My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.17 n.51 Murcia Jul. 2018 Epub Apr 01, 2018
https://dx.doi.org/10.6018/eglobal.17.3.292821
Originals
Pelvic floor dysfunctions in primiparous women after birth
1Profesora Asociada. Departamento de Enfermería Materno-Infantil y Psiquiátrica, Escuela de Enfermería, Universidad de São Paulo, São Paulo, SP, Brasil. soniaju@usp.br
2 Profesora Doctora. Curso de Obstetricia, Escuela de Artes, Ciencias y Humanidades, Universidad de São Paulo, São Paulo, SP, Brasil.
3Máster en Ciencias, Escuela de Enfermería, Universidad de São Paulo. Enfermera Obstétrica, Hospital Santa Bárbara, Santa Bárbara d'Oeste, São Paulo. Brasil.
4 Enfermera Obstétrica. Alumna de Máster del Programa Pos-Graduación en Enfermería de la Escuela de Enfermería de la Universidad de São Paulo, SP, Brasil.
5 Enfermera Obstétrica. Residente del Programa de Residencia en Enfermería Obstétrica de la Escuela de Enfermería, Universidad de São Paulo, SP, Brasil.
Objective
To assess the prevalence of the urinary tract infection (UTI), urinary incontinence (UI), anal incontinence (AI) and dyspareunia among primiparous women, as well as to identify the association between dyspareunia and UI and mode of birth.
Material and methods
Prospective observational study carried out with 96 post-partum women (72 normal births and 24 caesarean section), two and six months after birth. Data were collected via prenatal cards, medical registers and interviews with women between January and August, 2014, at the Centro do Parto Normal do Pronto Socorro e Maternidade Municipal Zoraide Eva das Dores, located in Itapecerica da Serra, São Paulo, and at Health Centers in the Itapecerica da Serra and the cities of Juquitiba, São Lourenço and Embú-Guaçú.
Results
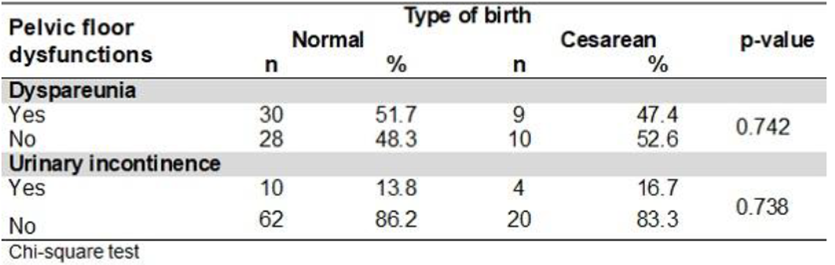
During pregnancy, 52.1% of women reported UTI and 30.2%, UI. Two and six months after birth, there was a prevalence of 4.2% and 11.8% of UTI, 17.7% and 11.8% of UI, 8.4% of AI (6.3% of flatus incontinence and 2.1% of feces) and 2.0% (only flatus incontinence; there was no faecal incontinence); and 48.1% and 17.8% of dyspareunia, respectively. There was no statistical association between the mode of delivery and dyspareunia and UI (p=0.742 and p=0.738; respectively).
Conclusions
The most frequent pelvic floor dysfunctions (PFD) after birth were IU and dyspareunia. There was spontaneous reduction of the PFD in the sixth month after birth. The early identification of these diseases is extremely important to prevent, diagnose and treat any harm to women’s physical and emotional health.
Keywords Urinary tract infection; Urinary incontinence; Anal incontinence; Dyspareunia; Primiparous; Postpartum period
INTRODUCTION
The shape and regular function of the pelvic floor (PF) are determined by the interaction and proper functioning of their structures. As such, gestation and birth can cause trauma and diminish muscular tone, leading to problems collectively termed pelvic floor dysfunction. These problems have a negative impact on the quality of life of the woman1. The expression Pelvic Floor Dysfunction (PFD) is a general term used to describe the conditions which compromise the mechanics of urinary and faecal continence and/or the support of pelvic organs2.
