Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.17 no.50 Murcia abr. 2018 Epub 14-Dic-2020
https://dx.doi.org/10.6018/eglobal.17.2.275881
Originals
Risk factors associated to vaginal infections and squamous intraepithelial lesions in university students in Medellín, Colombia
1 Bacteriólogo, especialista en Biotecnología, docente Tecnológico de Antioquia Institución Universitaria, Grupo de Investigación BISMA TdeA, Docente Instituto Tecnológico Metropolitano. Colombia.
1 Bacteriólogo, especialista en Biotecnología, docente Tecnológico de Antioquia Institución Universitaria, Grupo de Investigación BISMA TdeA, Docente Instituto Tecnológico Metropolitano. Colombia.
2 Médico, Residente de Ginecología y Obstetricia Universidad Pontificia Bolivariana.Colombia.
3 Enfermero, Magíster en Epidemiología, Candidato a PhD en Salud Pública. Docente Titular Uniiversidad Pontificia Bolivariana.Colombia.
4 Citohistotecnólogo, Bacteriólogo, Docente Tecnológico de Antioquia Institución Universitaria. IPS Universitaria Universidad de Antioquia. Colombia. Colombia.
41 Citohistotecnólogo, Bacteriólogo, Docente Tecnológico de Antioquia Institución Universitaria. IPS Universitaria Universidad de Antioquia. Colombia.
5 Enfermera, Especialista en Gerencia de la Calidad y Auditoría en Servicios de Salud. Docente Universidad Pontificia Bolivariana. Colombia..
Objective
To explore the risk factors associated with vaginal infections and squamous intraepithelial lesions of the cervix in university students in Medellín, Colombia.
Materials and methods
Cross-sectional study; a convenience sample of 176 students from the health care field were included. Data were obtained through an anonymous survey that included demographic, clinical, and academic variables, as well as those pertaining to sexual habits. Cervical cytology and direct gram stain of vaginal fluid were taken. The statistical association for vaginal infections and squamous intraepithelial lesions of the cervix was explored through the odds ratio and the 95% confidence intervals (95% CI). A p value <0.05 was considered statistically significant.
Results
Atypical squamous cells of undetermined significance (ASCUS) was found in 9.1% of participants; low-grade cervical squamous intraepithelial lesions in 4.5%, and vaginal infections in 30.7%; bacterial vaginosis was the most common infection. Previous history of HPV has a statistical association with ASCUS OR = 36.69 95% CI (3.56-378.15) and vaginosis by Gardnerella OR = 10.57 CI 95% (1.07-104.64), whereas urinary infections had a statistical association for candidiasis OR = 4.46 CI 95% (1.21-16.5).
Conclusions
Our findings can be used as descriptive information regarding the frequency of vaginal infections and squamous intraepithelial lesions of the cervix in university populations, to continue or improve programs for the promotion and prevention of sexual and reproductive health in young populations.
Keywords Human papillomavirus; Trichomonas Vaginitis; Candidiasis, Vulvovaginal; Gardnerella vaginalis; Squamous Intraepithelial Lesions of the Cervix
INTRODUCTION
Vaginal infections (VI) are an alteration of the condition of the female genital system, which are multifactorial in origin and are clinically characterized by changes in amount of vaginal discharge, odor changes, irritation, and itching 1 2 3-4. Alterations of the normal vaginal condition are favored by various factors including poor genital-anal hygiene, new or multiple sexual partners (regardless of the frequency of sexual intercourse), bathing in swimming pools or bathtubs, pregnancy, diabetes, parasitosis, urinary or fecal incontinence, stress, congenital malformations of the genital tract, frequent use of antibiotics, hormones, use of oral topical contraceptive preparations, vaginal medications, immunological deficiency, wearing tight clothing, smoking, presence of herpes simplex virus 2 (HSV2) antibodies, and changes in the normal microbial flora such as a loss of production of H2O2 by lactobacilli 5 6 7 8 9-10.
