Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.19 no.60 Murcia Out. 2020 Epub 21-Dez-2020
https://dx.doi.org/10.6018/eglobal.414741
Originals
Clinical-epidemiological study of TB-HIV coinfection in priority municipality: 10 years análisis
1 Nurse, Master of Nursing, Federal University of Piauí. Brazil. inarasena22@gmail.com
2Nurse, specialist in Epidemiological Surveillance - School of Public Health of Ceará. Brazil
3 Graduating in Nursing - Vale do Acaraú State University. Brazil.
4Nurse, Master in Health and Community - Federal University of Piauí. Brazil.
Objective:
To know the clinical and epidemiological profile of TB / HIV in a priority municipality in Ceará.
Method:
Descriptive, epidemiological study, carried out through data collection. Collection performed in October 2019 for the years 2009 to 2019. The variables age group, sex, education, race, clinical form, case closure, antiretroviral therapy were used. The data were taken from SINAN (Information System for Notifiable Diseases), then tabulation was performed in the Tabwin software and later the records were transported to Excel.
Results:
71 cases of TB-HIV co-infection were registered, which corresponds to 4.28% of the cases of tuberculosis in the municipality. From the analysis of the database about notified cases, in 2014 the largest proportion of cases (6.72%) was identified, followed by 2013 (6.43%). It is noteworthy that as of 2017, there is a decline in cases in the municipality.
Conclusion:
The results obtained indicated that, in the investigated period, 4.3% of individuals with TB had coinfection with HIV, which shows its epidemiological relevance as a comorbidity with a great impact on public health.
Key words: Tuberculosis; HIV; Coinfection; Epidemiology
INTRODUCTION
According to the World Health Organization (WHO), Tuberculosis (TB) is still considered a strong problem impacting greatly the public health in Brazil, being currently identified as the main infectious disease that kills the most in the world, taking almost one and a half million people’s lives in 2017, which led a ranking among the top ten causes of deaths in general 1. This disease is associated with variables such as co-infection by the Human Immunodeficiency Virus (HIV), has a major impact on mortality from Acquired Immunodeficiency Syndrome - AIDS, due to the fact that Tuberculosis is responsible for about 50% of deaths in immunocompromised patients2.
TB is transmitted by Mycobacterium Tuberculosis, Koch's bacillus, which is eliminated through aerosol droplets on breathing, coughing and sneezing, requiring an infection in the pulmonary alveoli. It is a disease that presents itself mainly in the pulmonary form, having several characteristic clinical manifestations and inherent to TB, such as cough lasting for more than 15 days, fever, asthenia, sweating, chest pain, cachexia, hemoptysis, and it can affect several other systems of the organism, such as the bone and nervous systems 3 4.
As it is the main cause of death of patients among people with HIV, where worldwide, PLHIV were 20 times (17 - 23) more likely to become ill with TB than those without HIV, in 2017. It also stands out, those who face the threat of drug-resistant TB, if the diagnosis is delayed, there is an increased risk and mortality from multidrug-resistant and extensively drug-resistant TB 5.
Thus, TB / HIV co-infection presents itself as a challenge to public health services, due to the high rates of treatment abandonment and it is one of the major causes of death and hospital care in Brazil. Highlighting São Paulo, as one of the main states with the highest number of people affected with Tuberculosis and HIV, with almost 10% of cases of TB / HIV co-infection 6,7.
The high incidence of TB / HIV co-infection cases, in the period from 2001 to 2016, presented higher rates in the state of Alagoas, representing an exorbitant increase of almost 2000% of people diagnosed with HIV. With the majority being male patients, with about 74.2%. 93.7% being economically productive, 92.5% have low education and are black, pointing to TB as a serious comorbidity for HIV + patients 8.