The PF, which is the collection of tissues that cover the inferior portion of the pelvis, is composed of the pelvic and urogenital diaphragms and the endopelvic fascia. The diaphragms are formed by muscles organized in both superficial and deeper layers of the perineum, which act on the support mechanisms of the pelvic viscera, which impact urinary and anal continence as well as sexual function3. When this musculature loses its integrity, the risk of the occurrence of PFDs is increased, being urinary incontinence (UI), anal incontinence (AI) or Prolapse of Pelvic Organs (PPO)4. Statistically, approximately one third of women present PFD with differing levels of seriousness2. UI and AI are distressing, and in the long term potentially incapacitating, situations which can affect women of various ages, with the first episode occurring during pregnancy or postpartum5.
Factors linked to pregnancy and childbirth are noted as risks for the development of PFDs, including long labour times, prolonged expulsive period, the application of episiotomy and the increased weight of the newborn6)(7.
An association between natural and assisted vaginal childbirth as well as obstetric injuries, especially of the anal sphincter, and UI and AI, has been cited in the literature8. As such, the results of studies about the potential for caesarean sections to diminish the risk of UI, especially if preceded by labour, are very controversial9)(10.
Urinary incontinence is defined by the International Continence Society (ICS) as the involuntary loss of any quantity of urine, and it is one of the most frequently occurring conditions among women of any age group11. Apart from this, it is a serious public health issue, and has physical, social, psychological and economic implications. The majority of women do not inform their health professionals of these issues for feeling embarrassed, believing nothing can be done, not knowing who to talk to about it, or believing that the health professionals would not be interested5. Estimates of the prevalence of UI show discrepancies, with rates that vary from 17% to 45% in adult women2.
Changes attributed to pregnancy contribute to postpartum UI, and there is scientific evidence that, when it occurs during pregnancy, the problem becomes a risk factor of its occurrence in the postpartum period1.
Anal Incontinence consists of the involuntary loss of feces or flatulence, defined as the incapacity to maintain the physiological control of intestinal contents to a socially adequate time and location. It is sub-categorized into faecal incontinence (involuntary loss of faeces) and flatus incontinence (involuntary loss of gasses)11. When categorized as moderate or severe, faecal incontinence can cause embarrassment and social isolation, as well as causing the woman to have a reduced activity set and severely diminished quality of life12.
A study of approximately 15 thousand women post vaginal childbirth observed that AI was reported by 21% of women with a rupture in the anal sphincter, and the inability to control gasses was the most prevalent symptom encountered8. Even though AI is a less common complication than UI, a multicenter Italian study reported a prevalence of 16%10.
Birth can also have a great impact on the sexual function of the woman and many experience perineal pain, in addition to dyspareunia, in the period after giving birth, which can compromise, above all, the sexual health of the woman, even when dealing with a short-term complication not exceeding 12 months post-partum13. Apart from that, the relationship between obstetric risk factors including type of birth, perineal trauma and dyspareunia, is not well understood14.
Dyspareunia is a common and under-reported problem, which can significantly prejudice the health, quality of life, and sexual relationship of the woman. It is a complicated symptom to diagnose and treat, and can cause frustration on the part of both the patient and health professionals. However, the process of obtaining this history and of making continual exams establishes a relationship between patient and professional, which is essential in the treatment of this type of dysfunction15. Dyspareunia is worse in postpartum women that have perineal trauma, or in those who undergo assisted birth16.
Although urinary tract infection (UTI) is not considered a PFD, women who present some of these dysfunctions have a higher propensity to develop it. The higher rates of recurrence and the growth in the antimicrobial resistance of uropathogens threaten to considerably raise the use of financial resources in the treatment of these infections and represent a serious public health issue17.
In Brazil, there is very little research about the theme of PFDs in the postnatal period of up to six months.
In light of this, the objectives of this study were to estimate the prevalence of UTIs, UI, AI and dyspareunia in primiparous women, between two and six months after birth, and identify the association between dyspareunia and UI, and the type of birth.