Vaginal infections affect 20-62% of women of reproductive age 11 12-13 and approximately 20% are the result of alterations caused by medications such as antibiotics 14 or the use of birth control methods 15. Between 24% and 37% of VIs are sexually transmitted, and 21.5-54.4% 16 affect pregnant women 17 18 19-20.
The frequency of vaginal infections by Candida sp. in university students varies between 20% and 45% according to international reports 11,14. In Colombia, publications on these types of studies are scarce as studies have only been conducted in prison populations 21, sex workers 13 and women who seek medical attention due to alterations in vaginal discharge. Findings show that 90% of infections are bacterial in origin, while the rest are fungal or protozoan 22.
The literature reports that the frequency of human papillomavirus (HPV) infection is high in young women. Up to 50% of adolescent women and young adults get HPV infection within the first 4-5 years of being sexually active, of whom 25% develop low-grade squamous epithelial lesions. However, 90-95% of these infections in young women heal on their own 23.
The aim of this study was to explore some of the risk factors associated with vaginal infections and squamous intraepithelial lesions (SIL) of the cervix in university students in Medellín, Colombia.
Study Design and Population
A cross-sectional, analytical, observational study was conducted using a convenience sample of 176 students from the health care field aged 18 or older at a university in Medellín who voluntarily participated in the study to undergo a vaginal cytology and direct gram stain of vaginal fluids. The exclusion criteria considered included those who had sexual intercourse or who used a vaginal douche 48 hours prior to the cytology and direct gram stain, those who had menstrual bleeding at the time of the test, those who had never had intercourse, pregnant women, those not covered by the Colombian health system, those who could not undergo the tests based on the main researcher’s criteria, and those who refused to sign the informed consent.
Data Collection
An anonymous survey was used, which included demographic and academic variables (age, socioeconomic strata, marital status, and current semester), clinical variables (gynecologic history and pathology, use of contraceptives, frequent use of vaginal douche), as well as variables related to sexual habits such as the use of condoms, frequency of intercourse, and number of sexual partners over the past semester. Thereafter, samples were taken from the students using uterine cervical cytology and direct gram stain of vaginal fluids by students from the histo-cytotechnology program in their last semester at Institución Universitaria Tecnológico de Antioquia, who had been trained and were supervised by professional personnel. All samples were read by bacteriologists and histo-cytotechnologists, and 10% of the samples that were positive for SIL were sent in to be reviewed by a pathologist.
Statistical Analysis
The information was processed and analyzed using SPSS® version 17.0 (SPSS Inc; Chicago, Illinois, USA); under Universidad Pontificia Bolivariana (UPB) license. Quantitative and qualitative variables were described for the statistical analysis. The variables measured at nominal level were described with absolute and relative frequency measures; variables were expressed by means of their maximum, minimum, and median values and interquartile range (IQR) due to the fact that the Kolmogorov-Smirnov test resulted in a non-normal distribution, yielding a p value<0.0001.
The statistical association of the presence of VI or SIL with variables of interest through the odds ratio (OR) and its 95% confidence interval (CI95%) was explored. A p value <0.05 was considered statistically significant.
Ethical Issues
Students were asked to sign the informed consent prior to their participation in the study. Fundamental ethical principles were upheld, information was handled with absolute confidentiality, and the study was approved by the Research Ethics Committee.
The students having positive results for VI and/or SIL on the lab tests were referred to their respective healthcare providers.
Sociodemographic and Academic Characteristics
The median age of students was 20 years, with IQR (19-24); 91.9% came from low socioeconomic strata (strata one, two or three); 146 students (83.0%) were single at the time of the survey, 17 were in a common law marriage (9.7%), and 10 were married (5/5%); 72.4% were in one of their first four semesters.
The use of vaginal douches was found to be uncommon in those surveyed as only 35 women (19.9%) said they had used them at least once in their lifetime; of these, six (3.4%) had used them in the month prior to being surveyed, and four (2.3%) in the week prior. Regarding contraceptive use, 109 students (61.9%) had used them in the last six months; 29.5% used oral contraceptives, which was the most common method, followed by injectable contraceptives, used by 25%. Of all students surveyed, 125 (71.0%) reported having an active sexual partner; the median age at which they became sexually active was 17, with IQR (15-18), and less than half of the sample (45.5%) regularly used condoms. The frequency of sexual intercourse with penetration is presented on graph 1.
