My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.19 n.60 Murcia Oct. 2020 Epub Dec 21, 2020
https://dx.doi.org/10.6018/eglobal.386951
Originals
Patient safety culture from the perspective of the nursing team in a public maternity hospital
1Nurse. Specialist in Obstetric Nursing - Federal University of Piauí - UFPI. Teresina, PI Brazil. paulallima00@gmail.com
2PhD Professor at the Federal University of Piauí - UFPI. Teresina, PI, Brazil.
3Master in Nursing - Federal University of Piauí - UFPI. Teresina, PI, Brazil.
Objective:
To evaluate the dimensions of patient safety culture from the perspective of the nursing team in a public maternity hospital.
Method:
Cross-sectional study conducted in a public maternity hospital with 69 nursing professionals, from June to August 2017, through the application of the Hospital Survey on Patient Safety Culture.
Results:
The average of positive scores ranged from 33.0% to 69.6%, and the best evaluations were made in the following dimensions: organizational learning, teamwork between units, and non-punitive responses to the error. The most fragile evaluations were made in: internal transfers and shift reports, in addition to the frequency of reported events.
Conclusion:
The study pointed to a weak safety culture in all areas, and indicated that planning targeted strategies in order to achieve quality safety culture for the mother/child binomial is important.
Keywords: Culture; Patient safety; Maternity hospitals; Nursing Team
INTRODUCTION
Patient safety has become the focus of researchers worldwide, in view of the magnitude of the problem, and has assumed an essential dimension for health quality in the most diverse areas. In this context, reflections on actions aimed at patient safety have gained space. The World Alliance on Patient Safety was created after the phenomenon was recognized globally as a serious public health problem1. Thus, carrying out health education actions on patient safety and risk management in obstetric and neonatal care is of great importance2.
Adverse events (AE) related to assistance to women during the puerperal/pregnancy period are relatively common and, often, preventable. Therefore, AE are understood as damages arising from errors or failures in the assistance provided by health professionals, whether intentionally or not, and which can generate permanent or temporary harm, incapacitate patients or even lead to death3.
Thus, patient safety is defined as the reduction of risk of unnecessary harm associated with health care to an acceptable minimum5. Thus, authors emphasize the shared responsibility for implementing strategies aimed at correcting the weaknesses found, in favor of qualified, effective, efficient, and safe care1. Still, a critical analysis of the weaknesses of the patient safety process is recommended so as to seek strategies for the adoption of a positive safety culture, benefiting patients, family members and professionals, and especially maternal and child health4.
In this sense, a study carried out in maternity hospitals of seven hospitals in the city of Ilam, Iran, showed a receptive attitude of the team towards patient safety culture, but they were still far from achieving a safety culture of excellence. Only 59.1% of the participants reported a reasonable level of perception of general safety5. On the other hand, a study carried out in the South African region showed important reductions in maternal mortality after the implementation of the safe surgery checklist, modified for maternity care6.
At the national level, a study conducted in a philanthropic maternity hospital in the city of Lagarto, Sergipe, showed a positive patient safety culture in the maternity hospital, with the need for minor adjustments in the organizational and managerial commitment of the service.2 Another survey to assess the perception of nursing professionals working in a private hospital about the safety climate found a distance between the nursing management of the unit and the hospital and the workers who worked in loco. An expanded look both in the unit and in the hospital was thus necessary 7.
Therefore, it is fundamental to focus on improving the quality of systems that strategically invest in resources to achieve the fourfold objective. In other words, it is necessary to improve the health of people who seek health care, lowering the costs for the system, improving patient care and promoting an engaged and productive workforce in order to redirect health services towards promotion of population health8.
Thus, considering the importance of the performance of the Nursing team on patient safety, based on the knowledge acquired and experiences with challenges that influence safety culture, and also the way these factors can facilitate the development and implementation of better strategies, some authors point out several challenges hindering an effective and positive safety culture in healthcare organizations.
Thus, in order to meet international standards, health managers must employ modern management methods to overcome the challenges faced by the institutionalization of safety culture and to make a difference in the health system9.
In view of these considerations, studying safety culture in maternity hospitals is essential to ensure the provision of care free from AE, or at least with AE at acceptable levels. It also allows knowing the factors involved in the teamwork process, which sometimes represent gaps in theory and practice so as to strengthen the care by providing it with the best scientific evidence.
As a result, the encouragement and creation of safety culture in maternity hospitals, which take into account the local reality and the skills of the professionals involved, can enable action strategies for the development of attitudes, skills and knowledge to promote patient safety.
Based on the above, the objective of this study was to assess the dimensions of the patient safety culture from the perspective of the Nursing team in a public maternity hospital.