METHOD
This is a prospective observational study, based on data collected from the transversal study18, both undertaken at the Centro do Parto Normal do Pronto Socorro e Maternidade Municipal Zoraide Eva das Dores [Centre for Normal Birth of the Emergency and Maternity Municipal hospital of Zoraide Eva das Dores], located in the municipality of Itapecerica da Serra, São Paulo, and in the Basic Units of Health (BUH) in São Paulo and in the municipalities Juquitiba, São Lourenço, and Embú-Guaçú. The aforementioned transversal study had the following objectives: identify the pelvic floor muscular strength (PFMS) of primiparous women after normal birth and caesarean sections between 50 and 70 days postpartum, and compare the PFMS of primiparous women after normal and caesarean births in relation to social demographic characteristics, clinics, urogynecologists, perineal exercise, birth data, perineal conditions, and clinical data of the newborn.
The inclusion and exclusion criteria used in this study are the same used in the transversal study18, which were: be a primiparous woman with a normal or caesarean birth at term, without previous abortions; have a single alive newborn which had a normal birth with cephalic presentation (in the case of normal birth); not being submitted previously to abdominal or urogenital surgery; not be affected by illnesses or physical conditions that could interfere with the strength of the pelvic floor musculature; not have difficulty in understanding Portuguese or in communication. Only women with difficulty inserting the perineometer into the vagina were excluded.
The sample size calculation was based upon the means of the PFMS of women who underwent normal birth or caesareans in the previous study19 which found an effect size of 0.669 (Cohen’s d, alpha=0.05, beta=0.90). Assuming a type-I error of 5% and testing power of 90%, 96 women would be needed.
The sample is composed of 96 primiparous women, which gave birth at PSMMZED, between January and August of 2014, and considered the distribution of the type of birth registered in the registry of births of 2012, in which it was observed that, for every woman who undergoes caesarean birth, three have a normal one. As such, 24 post-caesarean and 72 normal-birthing women were included, totaling 96 participants.
Only women who signed the Informed Consent were eligible to participate.
Data was collected in three steps. In step 1, which occurred during the immediate postpartum period (within 48 hours), the recruitment and the initial phase of the interview, by way of the collection of the prenatal information cards and medical history of the woman, and the second appointment scheduled to be within 50 and 70 days of birth. Before this second consult, telephone contact was made, in order to confirm the presence of the subject. If she was unable to attend, a new appointment was made via telephone. In stage 2, the second part of the interview was carried out at the BUH or maternity. In stage 3 (between 170 and 190 days postpartum), a second interview was made with the now postpartum woman.
The form used to register the information was the same used in the previously stated study18. The data was entered in duplicate in the Statistical Package for Social Sciences version 22.0 for Mac (SPSS). The database was validated and data imported to Microsoft Excel, which was then used to calculate absolute and relative frequencies for qualitative variables and the central tendency and dispersion for the quantitative variables.
The Chi-squared distribution test was used to evaluate the association between dyspareunia and UI with type of birth. The same SPSS software was used to perform the analysis. Values were considered statistically significant with p-values lower than 0.05.
The study was approved by the Committee of Ethics in Research at the School of Nursing of the University of Sao Paulo (CAAE:13545113.5.0000.5392) and by the Municipal Council of Health for the Municipal Secretary of Health of Itapecerica da Serra, Sao Paulo.
RESULTS
In relation to the sociodemographic characteristics of the primiparous women, it was found that the average age was 21.7 (standard deviation=4.8) years, with the minimum being 13 and maximum 37 years. There was a predominance of women of mixed race, with high school education, living with the partner and without paid employment (Table 1).
Regarding the clinical and gynecological characteristics; the mean age of menarche was 12.8. The beginning of sexual relationship was 16.6 and active sex life was 5.3 years. Other average values obtained were as follows: weight 59.2kgs, height 159.7cm, Body Mass Index (BMI) of 23.3 and weight gain during pregnancy of 10.6kg. The women made, on average, 8 prenatal consults (data not presented in the table).