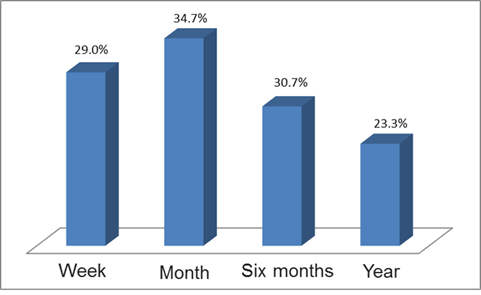
Graph 1 Frequency of sexual intercourse with penetration over the last week, the last month, the last six months, and the last year.
Regarding gynecologic histories, 33 students (18.8%) had been pregnant at least once, of whom 14 (42.4%) aborted; five admitted to having had sexually transmitted infections, four of which were by human papillomavirus (HPV) and one by trichomoniasis. Twenty-six women said to have had vaginal infections over the month previous to data collection, which represents 14.8%, while 13 (7.4%) reported having urinary infections.
Signs and symptoms observed in exams
With respect to the symptoms described by study participants during the tests, 24 (13.6%) had itching, four (2.3%) dyspareunia, and two (1.1%) pelvic pain.
The macroscopic examination revealed 24 women with cervical erosion (13.6%); the same percentage had clumpy discharge, while three (1.7%) had mucopurulent discharge, and one had brown discharge. Thirty-four women (19.3%) had cervical ectropion, and eight (4.5%) had cervical congestion. Cysts were found in three patients and condyloma in two.
Vaginal Infections and Squamous Intraepithelial Lesions
Upon conducting the direct gram stain, 54 positive results (30.7%) were obtained for vaginal infections, of which 34 (63.0%) corresponded to bacterial vaginosis, while 20 (37.0%) were positive for vaginitis by Candida sp.
Atypical squamous cells of undetermined significance (ASCUS) were found in 16 students (9.1%), low-grade squamous intraepithelial lesions (LSIL) in eight (4.5%), LSIL by HPV in two, and high-grade SIL (HSIL) and ASC-H in only one student. None were found to have adenocarcinomas.
Factors Associated with VI or SIL
When exploring the statistical association between the variables of interest and the presence of VI or SIL in the exams conducted, it was found that being under age 30 was a protective factor for low-grade SIL (OR=0.13; CI 95%=0.02-0.76). An HPV background was a risk factor for ASCUS (OR=36.69; CI 95%=3.56-378.15) and for vaginosis by Gardnerella (OR=10.57; CI 95%=1.07-104.64), while urinary infections were a risk factor for candidiasis OR=4.46; CI 95%=1.21-16.5).
DISCUSSION
In this study it was observed that over half of the participants do not frequently use condoms as a method of avoiding sexually transmitted infections, which is consistent with the literature. For example, it was reported that 23% of participants in a study conducted in Medellín with a comparable population stated they never used condoms during sexual intercourse 24. There were similar observations in Iztacala, México where 45% of university students surveyed expressed they did not always use condoms during intercourse 25; similarly, a study conducted in Asturias, Spain revealed that 34% of university students did not use condoms 26.
Regarding the number of sexual partners, data obtained are similar to those found in a university population in Bogotá which reported that 61.8% of participants mentioned only having one partner 27; a similar figure was reported by Universidad del Rosario de Colombia in 2005, where 74% of participants stated they had had fewer than three sexual partners since they had been sexually active 28. These similarities are probably related to cultural aspects and could be associated to the average age at which women become sexually active in Colombia.
With respect to the use of contraceptives, it was observed that 61.9% of students had used them within the six previous months. This percentage is lower than data collected in other studies in Colombia with similar populations, such as 82% 27 and 88% 28 in university students in Bogotá. This study revealed that the use of oral contraceptives was the most common at 29.5%, followed by injectable contraceptives used by 25%. These figures are similar to what was reported in a study conducted at a university in Bogotá in 2010 27, but differ from another study in the same city in 2006 which reported that 44.8% of university students surveyed used anovulatory oral contraceptives, 18.8% used injectable contraceptives, and 31.4% used condoms 29. Such differences could be explained by the fact that oral contraceptives are Colombian women’s preferred self-administered hormonal contraceptive mainly due to the lack of medical advice and the fact that they are sold as over-the-counter drugs 30 31-32.