The educational level, the age group, the degree of exposure to bacterium myco tuberculosis, the permanence in private institutions, such as asylums and prisons, vulnerable behaviors, unfavorable environmental conditions, and among several other factors, can be determinant causes to result in a high risk of TB / HIV co-infection. About 10% of TB infection cases were identified in HIV-positive patients living in private institutions, with a percentage difference when compared to other regions of the country, being lower in the Northeast and higher in the South 9.
It is of fundamental importance to use Tuberculosis control strategies to reduce the incidences of the disease in the country. Leading to a place so that there is a viability of control, through the awareness of an appropriate treatment, the involvement of the health team with the particularity of each patient, the planning and adopting technological strategies that have an impact on the population, relating to the prevention and adequate continuity of treatment, as well as bringing innovations to enable the construction of new health policies 10.
However, there are still weaknesses in relation to the use of strategies to combat and control TB, pointing to a situation of decay in the entire country. Ranging from gaps in the work processes in Primary Care, to the lack of commitment to investments to improve conditions. population health 11.
In view of the epidemiological relevance of Tuberculosis and the need to contribute to the renewal of the peculiarities of this disease in relation to HIV, it is essential to carry out this study on the temporal trends of TB in association with HIV, in which it can subsidize the insertion of measures of prevention and control of this public health problem. Thus, this study aims to present the epidemiology of TB / HIV co-infection in a population in the interior of the state of Ceará, in the period from 2009 to 2019.
MATERIAL AND METHOD
It is a descriptive, epidemiological study, carried out through a survey in the database. The data was collected in October 2019 and is for the years 2009 to 2019. The study was conducted in the municipality of Sobral-Ceará, whose population is 208,935 inhabitants, located in the northeast of Brazil. 12
The main variables obtained for epidemiological information were: age range, sex, education, race of patients, case closure, clinical form, use of antiretroviral therapy. In order to define the clinical-epidemiological profile and discuss the incidence of cases in the state, in the period from 2009 to 2019.
The data was collected by the researchers themselves, who are part of the Health Surveillance and Epidemiological Surveillance cell, through the database available in the Notifiable Diseases Information System - SINAN. This is mainly fed by the notification and investigation of cases of diseases and conditions that appear on the national list of compulsory notification diseases.
After the collection, data was tabulated in the TABWIN progrAm Subsequently transported to Excel for simple descriptive analysis. The most significant findings were presented in graphs and tables.
The discussion of the data was based on scientific production on the subject. Since the research was carried out from a public domain database, it was not necessary to submit it to the Research Ethics Committee, as it was based on Resolution No. 510, of April 7, 2016, of the National Health Council13. It is noteworthy that all ethical principles for national and international research were respected.
RESULTS
There were 71 cases of TB-HIV co-infection, which corresponds to 4.28% of Tuberculosis cases in the municipality of Sobral. From the analysis of the database about the notified cases, in 2014 the largest proportion of cases (6.72%) was identified, followed by the year 2013 (6.43%). It is noteworthy that as of 2017, there is a decline in cases in the municipality (Graph 1).
Regarding the profile of the cases, there is a predominance of males (78.87%), aged between 25 and 44 years (77.46%), browns (78.88%) and whites (11.27%). It is worth mentioning the high proportion of information ignored in education (39.40%), in addition to 20 cases (28.16%) having incomplete elementary education, with the majority of cases (92.95%) residing in the urban area (Table 1).
Table 1: Distribution of the social characteristics of the 2009-2019 TB-HIV co-infection cases (N = 71). Sobral- CE, Brazil. 2019.