75% of the women included had a normal birth, and the majority of them presented with some type of perineal trauma, the majority being episiotomy. Almost all of the women who had perineal trauma underwent perineal repair (Table 1).
Table I Distribution of women according to sociodemographic characteristics, type of delivery and perineum conditions after normal delivery. Itapecerica da Serra - 2014-1015.

It is worth commenting that the newborns had an average weight of 3 239.2 (±419) grams and cephalic circumference of 33.9 (±1.5) centimeters (data not presented in table). Six months postpartum, telephone contact was made with 51 (53.1%) of the women for the second interview.
The majority of participants informed that they did not use contraceptives two months after birth, although there was a definite increase in use at six months (14.3 percentage points).
Two months postpartum, approximately 80% of the women, independent of the type of birth, returned to sexual activity (data not presented in table), and, of these, practically half complained of dyspareunia. At six months, all of the postpartum women resumed their sexual activity, and less than a fifth cited dyspareunia (Table 2). For those that did not return to sexual activity, the main reasons were: fear of pain (n=8), no partner (n=7), unwilling (n=2), partner with herpes (n=1), and fear of becoming pregnant (n=1) (data not presented in table).
Table II Number and percentage of women to contraceptive use, the return of sexual activity, reason for not returning to sexual activity and dyspareunia, at 2 and 6 months postpartum (PP). Itapecerica da Serra - 2014-1015.

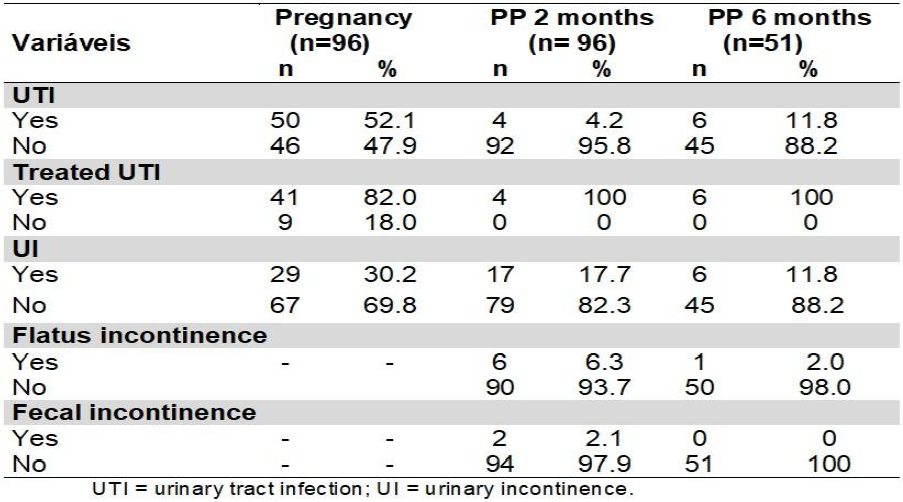
In regard to UTI, a large part of the women presented this complication during gestation, and the majority had it treated. Comparing the prevalence of UTI in pregnancy with the postpartum period, a 4.2% fall was noted at two months and a definite increase to 11.8% at six months after giving birth. In the postpartum period, all women reported having treated the infection (Table 3).
Among the PFDs, a little less than a third reported a UI before pregnancy, and 17.7% and 11.8% at two and six months postpartum, respectively. Flatus incontinence was reported by few (6.3%) women at two months and only one confirmed that it continued at six months. Two women cited faecal incontinence at two months, and none at the six month point. (Table 3)
Table III Number and percentage of women according to urinary tract infection (UTI) and pelvic floor dysfunction in pregnancy and postpartum (PP) at 2 and 6 months. Itapecerica da Serra - 2014-1015.
The results of Table 4 show that there was no association between the type of birth and dyspareunia and UI.
DISCUSSION
This study observed a high proportion of adolescent postpartum women (36.5%), average age of 21.7 years, with variation between 13 and 24 years; a value which is above the Brazilian pregnancy index in that age group, which was 20% in 2010, according to the System of Information about Live Newborns20. This fact could be due to the early beginning of sexual relationships found in the results, which increases the propensity of pregnancy in these adolescents.