Concerning gynecologic history, 18.8% of the population had been pregnant at least once, of whom 42.4% aborted. This differs from what was reported in a study conducted at Universidad Industrial de Santander where only 8% of surveyed students had ever been pregnant 33. This difference is due to the fact that the number of pregnant teenagers between 2005 and 2010 in the department of Antioquia was greater than in Santander. Thus, the results of this study are similar to data obtained in Antioquia (19.8%) and are near the national percentage (19.5%) 34.
Of the cytologies conducted, 13.6% yielded results with abnormalities. These findings are consistent with those obtained in a group of university students in Popayan where there was a 10% prevalence of cytologic alterations 21, but they differ from what was reported in a study from Universidad Industrial de Santander where 33% of exam results were abnormal 33. This could be associated to the different sampling techniques used as well as the characteristics such as age, biological variables, and demographic conditions of the participants in both studies.
The most common vaginal infection was bacterial vaginosis, found in 29.5% of students, while 11.4% were positive for vaginitis by Candida sp.; these results are consistent with what has been reported in the scientific literature 17,22,35. With respect to ASCUS, the data found are similar to those reported by Bravo 5% 21, Mount 9.7% 36, and Mangan 4.1% 37. However, there is consensus that the prevalence of ASCUS and low-grade lesions in adolescents and young women is significantly high and that most are related to infection by HPV 38.
Findings related to SIL present low prevalence in this type of population, which is similar to what has been reported in the literature and can be explained due to the protective factor associated to age found in the present study, which is similar to what has been reported in the literature 2,9,23,26,33 34 35 36-37.
Studies conducted in university populations in Latin America show that students lack knowledge regarding sexually transmitted infections. For example, a study conducted at a university in Medellín found that 69.9% of those surveyed were unaware of how HPV is acquired or transmitted, and 84.9% did not know which diseases are caused by this virus 24. Another study carried out in Mexico found that 63% of those surveyed were unaware of the clinical manifestations of sexually transmitted infections and HPV 41.
Although this study did not explore students' knowledge regarding sexually transmitted infections, the study of the prevalence of vaginal infections and infections by HPV is important in this type of population. The correlation with the knowledge regarding these infections and their prevention should also be studied with the aim of establishing promotion and prevention measures with respect to these manifestations. According to the literature, this lack of knowledge puts these types of populations at risk of acquiring infections making it necessary to improve sex education in the university setting and heighten awareness regarding the repercussions of such infections.
The authors consider it imperative for there to be intervention, control, and knowledge of the frequency of vaginal infections in this population since it was found that the average age to become sexually active in women is 17 years. These data are consistent with that which has been reported in other studies 23 24 25-26 and correspond to the average age students enter college in Colombia 42, which is why addressing this population in an adequate and opportune manner by offering topics related to sex education could positively impact the prevention of such infections.
Limitations
Due to the fact that a convenience sample was used and since it cannot be guaranteed that the risk factors preceded the event because of the temporality of the study, inferences cannot be made. Therefore, findings regarding risk or protective factors must be interpreted as statistical associations but not as causal associations.
CONCLUSIONS AND RECOMMENDATIONS
The abnormalities in the results of the vaginal discharge and cytology tests are mainly associated to microorganisms and the presence of squamous cell abnormalities. These findings can be used as descriptive information regarding the frequency of VI and SIL in university populations to conduct follow-up studies that may allow to implement, continue, or improve programs for sexual and reproductive health, prevention, detection, and treatment of uterine cervical diseases in young populations.
Since uterine cervical cytology is a screening test, further studies are warranted in which other diagnostic tests are conducted to evaluate the specificity of such tests for the detection of cancer and which allow to associate other factors with this event.