METHODS
The methodology adopted in this work was a cross-sectional study with quantitative approach in a public maternity hospital, in the Northeast of Brazil, responsible for 63% of births that occurred in the capital of Piauí, Teresina 10. Data collection took place from June to August 2017.
Therefore, the following inclusion criteria were adopted: being a professional of the nursing team; working in direct assistance to patients admitted to the normal delivery center, superior obstetric center, and surgical center; being employed for at least three months, with effective bond or not. Professionals who were on sick leave, maternity leave, vacation and/or absent for other reasons were excluded, as well as those who were making scheduled replacements and who did not belong to the sector under study.
Participants were recruited using the non-probabilistic sampling technique for convenience. Thus, all eligible professionals had the opportunity to participate in the study. Therefore, only 69 among 74 professionals accepted to participate, which corresponds to 31 nurses, 37 nursing technicians and 1 nursing assistant.
Data collection took place by applying a version of the Hospital Survey on Patient Safety Culture (HSOPSC)11, translated and validated for Brazil, prepared by the Agency for Healthcare Research and Quality (AHRQ). 12 Thus, the instrument contemplated sociodemographic (sex, age, educational level) and professional aspects (time of work in the hospital, time of work in the current area, weekly workload).
In this context, the questionnaire also covered the variables of dimension of safety culture, which included: variables within the unit (teamwork in the unit, expectations and actions to promote patient safety by the supervisor/manager, organizational learning and continuous improvement, feedback and communication of errors, openness to communication, personnel and non-punitive responses to errors); variables within the hospital organization (support of hospital management for patient safety, teamwork between hospital units, internal transfers and shift reports); and outcome variables (general perception of patient safety, frequency of reported events).
Two additional questions were included: a global assessment of patient safety and the number of prevalence of AE reported by professionals in the last 12 months. In this study, the proportion of positive responses in each HSOPSC category was adopted as primary outcome.
The collection took place in a reserved and adequate space, after informed consent by the participants. Data were collected in the participants' work shift. In order to guarantee greater adherence of participants, before data collection, the managers communicated the immediate heads of the unit about the purpose of the study, as well as the importance of their participation in the process. Also, to ensure greater reliability of the information provided, a white envelope without an identifier was delivered together with the questionnaire to be later deposited in a sealed box.
In this study, HSOPS responses were coded using a five-point Likert scale of agreement (strongly disagree, disagree, neither agree nor disagree, agree, strongly agree) and frequency (never, almost never, sometimes, almost always, always). The results were evaluated based on the performance of each item and of the dimension.
After collection, the data were submitted to double entry, in which two people tabulated them in the Microsoft Excel software. Then, the results were crossed in order to reduce typing errors. After that, they were exported to the IBMR SPSS 21.0 and, then, the percentage frequency of each dimension was calculated and classified as recommended by AHRQ: items and dimensions with 75% of positivity were used as strengths, and those with less of 50% of positivity as fragilities.12 Inferential analyses used descriptive statistics with frequency tables and means for the percentages of positive scores of the dimensions.
This study was approved by the Research Ethics Committee of the Federal University of Piauí, with opinion nº 1,971,732.
RESULTS
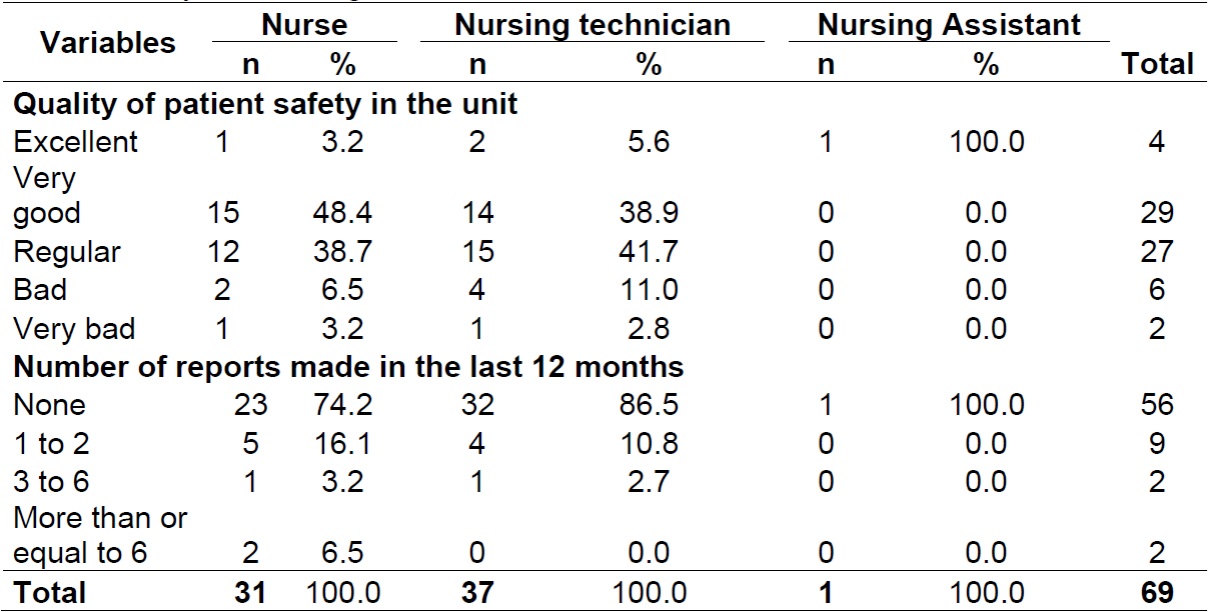
Of the 74 nursing professionals eligible for the study, 69 agreed to participate. There was a predominance of nursing technicians 37 (57.0%), 65 (94.2%) of whom were female, and the age ranged from 20 to 50 years; 23 (67.9%) were aged between 31 and 40 years. Regarding the level of education, 24 (77.4%) of the nurses had graduate level Lato sensu and 18 (48.6%) of the nursing technicians had complete high school (Table 1).