It was found that a large number of women had studied until high school, which concurs with the age of the participants.
In this sense, people with a lower level of education can present difficulty in understanding the recommendations offered by health professionals. Against these observations, it is worth noting that the strategies to be implemented as regards the prevention and treatment of PFDs should consider the women’s level of education.
At two months postpartum, a little over half of the women were using contraceptives, yet there was a definite increase at six months. This higher proportion may be related to the advice offered at postpartum consultations, to raising awareness of the need to avoid an early pregnancy, and to the period in which the majority resumed sexual activity.
The variation in weight during gestation and BMI found were within the normal range in accordance with the nutritional state of gestation and pre-birth21. The study found that weight gain in the gestation period increases the risk of PFD and as such this datapoint is relevant in the woman’s assessment22. It should be noted that, in this study, the data for weight during pregnancy were those registered on the prenatal card, and in some cases this variable was not recorded. Due to this, it was not possible to ascertain the total weight gain with precision, a fact that limits the discussion of these values.
Regarding perineal conditions, the study found that spontaneous perineal injuries occurred in around half of the women, episiotomy used on a little over a third of those, and perineal stitches applied to all. The widespread use of episiotomy, associated with the context of interventionist professionals at the ward of the study, is not in agreement with the rate of 10% recommended by the WHO. This fact leads to the question of the possibility of incorrect classification or of unnecessary suturing of spontaneous lacerations, since a great number of the women presented with a first degree laceration, which, in many cases, does not require suturing, on the recommendation of the WHO23. Thus, although selective episiotomies have a significant place in obstetric practice, its routine use is not justified, as it increases the risk of maternal trauma and complications during vaginal birth, which impact on the chances of developing PFDs in the postpartum6. In the current study, the variable of perineal condition was not associated with PFDs, due to the small number of cases observed in each category.
In this study, a little over half of the women presented with UTI during gestation, and the majority informed that they had undergone treatment. The elevated frequency of occurrence of this disease during pregnancy in this study is reasonable due to the fact that pregnancy raises the risk of infection, as a result of physiological alterations during this period24. In relation to UTIs, one study found that adolescent women who had a lower economic level and lesser education and did not live with the partner were those who most frequently required hospitalization to treat a UTI25. In the current study, at both two and six months postpartum, few women reported UTIs and all confirmed treatment with antibiotics. However, this variable was obtained by voluntary admission by the woman, which could present a discrepancy in information.
In the current study, the prevalence of UI was 20.5 percent points more in the gestation period than six months after birth. These findings are similar to those of a prospective study9, which also found increased indexes during pregnancy compared to the postpartum period (30.6% versus 6.7%). The highest rate at three months postpartum was observed in the Australian cohort (29.3%)5. Similarly, another prospective cohort of primiparous women found that 30% had any type of UI one year after their first vaginal birth1. The reasons why prevalence may vary between studies include difference in populations, study design, and subgroups studied7. Furthermore, in the current study, there were no cases of 3rd or 4th degree lacerations, which can also explain the low prevalence of PFDs found in the sample.
Although the literature indicates that caesarean section seems to protect against UI22, the findings in the current study showed no association between the type of delivery and UI.
The prospective cohort of primiparous women which were investigated for 5-10 years after normal or caesarean birth asserted that the relative risk of PFDs after vaginal birth was higher for women with symptoms of UI (RR 1.15, confidence 95% interval 0.92-1.42)26.
Thus, the screening of women with or without UI episodes during pregnancy should be performed, due to their importance in prevention and early treatment. Supporting this, a clinical trial pointed out that pelvic floor muscle exercises applied during pregnancy and postpartum increased the muscle strength of the pelvic floor and avoided the worsening of PFDs27.
Similarly, a systematic review of the Cochrane Library, which included 21 clinical trials and involved 1 281 women, assessed the effects of pelvic floor training programmes (PFTP) on women with any type of UI compared to no treatment or other treatments. Women with UI who were part of PFTP were more likely to report healing or improvement in symptoms. The reviewers concluded that the assessment supports the widespread recommendation that PFTP be included as a priority in programmes to assist women with UI, regardless of the type of incontinence28.