REFERENCIAS
1. Zhou X, Westman R, Hickey R, Hansmann MA, Kennedy C, Osborn TW, et al. Vaginal microbiota of women with frequent vulvovaginal candidiasis. Infect Immun. 2009;77(9):4130-5. [ Links ]
2. Klebanoff MA, Hillier SL, Nugent RP, MacPherson CA, Hauth JC, Carey JC, et al. Is bacterial vaginosis a stronger risk factor for preterm birth when it is diagnosed earlier in gestation? Am J Obstet Gynecol. 2005;192(2):470-7. [ Links ]
3. González C, Moreno MA, Nieves B, Flores A, Chille A, Carrero S, et al. Flora vaginal en pacientes que asisten a consulta ginecológica. Rev Soc Venez Microbiol. 2006;26(1):19-26. [ Links ]
4. Mandell G, Bennett J, Dolin R. Enfermedades infecciosas: principios y práctica. 7.a ed. Madrid: Elsevier; 2012. [ Links ]
5. Eckert LO. Acute vulvovaginitis. N Engl J Med. 2006;355(12):1244-52. [ Links ]
6. Fethers KA, Fairley CK, Hocking JS, Gurrin LC, Bradshaw CS. Sexual risk factors and bacterial vaginosis: a systematic review and meta-analysis. Clin Infect Dis. 2008;47(11):1426-35. [ Links ]
7. Joesoef MR, Schmid GP. Bacterial vaginosis. Clin Evid [Internet]. 2005 [citado 3 de septiembre de 2016];2005;4:1601. Disponible en: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907556/ [ Links ]
8. Cherpes TL, Hillier SL, Meyn LA, Busch JL, Krohn MA. A delicate balance: risk factors for acquisition of bacterial vaginosis include sexual activity, absence of hydrogen peroxide-producing lactobacilli, black race, and positive herpes simplex virus type 2 serology. Sex Transm Dis. 2008;35(1):78-83. [ Links ]
9. Chiaffarino F, Parazzini F, De Besi P, Lavezzari M. Risk factors for bacterial vaginosis. Eur J Obstet Gynecol Reprod Biol. 2004;117(2):222-6. [ Links ]
10. Novak RM, Donoval BA, Graham PJ, Boksa LA, Spear G, Hershow RC, et al. Cervicovaginal levels of lactoferrin, secretory leukocyte protease inhibitor, and RANTES and the effects of coexisting vaginoses in human immunodeficiency virus (HIV)-seronegative women with a high risk of heterosexual acquisition of HIV infection. Clin Vaccine Immunol. 2007;14(9):1102-7. [ Links ]
11. Di Bartolomeo S, Rodriguez Fermepin M, Sauka DH, Torres RA de. Prevalencia de microorganismos asociados a secreción genital femenina, Argentina. Rev Saúde Pública. 2002;36(5):545-52. [ Links ]
12. Flores-Paz R, Rivera-Sánchez R, García-Jíménez E, Arriaga-Alba M. Etiología de la infección cérvico vaginal en pacientes del Hospital Juárez de México. Salud Pública México. 2003;45: S694-7. [ Links ]
13. Mondeja A, Diana L, Almanza Martínez C, Fernández Limia O. Diagnóstico y prevalencia de infecciones vaginales. Rev Cuba Obstet Ginecol. 2010;36(2):62-103. [ Links ]
14. Azzam-W M, Cermeño-Vivas JR, Orellán-García Y, Penna-V SJ. Vulvovaginitis por Candida spp. y Trichomonas Vaginalis en Mujeres Sexualmente Activas. Investig Clínica. 2002;43(1):03-13. [ Links ]
15. Restrepo A, Díaz F, Estrada S, Franco L, Jaramillo J, Maestre A, et al. Microbiología de las infecciones humanas [Internet]. 1.a ed. Medellín: CIB; 2007 [citado 3 de septiembre de 2016]. Disponible en: http://www.fondoeditorialcib.com/producto/microbiologia-de-las-infecciones-humanas/ [ Links ]