Table 1. Sociodemographic and professional characteristics of the nursing team in a public maternity hospital (N = 69). Teresina, PI, Brazil.
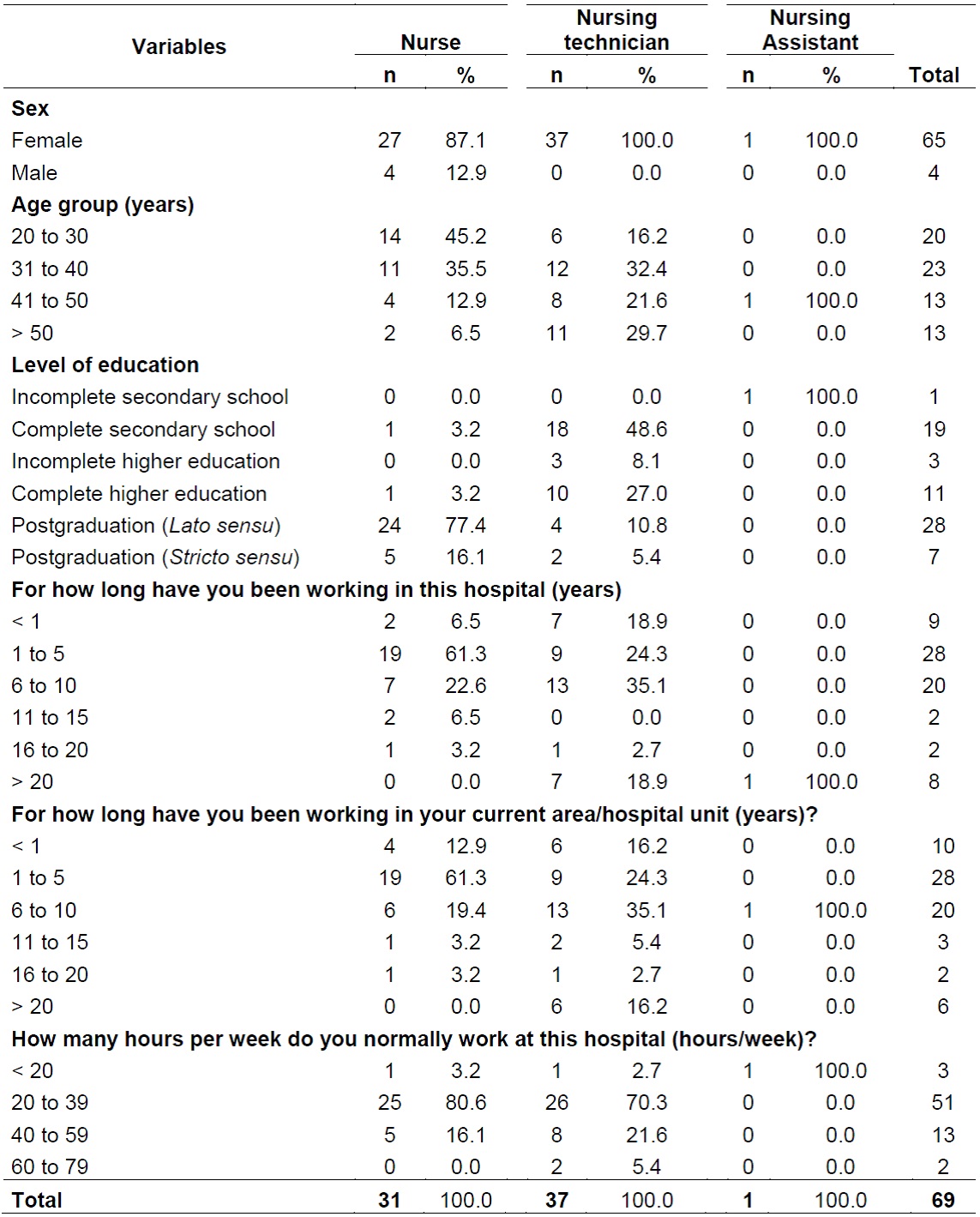
Source: prepared by the authors
Regarding professional aspects, the majority of the participants had been working at the hospital from 1 to 5 years, of these, 19 (61.3%) were nurses. The predominant weekly workload was 20 to 39 hours for both nurses, 25 (80.6%), and nursing technicians, 26 (70.3%) (Table 2).