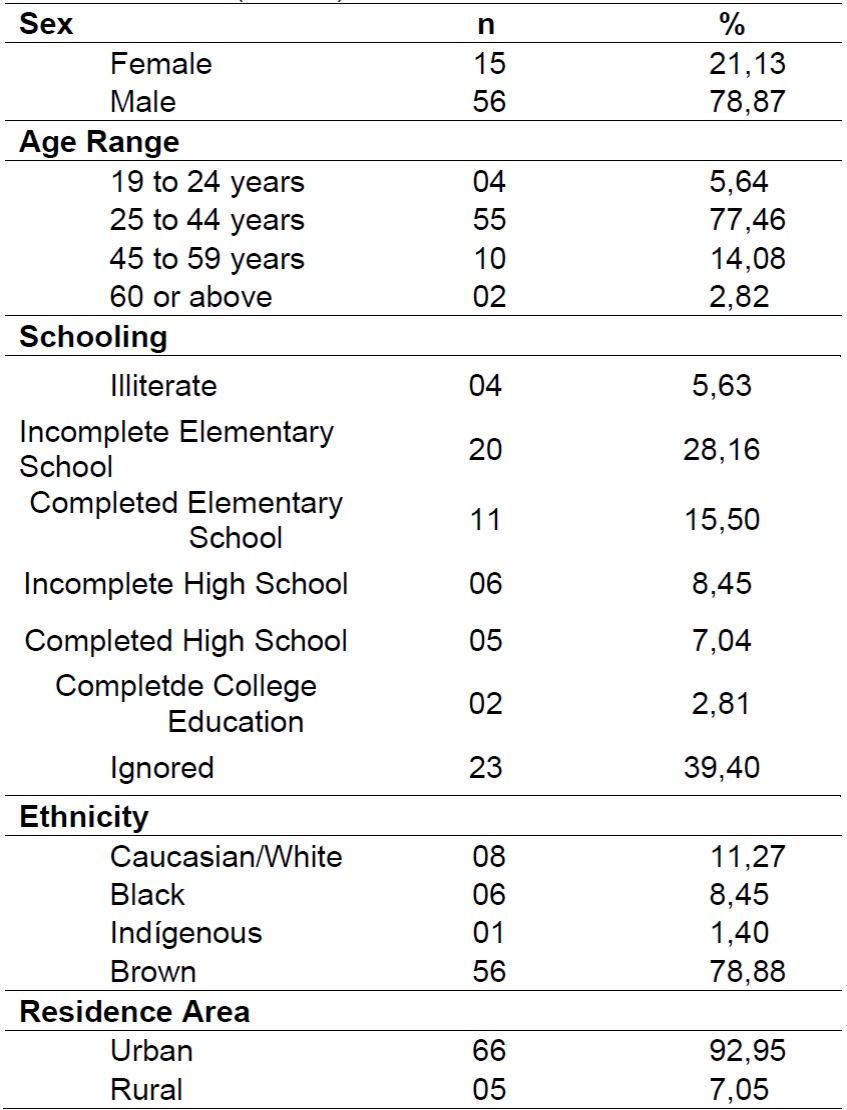
Source: SINAN-VIGEP. Data exported on 11/20/2019.
The most common clinical form was pulmonary in 51 of the cases (71.83%), followed by extrapulmonary in 17 cases (23.94%). Regarding the situation of closure, most individuals (69.01%) with TB-HIV co-infection were cured.
With regard to therapy, 31 of the patients (43.66%) use antiretrovirals and 25 of the individuals (35.21%) undergo treatment directly observed. It is worth noting that 53.52% of the information was ignored, making a more detailed analysis of the data difficult (Table 2).
DISCUSSION
TB / HIV co-infection began to be monitored by WHO in 2004 with the aim of reducing its impact on global public health, through the establishment of routine HIV testing for all patients diagnosed with tuberculosis, respiratory symptoms and patient partners. with TB / HIV. Based on this measure, it is estimated that 5.8 million lives were saved worldwide, it is also noteworthy that collaborative activities focused on TB-HIV and the management of comorbidities is one of the components of the End TB strategy 14,15.
Epidemiological data shows the magnitude of TB / HIV co-infection, estimated at 400,000 deaths and 1.2 million incident cases in 10.4 million confirmed cases of tuberculosis. Furthermore, in a study carried out in Portugal, the prevalence of 70% of tuberculosis (TB) cases with known HIV status, Spain (60%), Holland (59%), Belgium (50%), with the most contrasting value found in Serbia (5%) 16.