16. Vázquez J, Ortiz C, Ley M, Pérez J, Calero J. Prevalencia de infecciones cervico-vaginales en embarazadas en un hospital obstétrico de referencia de Ciudad de la Habana. Rev Cubana Obstet Ginecol. 2007;33(2). [ Links ]
17. Medina R, Rechkemmer A, Garcia-Hjarles M. Prevalencia de vaginitis y vaginosis bacteriana en pacientes con flujo vaginal anormal en el Hospital Nacional Arzobispo Loayza. Rev Medica Hered. 1999;10(4):144-50. [ Links ]
18. Aroutcheva A, Ling Z, Faro S. Prevotella bivia as a source of lipopolysaccharide in the vagina. Anaerobe. 2008;14(5):256-60. [ Links ]
19. Coppolillo E, Vay C, Menghi C, Cora M, Gatta C, de Torres R, et al. Prevalencia de infecciones vaginales en embarazadas sintomáticas y asintomáticas. Enfermedades del Tracto Genital Inferior. 2007;1(1):17-22. [ Links ]
20. González Melián D, Blanco Miclín N, Lucas Macías F, La Rosa Kindelán E. Principales causas de infecciones vaginales en gestantes ingresadas en el hospital "reynaldo chiang vargas" durante enero - abril del 2001. MEDISAN. 2002;6(3):44-48. [ Links ]
21. Bravo de Insuasty M, Erazo JV, Álvarez AM, Casas MI, Ortiz de Collazos O, Álvarez-Soler J. Prevalencia De Anormalidades En La Citología Cervical En Tres Grupos Poblacionales De Mujeres En Popayán, Colombia 2003 - 2005. Rev Colomb Obstet Ginecol [Internet]. 2008 [citado 18 de junio de 2016];59(3). Disponible en: http://www.redalyc.org/resumen.oa?id=195214332003 [ Links ]
22. Salas N, Ramírez JF, Ruiz B, Torres E, Jaramillo LN, Gómez-Marín JE. Prevalencia de microorganismos asociados a infecciones vaginales en 230 mujeres gestantes y no gestantes sintomáticas del Centro de Salud La Milagrosa en el municipio de Armenia (Colombia). Rev Colomb Obstet Ginecol. 2009;60(2):135-42. [ Links ]
23. Herrero R, Castle PE, Schiffman M, Bratti MC, Hildesheim A, Morales J, et al. Epidemiologic profile of type-specific human papillomavirus infection and cervical neoplasia in Guanacaste, Costa Rica. J Infect Dis. 2005;191(11):1796-807. [ Links ]
24. Gaviria ÁM. Conocimientos de los estudiantes universitarios del Colegio Mayor de Antioquia, Medellín, acerca del Papilomavirus humano. Revista Facultad Nacional de Salud Pública. 2003;21(2):43-48. [ Links ]
25. Hurtado de Mendoza Zabalgoitia MT, Olvera Méndez J. Infecciones de transmisión sexual en la población femenina de estudiantes universitarias. Rev Electrónica Psicol Iztacala [Internet]. 2012 [citado 18 de junio de 2016];15(3). Disponible en: http://revistas.unam.mx/index.php/repi/article/view/33734 [ Links ]
26. Anton Fernández R. Conocimientos y conductas frente al virus del papiloma humano y cáncer de cérvix en mujeres universitarias del Principado de Asturias. Oviedo: Universidad de Oviedo; 2015 [citado 18 de junio de 2016]; Disponible en: http://digibuo.uniovi.es/dspace/handle/10651/31563 [ Links ]
27. Acosta S, Ibáñez E, Alfonso A, Cifuentes L, Gamba S, Mojica C, et al. Conductas de salud y factores de riesgo en la salud sexual y reproductiva de una población universitaria. NOVA [Internet]. 2010 [citado 18 de junio de 2016];8(13): 30-41. Disponible en: http://unicolmayor.edu.co/publicaciones/index.php/nova/article/view/148 [ Links ]
28. Ruiz Sternberg AM, Latorre Santos C, Beltrán Rodríguez J, Ruiz Sternberg J, Vélez Van Meerbeke A. Conocimientos, actitudes y prácticas en salud sexual y reproductiva en una población universitaria. Rev Soc Chil Obstet Ginecol Infant Adolesc. 2005;12(3):86-93. [ Links ]