The frequency of AI found in the current study was also lower than the UI at 2 months, as expected, and only one occurrence of flatus incontinence was observed at six months. It should be noticed that all of the women with either type of AI had a normal vaginal birth. As previously mentioned, this fact did not allow a statistical analysis. A study that examined 744 women at three months postpartum found a much higher prevalence of AI (16.3%). The presence of UI in pregnancy was an independent predictor for persistent UI (Odds Ratio (OR) 4.6; p<0.001) and AI (OR 3.6; p<0.001). The family history of UI or AI was associated, respectively, with UI (OR 2.6; p <0.001) and AI (OR 2.4; p <0.001), with those at 3 months postpartum10.
A study with primiparous women shows that this intercurrence was four times more frequent in the postpartum period, regardless of the method of delivery, and persisted for six months after delivery. The data showed that women who suffered anal sphincter rupture during vaginal delivery had twice the risk of faecal and flatus incontinence compared to those without anal sphincter injury. On the other hand, caesarean section without previous labour was not associated with PFD. It is important to note that the postnatal examination is an opportune moment to ask about intestinal function, especially in the case of anal sphincter injury at delivery and to offer appropriate interventions to symptomatic women12.
A study that investigated whether primary care providers routinely ask about postpartum UI and AI found that more than 70% of women with severe urinary incontinence and/or faecal incontinence had not discussed their symptoms with a physician or nurse5.
Regarding sexual health in the postpartum period, the majority of the postpartum women had resumed sexual relations at two months and all of them by six months. These results are similar to those found in studies with Australian and Chilean women14)(16.
At two months postpartum, half of the women with sexual activity reported dyspareunia, and at six months, there was a reduction in that complaint to about one fifth. Similar findings were verified at three months postpartum in a multicenter prospective cohort, with 44.7% of the women citing this discomfort; however, the prevalence at six months was more than double the current study (43.4%). This study also evaluated the persistence of dyspareunia at 12 and 18 months postpartum, which remained at 28.1% and 23.4%, respectively14.
Although researchers report that women with caesarean delivery or normal delivery without perineal trauma report less significant pain in the first postpartum relationship29, our results indicated that there was no association of dyspareunia with type of delivery.
The previously cited cohort found that women with operative vaginal delivery (forceps or vacuum extraction) were three times more likely to have dyspareunia at 6 months postpartum. Emergency caesarean section and vaginal delivery with lacerations and / or sutured episiotomy were also associated with a higher probability of dyspareunia at 6 months postpartum. The authors suggest that the higher prevalence of persistent dyspareunia in women who had operative delivery allows us to identify important questions about the long-term impact of obstetric procedures on women's health14.
Another study also found that women who suffered from perineal lacerations are five times less likely to be sexually active compared to women with an intact perineum. The authors mention that only 15% of the postpartum women reported sexual dysfunction to health professionals15. In this sense, it is fundamental to investigate the factors that lead these women to have pain in the relationship. Moreover, the literature states that the sexual life quality of couples in the first postnatal year is clearly affected by several factors associated with this phase30.
The lack of knowledge by health professionals about the relevance of addressing this issue should be investigated in order to enable them to deal with this subject. It is necessary for women to be guided, during the pre or postnatal period, about these dysfunctions, which are often unduly perceived as normal and inherent in the pregnancy process, but which must be identified as early as possible so that they can be treated properly.
Among the limitations of this study, it can be mentioned that the first 48 hours after giving birth may not be the ideal time for women to be recruited. However, in Brazil, women do not have a guaranteed hospital bed at the time of delivery, which makes it difficult to know where they will give birth. Thus, the recruitment of women during pregnancy was unviable. In addition, the low prevalence of AI and UI observed in this investigation made it difficult to assess the association with the type of delivery, so our results should be interpreted with caution, as they may reflect a limited study power for comparisons among the subgroups surveyed. Finally, there was a high rate of follow-up loss at 6 months postpartum, only 51 women (53.1%) of the original participants were contacted in stage 3.