In the Brazilian scenario, 72,788 new cases of tuberculosis were identified, of which 6,501 presented positive results for HIV, which represents a proportion of TB-HIV coinfection of 9.4%. The Federative Units with the highest proportion of TB / HIV co-infection were Rio Grande do Sul (18.3%) and Santa Catarina (16.2%) 17.
On the other hand, in Ceará, during the period from 2013 to 2017, there was an increase of 8.9% in the performance of tests for HIV testing, going from 61.5% to 70.4%, and a stable coinfection at the time. over the years 18. This reality differs from the data found in Sobral, where there was a decline in the prevalence of TB / HIV coinfection cases throughout the selected historical series, which may be related to the underreporting of these diseases, which makes it difficult to estimate the real prevalence of coinfection. A useful tool to monitor the occurrence of coinfection.
The demographic characteristics of the participants are similar to other studies that showed a predominance of males. The reasons for a higher proportion of cases of tuberculosis / HIV coinfection in male individuals, possibly, can be explained by their behavioral characteristics. Such as, the greater difficulty in adhering to treatment and the fragile access of this population to services and actions offered by the Health Units19.
As for the race / color variable, 78.88% of the individuals were brown and only 11.27% were characterized as white. In a study carried out in a reference hospital in the city of Rio de Janeiro, a different reality was identified with a rate of 55.5% for self-reported black skin color and 44.5% for white skin color 20.
Regarding the age group, it was noted that co-infection affects more individuals between 25 and 44 years old, living in the urban area. The profile of co-infection has been changing in Brazil, despite the high prevalence in the south and southeast regions, incidence rates have increased in the north and northeast regions, with a predominance of cases in patients aged 25 to 59 years, living in the urban area. A fact that is associated with the lifestyle of young adults, often linked to a lack of awareness of their vulnerability, exposing them to the HIV virus and tuberculosis. It also stands out, spatial patterns based on age categories showed a generalized risk of coinfection for the ages of 25 to 34, followed by 35 to 44 years 21,22.
Weaknesses were also detected in filling out the forms that presented ignored information, making it difficult to use this data and impairing the quality of the information. Since the potential usefulness of the case notification data provides robust estimates for the wide space-time structure of co-infection TB-HIV 22.
Regarding the education variable, in 39.40% of the cases, they were marked as ignored information. Being an essential field in the notification, in view of the existence of a pattern of prevalence in the studies that presented the sociodemographic profile, in which it was possible to observe that low education, male gender, economically active age, heterosexuality were associated with TB / HIV co-infection, factors that contribute to non-adherence and / or abandonment of the treatment and, therefore, increase bacterial resistance 23.
Regarding the clinical form of tuberculosis, the pulmonary form (71.83%) stood out in relation to extrapulmonary form (23.94%), considering tuberculosis the main cause of death in people living with HIV. The sequelae of pulmonary tuberculosis can cause significant pulmonary impairment and morbidity, particularly in young adults, in which the end of tuberculosis treatment may mark the beginning of a chronic respiratory disease; thus, reinforcing the need for interventions aimed at combating the disease24.
Regarding the closure of the case, most individuals were cured (69.01%) and only 7.04% abandoned treatment. Similar results were found in a study conducted in São Paulo, which found a percentage of 97.3% of cases closed due to being cured. Reflecting the expansion of access to the diagnosis and treatment of co-infection, in addition to the epidemiological surveillance actions that are developed to block the chain of transmission and prevention of disease 25.
Considering the relevance of deaths registered in SINAN, the TB-HIV association increases the likelihood of death of the affected people. Considering that, there is a change concomitant with the evolution of each infection and, consequently, of the resulting diseases, which is revealed as complications from the clinical picture, different responses to drug therapies and uncertain or unfavorable prognosis 17.
Regarding antiretroviral therapy, there was a percentage of 43.66% of individuals co-infected with TB / HIV who use this class of drugs, constituting a fundamental strategy for reducing deaths. Antiretroviral therapy reduces the mortality of HIV-infected patients by 44 to 72% during the treatment of TB 26.