29. Arteaga Correa M, Daza Arias M, Gomez Robles N, Raga Ruiz N. Asociación entre conocimiento y uso de métodos anticonceptivos en estudiantes de enfermería y medicina de la Universidad El Bosque. Rev Colomb Enferm. 2006;1(1):65-73. [ Links ]
30. Carvajal O. Cucuteñas prefieren la inyección y la píldora para planificar. La Opinión [Internet]. 2015 [citado 18 de junio de 2016]. Disponible en: http://www.laopinion.com.co/cucuta/cucutenas-prefieren-la-inyeccion-y-la-pildora-para-planificar-102751#ATHS [ Links ]
31. Colombia, en la era de los inyectables. El Tiempo [Internet]. 1997 [citado 18 de junio de 2016]. Disponible en: http://www.eltiempo.com/archivo/documento/MAM-615862 [ Links ]
32. Gómez P, Lozano F, Velásquez Á, Marrugo M, Torres L. Impacto de la asesoría sobre anticoncepción en la selección de métodos hormonales combinados en Colombia. Rev Panam Salud Publica. 2015;37(6):395-401. [ Links ]
33. García Rueda A, Fajardo Peña MT, Caballero Badillo MC, Camargo-Figuera FA. Resultados de la citología cervicovaginal en población universitaria. Un estudio descriptivo. Enferm Glob. 2016;15(2):1. [ Links ]
34. Colombia. Consejería Presidencial para la Primera Infancia. El aumento del embarazo de adolescentes en Colombia [Internet]. Bogotá: De Cero a Siempre; 2013 [citado 18 de junio de 2016]. Disponible en: http://www.deceroasiempre.gov.co/Prensa/CDocumentacionDocs/Bolet%C3%ADn%20No.%202%20El%20aumento%20de%20embarazos%20adolescentes%20en%20Colombia.pdf [ Links ]
35. Martínez M, Barría PA, Meneses R, Oyarzún P, Sandoval J. Vulvovaginitis en la adolescencia: estudio etiologico. Rev Chil Obstet Ginecol. 2003;68(6):499-502. [ Links ]
36. Mount SL, Papillo JL. A Study of 10 296 Pediatric and adolescent papanicolaou smear diagnoses in northern New England. Pediatrics. 1999;103(3):539-45. [ Links ]
37. Mangan SA, Legano LA, Rosen CM, McHugh MT, Fierman AH, Dreyer BP, et al. Increased prevalence of abnormal Papanicolaou smears in urban adolescents. Arch Pediatr Adolesc Med. 1997;151(5):481-4. [ Links ]
38. Richardson H, Kelsall G, Tellier P, Voyer H, Abrahamowicz M, Ferenczy A, et al. The natural history of type-specific human papillomavirus infections in female university students. Cancer Epidemiol Biomark Prev. 2003;12(6):485-90. [ Links ]
39. Bravo MM, Medina O, Melgarejo D, Serrano M. Infección por virus del papiloma humano en una muestra de mujeres jóvenes con citología normal. Rev Colomb Cancerol. 8(2):5-10. [ Links ]
40. de Sanjosé S, Diaz M, Castellsagué X, Clifford G, Bruni L, Muñoz N, et al. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis. Lancet Infect Dis. 2007;7(7):453-9. [ Links ]
41. Bustamante-Ramos GM, Martínez-Sánchez A, Tenahua-Quitl I, Jiménez C, López-Mendoza Y. Conocimiento y prácticas de prevención sobre el virus del papiloma humano (VPH) en universitarios de la Sierra Sur, Oaxaca. An Fac Med. 2015;76(4):369-76. [ Links ]
42. Colombia. Ministerio de Educación. Análisis de determinantes de la deserción en la educación Superior Colombiana con base en el SPADIES. Bogotá: Ministerio de Educación; 2008. [ Links ]
Received: November 23, 2016; Accepted: April 07, 2017











 texto en
texto en 