CONCLUSION
During pregnancy, 52.1% of the women reported having a UTI, evidencing that this morbidity is frequent in pregnancy. In the postpartum period, there was a reduction in the prevalence of UTI (40.3 percentage points at six months), and all women reported having been treated for this morbidity.
In relation to the UI, 30.2% of the women cited this PFD during pregnancy, and this proportion decreased to 17.7% and 11.8% at two and six months, respectively.
At two months postpartum, AI was present in 8.4%, of which 6.3% were of flatus incontinence and 2.1% of faeces, whereas at 6 months there was only 2.0% of incontinence of flatus and none of faeces. Dyspareunia was present in 48.1% and 17.8% of women, at two and six months postpartum, respectively. There was no statistical association between type of delivery and dyspareunia and UI. The early identification of PFD is extremely important for the prevention, diagnosis and treatment of injuries to the physical and emotional health of women, both during pregnancy and postpartum.
REFERENCIAS
1. Svare JA, Hansen BB, Lose G. Risk factors for urinary incontinence 1 year after the first vaginal delivery in a cohort of primiparous danish women. Int Urogynecol J. 2014;25(91):47-51. [ Links ]
2. Kim S, Harvey MA, Johnston S. A review of the epidemiology and pathophysiology of pelvic floor dysfunction: do racial differences matter? Obstet Gynaecol Can. 2005;27(3):251-259. [ Links ]
3. Cabar FR, Codarin RR, Bunduki V. Anatomia da pelve feminina. In: Zugaib M, Francisco RPV. Zugaib Obstetrícia. 3ª ed. Barueri, SP: Manole; 2016. p. 34-49. [ Links ]
4. Assis TH, Sá ACAM, Amaral WN, Batista EM, Formiga CKMR, Conde DM. Efeito de um programa de exercícios para o fortalecimento dos músculos do assoalho pélvico de multíparas. Rev Bras Ginecol Obstet. 2013;35(1):10-5. [ Links ]
5. Brown S, Gartland D, Perlen S, McDonald E, MacArthur C. Consultation about urinary and faecal incontinence in the year after childbirth: a cohort study. BJOG. 2014;122(7):954-62. [ Links ]
6. Ferederice CP, Amaral E, Ferreira NO. Sintomas urinários e função muscular do assoalho pélvico após o parto. Rev Bras Ginecol Obstet. 2011;33(4):188-95. [ Links ]
7. Yohay D, Weintraub AY, Mauer-Perry N, Peri C, Kafri R, Yohay Z, et al. Prevalence and trends of pelvic floor disorders in late pregnancy and after delivery in a cohort of Israeli women using the PFDI-20. Eur J Obstet Gynecol Reprod Biol. 2016;200:35-9. [ Links ]
8. Laine K, Skjeldestad FE, Sanda B, Horne H, Spydslaug A, Staff AC. Prevalence and risk factors for anal incontinence after obstetric anal sphincter rupture. Acta obstetGynecol Scand. 2011;90(4):319-24. [ Links ]
9. Valeton CT, Amaral VF. Evaluation of urinary incontinence in pregnancy and postpartum in Curitiba mothers program: a prospective study. Int Urologynecol J. 2011;22(7):813-8. [ Links ]
10. Torrisi G, Minini G, Bernasconi F, Perrone A, Trezza G, Guardabasso V, et al . Prospective study of pelvic floor dysfunctions related to delivery. Eur J Obstet Gynecol Reprod Biol. 2012;160(1):110-5. [ Links ]
11. Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C., et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse and fecal incontinence. Neurourol Urodyn. 2010;29(1):213-40. DOI:10.1002/nau.20870. [ Links ]
12. Borello-France D, Burgio KL, Richter HE, Zyczynski H, FitzGerald MP, Whitehead W. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006;108(4):863-72. [ Links ]