It is also to be considered that the risk of tuberculosis among those who did not receive ART is about 8 times greater than those who received it, thus reinforcing the effectiveness in preventing active TB in people living with HIV / AIDS when starting ART as quickly as possible. Doing so even if there are challenges in the simultaneous use of antiretroviral and tuberculostatic drugs due to the overlap of toxicity that can lead to treatment interruption and / or the need for alternative schemes 23. In addition, the high percentage of ignored information (53.52%) about the use of antiretrovirals is also highlighted, which may be associated with the recent insertion of the item in the tuberculosis notification form, starting in 2011.
In this study, it was noted the low performance of Directly Observed Treatment (DOT), a notorious case management tool used by Nursing within the Family Health Strategy. Considering that these professionals are the first to have contact with patients establishing bonds and strengthening their relationship with the health unit, a higher performance was expected.
The DOT expresses a potent bet on public policies aimed at tackling TB, whose decentralized assistance, enables greater chances of resolving the disease. In addition, to adopt in its praxis the holistic view that not only glimpses the disease but also the comprehensiveness of each individual, potentiating the therapy and favoring the adherence to the treatment 27,28.
CONCLUSION
The results obtained indicated that, in the investigated period, 4.3% of individuals with TB had coinfection with HIV, which shows their epidemiological relevance as a comorbidity with a great impact on public health. The study explored the clinical-epidemiological characteristics of TB / HIV co-infection, which may provide evidence for future socio-demographic research on this relevant association, with a view to reducing the burden of tuberculosis in different contexts.
This study has limitations due to the use of secondary databases, when considering the accuracy and completeness of the information. However, expanding the use of SINAN data can raise awareness among professionals about the completeness of the information and therefore qualify them, bringing greater precision and reliability to the studies.
Therefore, knowing the profile of TB / HIV co-infection cases allows us to ascertain the need to adopt specific strategies according to the characteristics observed, improving the nurse's work process, which deals directly with the integrality of co-infected patients and thus, support the restructuring of public health policies and the adequate targeting of health education practices.
REFERENCIAS
1. Migliori BG, Centis R, D'ambrosio L, Silva DR, Rendon A. A colaboração internacional entre sociedades médicas é uma forma eficaz de aumentar a produção de artigos sobre tuberculose na América Latina. J Bras Pneumol [internet] 2019, 45:(2): 1-11. Disponível em: http://www.scielo.br/pdf/jbpneu/v45n2/pt_1806-3713-jbpneu-45-02-e20180420.pdf. Acesso em: 12 de outubro de 2019. [ Links ]
2. Valente BC, Angelo JR, Kawa H, Baltar VT. A tuberculose e seus fatores associados em um município da região metropolitana do Rio de Janeiro. Rev Bras Epidemiol. [internet] 2019, 22:E190027: 1-12. Disponível em: http://www.scielo.br/pdf/rbepid/v22/1980-5497-rbepid-22-e190027.pdf. Acesso em: 12 de outubro de 2019. [ Links ]
