted diseases treatment guidelines. 2010. MMWR Recom Rep. 2011. 60(1):18. [ Links ]
14. Oliveira FS, da Costa CFC, Kerber NPC, Barros AM, Wachholz VA, Lemos DB. A utilização do preservativo feminino pelas profissionais do sexo. Enfermería Global. 2012, (26): 399. [ Links ]
15. Campos ALA, Araújo MAL, Melo SP, Gonçalves MLC. Epidemiologia da sífilis gestacional em Fortaleza, Ceará, Brasil: agravos sem controle. Cad. Saúde Pública 2010;26(9):1747-55. [ Links ]
16. Domingues RMSM, Saracen V, Hartz ZMA, Leal MC. Sífilis Congênita: evento sentinela da qualidade da assistência pré-natal. Rev. Saúde Pública [Internet] 2013; 47(1):147-57. [ Links ]
17. Nascimento MI, Cunha AA, Guimarães EV, Alvarez FS, Oliveira SRSM, Bôas EV. Gestações complicadas por sífilis materna e óbito fetal. Rev. bras. ginecol. obstet. 2012;34(2):56-62. [ Links ]
18. Muricy CL, Junior VLP. Congenital and Maternal syphilis in the capital of Brazil. Rev. da Sociedade Brasileira de Medicina Tropical. 2015;48(2):216-9. [ Links ]
19. Parker LA, Deschutter, Bornay-Llinares, Hernandez-Aguado I, Silva G, Pirangine CR, L B. Clinical and socioeconomic determinants of congenital syphilis in Posadas, Argentina. Internacional Journal of Infectious Diseases, 2012;16:256-61. [ Links ]
20. Costa CC, Freitas LV, Sousa DMN, Oliveira LL, Chagas ACMA, Lopes MVO, et. al. Sífilis congênita no Ceará: análise epidemiológica de uma década. Rev. Esc. Enferm USP. 2013;47(1):152-9. [ Links ]
Received: June 18, 2015; Accepted: September 21, 2015











 text in
text in