13. Bertozzi S, Londero AP, Fruscalzo A, Driul L, Marchesoni D. Prevalence and risk factors for dyspareunia and unsatisfying sexual relationships in a cohort of primiparous and secondiparous women after 12 months postpartum. Intern J Sexual Health. 2010;22(1):47-53. [ Links ]
14. McDonald EA, Gartland D, Small R, Brown SJ. Dyspareunia and childbirth: a prospective cohort study. BJOG. 2015;122(5):672-9. [ Links ]
15. Lucena HM, Mukhopadhyay S, Morris E. Dyspareunia: a difficult symptom in gynaecological practice. Obstet Gynaecol Reprod Med. 2015;25(4):96-101. [ Links ]
16. Chaparro GM, Pérez VR, Sáez CK. Función sexual femenina durante el período posparto. Rev Obstet Ginecol Venez. 2013;73(3):181-6. [ Links ]
17. Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269-84. [ Links ]
18. Mendes EPB, Oliveira SMJV, Caroci AS, Francisco AA, Oliveira SG, Silva RL. Pelvic floor muscle strength in primiparous women according to the delivery type: cross-sectional study. Rev Latino-Am Enfermagem [on line]. 2016;24(e2758). [ Links ]
19. Menta SS, Schirmer J. Relação entre a pressão muscular perineal no puerpério e o tipo de parto. Rev Bras Ginecol Obstet. 2006;28(9):523-9. [ Links ]
20. Brasil. Ministério da Saúde. Informações de Saúde. Estatísticas vitais. Nascidos vivos - Brasil. Proporção de nascidos vivos de mães adolescentes segundo Unidade de Federação (Datasus), 2010. [acesso em 30 marc. 2015]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?idb2011/g15.def [ Links ]
21. Melo ME. Ganho de peso na gestação. ABESO [on line]. ABESO; s.d. [2015 ago. 08]. http://www.abeso.org.br/uploads/downloads/5/5521b01341a2c.pdf [ Links ]
22. Rørtveit G, Hannestad YS. Association between mode of delivery and pelvic floor dysfunction. Tidsskr Nor Legeforen. 2014;134(19):1848-52. [ Links ]
23. Organização Mundial da Saúde-OMS. Assistência ao parto normal: um guia prático. Brasília (DF): OPAS/USAID; 1996. [OMS/SRF/MSM/96.24 ] [ Links ]
24. Parveen K, Momen A, Begum AA, Begum M. Prevalence of urinary tract infection during pregnancy. J Dhaka National Med Coll Hosp. 2011;17(2):8-12. [ Links ]
25. Hackenhaar AA, Albernaz EP. Prevalência e fatores associados à internação hospitalar para tratamento da infecção do trato urinário durante a gestação. Rev Bras Ginecol Obstet. 2013;35(5):199-204. [ Links ]
26. Huser M, Janku P, Hudecek R, Zbozinkova Z, Bursa M, Unzeitig V, Ventruba P. Pelvic floor dysfunction after vaginal and cesarean delivery among singleton primiparas. Int J Gynaecol Obstet. 2017;137(2):170-3. [ Links ]
27. Sut HK, Kaplan PB. Effect of pelvic floor muscle exercise on pelvic floor muscle activity and voiding functions during pregnancy and the postpartum period. Neurourol Urodyn. 2016;35(3):417-22. [ Links ]
28. Dumoulin C, Hay-Smith EJC, Mac Habée-Séguin G, Mercier J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: A short version Cochrane Systematic Reviews with Meta-Analysis. Neurourol Urodyn. 2015;34(4):300-8. [ Links ]
29. Buhling KJ, Schmidt S, Robinson JN, Klapp C, Siebert G, Dudenhausen JW. Rate of dyspareunia after delivery in primiparae according to mode of delivery. Eur J Obstet Gynecol Reprod Biol. 2006;124(1):42-6. [ Links ]
30. Yeniel AO, Petri E. Pregnancy, childbirth, and sexual function: perceptions and facts. Int Urogynecol J. 2014;25(1):5-14. [ Links ]
Received: May 01, 2017; Accepted: September 24, 2017











 text in
text in