3. Santos AC, Aquino RCA. Perfil epidemiológico de pacientes imunocomprometidos com tuberculose. Rev eletrôni Estácio Recife. [internet] 2019, 5(1):1-14. Disponível em: https://reer.emnuvens.com.br/reer/article/download/181/104. Acesso em: 12 de outubro de 2019. [ Links ]
4. Ministério da Saúde. Secretaria de Vigilância em Saúde. Coordenação-Geral de Desenvolvimento da Epidemiologia em Serviços. Guia de Vigilância em Saúde: volume único [internet]. 3ª. Edição 2013 Brasília, 2019. Disponível em: http://portalarquivos.saude.gov.br/images/pdf/2017/outubro/06/Volume-Unico-2017.pdf [ Links ]
5. World Health Organzation. HIV-Associated Tuberculosis. [internet] 2018. Disponível em: https://www.who.int/hiv/topics/tb/about_tb/en/. Acesso em: 12 de outubro de 2019. [ Links ]
6. Campoy LT, Arakawa T, Andrade RLP, Ruffino-Netto A, Monroe AA, Arcêncio RA. Qualidade e gestão da atenção à coinfecção tuberculose e hiv no estado de São Paulo.Texto contexto - enferm [internet]. 2019; 28: e20180166. Disponível em: http://www.scielo.br/pdf/tce/v28/pt_1980-265X-tce-28-e20180166.pdf. Acesso em: 12 de outubro de 2019. [ Links ]
7. Ministério da Saúde. Informações de saúde: epidemiológicas e morbidade - 2015 [internet] 2016. Disponível em: http://www2.datasus.gov.br/DATASUS/index.php?area=0203. Acesso em 12 de outubro de 2019. [ Links ]
8. Santos Junior CJ, Rocha TJM, Soares VL. Aspectos clínicos e epidemiológicos da tuberculose em pacientes com HIV/aids. Medicina (Ribeirão Preto. Online) 2019; 52:(3)231-8. Disponível em: http://www.revistas.usp.br/rmrp/article/view/156246/157430. Acesso em: 12 de outubro de 2019. [ Links ]
9. Baldan SS, Ferraudo AS, Andrade M. Características clínico-epidemiológicas da coinfecção por tuberculose e HIV e sua relação com o Índice de Desenvolvimento Humano no estado do Mato Grosso do Sul, Brasil. Rev Pan-Amaz Saúde[internet]. 2017, 8:(3) 59-67. Disponível em: http://scielo.iec.gov.br/pdf/rpas/v8n3/2176-6223-rpas-8-03-00059.pdf. Acesso em 13 de outubro de 2019. [ Links ]
10. Dos Santos SLF, Barros KBNT, Torres JCN; et al. Estratégias de controle da Tuberculose no SUS: revisão sistemática dos resultados obtidos. Boletim Informativo Geum [internet] 2015, 6:(3) 50-58. Disponível em: https://revistas.ufpi.br/index.php/geum/article/view/3879. Acesso em: 13 de outubro de 2019. [ Links ]
11. Baumgarten A, Rech RS, Bulgarelli PT, Souza KR, Santos CM, Frichembruder K, Hilgert JB, Bulgarelli AF. Ações para o controle da tuberculose no Brasil: avaliação da atenção básica. Rev Bras Epidemiol [internet] 2019, 22:190031. Disponível em: http://www.scielo.br/pdf/rbepid/v22/1980-5497-rbepid-22-e190031.pdf. Acesso em 13 de outubro de 2019. [ Links ]
12. Instituto Brasileiro de Geografia e Estatística [internet] 2019. Disponível em: https://cidades.ibge.gov.br/brasil/pi/panorama. Acesso em 13 de outubro de 2019. [ Links ]
13. Brasil. Conselho Nacional de Saúde. Resolução 510/2016. Trata de pesquisas em seres humanos e atualiza a resolução 196. [Internet]. Diário Oficial da União. 12 dez. 2012 [citado em 2019 janeiro 29]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/cns/2016/res0510_07_04_2016.html [ Links ]
14. World Health Organization. Global tuberculosis report 2016. Geneva: WHO; 2016[internet] Disponível em: http://apps.who.int/iris/bitstream/. Acesso em: 15 de outubro de 2019. [ Links ]
15. Global tuberculosis report 2019. Geneva, World Health Organization, 2019.[internet] Disponivel em: https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf?ua=1. Acesso em: 15 de outubro de 2019. [ Links ]
16. Werf Marieke J van Der, Sotgiu Giovanni, Dara Masoud. Closing the gap in surveillance of tuberculosis and HIV co-infection: a European perspective on the need for clinician-public health alliances. European Respiratory Journal, [internet.] 2017, 50:(5)1701758-1701763. Disponível em: https://erJersjournals.com/content/50/5/1701758. Acesso em: 20 de outubro de 2019. [ Links ]
17. Ministério da Saúde. Secretaria de Vigilância em Saúde. Boletim Epidemiológico. v. 50, n.26 , set. 2019a. [ Links ]
18. Secretaria da Saúde do Estado do Ceará. Coordenadoria de Promoção e Proteção à Saúde, Núcleo de Vigilância Epidemiológica. Boletim Epidemiológico Tuberculose. Ceará, CE, 2018. [ Links ]
19. Castrighini CC, Reis RK, Neves LAS, Galvão MTG, Gir E. Prevalência e aspectos epidemiológicos da coinfecção HIV/tuberculose. Rev Enferm Uerj [internet] 2017,25:(2)1-6 Disponível em: http://dx.doi.org/10.12957/reuerJ2017.17432. Acesso 01 de novembro de 2019. [ Links ]
20. Ferreira DP, Souza FA, Motta MCS. Prevalência da Coinfecção Hiv/Tb em Pacientes de um Hospital de Referência na Cidade do Rio De Janeiro. Rev Fund Care Online [internet] 2019, 11:(2)358-362. Disponível em: http://www.seer.unirio.br/index.php/cuidadofundamental/article/view/6558/pdf_1. Acesso em: 28 nov 2019. [ Links ]
21. Miranda LO, et al. Aspectos epidemiológicos da coinfecção Tuberculose/HIV no Brasil: revisão integrativa. Rev Pre Infec e Saúde [internet].2017;3(3):59-70. doi: https://doi.org/10.26694/repis.v3i3.645022. Acesso em 28 novembro de 2019. [ Links ]
22. Alene KA, Viney K, Moore HC, Wagaw M, Clements ACA. Spatial patterns of tuberculosis and HIV co-infection in Ethiopia. PLoS One, 14(12):e0226127, Acesso em: 04 Dezembro de 2019. [ Links ]
23. Cui Z, Lin M, Nie S, Lan R. Risk factors associated with Tuberculosis (TB) among people living with HIV/AIDS: A pair-matched case-control study in Guangxi, China. PLoS One.[internet] 2017;12(3):e0173976. Disponível em: doi:10.1371/journal.pone.0173976. Acesso em 04 de dezembro de 2019. [ Links ]
24. Tiberi S, et al. Tratamento da tuberculose grave e suas sequelas: da terapia intensiva à cirurgia e reabilitação. J bras pneumol. [Internet]. 2019 [cited 2020 Feb 05] ; 45( 2 ): e20180324. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1806-37132019000200500&lng=en. Disponível em: http://dx.doi.org/10.1590/1806-3713/e20180324. [ Links ]
25. Alcalde GFG et al. Perfil epidemiológico de tuberculose em pacientes portadores de hiv. Rev Preven de Infecção e Saúde.[internet] 2018, 4: 1-12. Disponível em: http://dx.doi.org/10.26694/repis.v4i0.7519 [ Links ]
26. Ministério da Saúde. Secretaria de Vigilância em Saúde. Boletim Epidemiológico. v. 50, n.26 , set. 2019a. [ Links ]
27. Coelho LE et al. O tratamento da coinfecção HIV-TB. The Brazilian Journal Of Infectious Diseases [internet] 2016, 2: (5)134-148. Disponível em: http://www.bjid.org.br/en-o-tratamento-da-coinf [ Links ]
28. Junges JR, Burille A, Tedesco J Tratamento Diretamente Observado da tuberculose: análise crítica da descentralização. Interface (Botucatu) [Internet]. 2020 [cited 2020 Feb 05] ; 24: e190160. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1414-32832020000100206&lng=en. Epub Oct 24, 2019. http://dx.doi.org/10.1590/interface.190160 [ Links ]
Received: February 13, 2020; Accepted: March 30, 2020











 texto em
texto em 