Regarding the average positive percentage scores of the patient safety culture dimensions, the average percentage of positive responses ranged from 33.0% for the dimension internal transfers and shift reports to 69.6% for the dimension organizational learning (Figure 1).
In this study, most of the dimensions assessed were classified as neutral areas, since the items or dimensions in which the percentage of positive responses was greater than 50% and smaller than 75% ranged from 51.1% to 69.6%, corresponding to 58.4% (Figure 1).
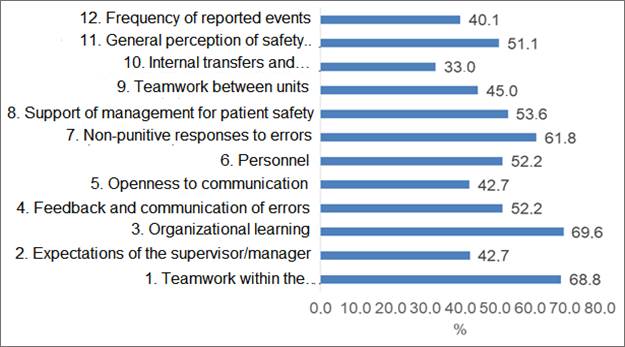
Source: prepared by the authors
Figure 1. Average of positive percentage scores of the patient safety culture dimensions (N = 69). Teresina, PI, Brazil.
Regarding the level of patient safety, 48.8% of the nurses considered it to be very good and 41.7% of the nursing technicians assessed it as regular. As for the number of events reported in the last 12 months, 96.5% of the nursing technicians did not report any events and only 6.5% of the nurses reported six or more events (Table 3).
DISCUSSION
The data collected in this study showed a safety culture in the maternal care environment with potential for improvement in all areas, particularly on internal transfers and shift reports. Even so, none of the dimensions reached the recommended percentage above 75.0%. These results are in line with other national studies13,14.
In the international context, a research carried out in Australian maternity hospitals showed that assessing safety culture is complex and that achieving satisfactory responses involves local engagement, commitment and the capacity of the place of study5.
However, it is emphasized that the absence of strength areas may be related to the recent concern with the theme and time of implementation of Patient Safety Centers, which were structured in health services mainly in 2013, after publication of the National Patient Safety Program15.
In this perspective, there is a need for ensuring care during labor and delivery with better patient safety and greater emphasis on weak points, as well as for encouraging strong points in care, in order to guarantee healthy delivery and birth.
Regarding the dimension “internal transfers and shift reports”, significant negative responses were noteworthy. In this perspective, it is worth noting that, according to the Ministry of Health, the shift reports between health teams are considered, in the current context, essential tools for the continuity of quality care, as well as for preventing failures and errors3.
In this context, there is an urgent need to review this dimension because it presents a fragile aspect within the institution. In other words, loss of important information and procedures can occur and patient safety can be consequently compromised.
Some authors stress that although practical strategies to create a safety culture may seem simple, their implementation is not precisely easy. There are several challenges to overcome in order to cultivate an effective and positive safety culture in healthcare organizations9 .
To keep up with international standards, health managers must employ modern management methods to overcome the challenges faced by the institutionalization of the safety culture and to make a difference in the health system9. In this perspective, the search for safety culture requires proactive attitudes from all actors involved and the identification of gaps in care provision both at a personal and collective level, in order to overcome personal and organizational challenges.
Although the dimensions “organizational learning” and “teamwork” did not reach the desired minimal percentage of 75% of positive responses, they deserve to be highlighted because they presented the best percentage of positive responses for patient safety.
A survey conducted at three general hospitals in Arabia to assess the current safety culture is in line with the present findings; nurses perceived only two areas of patient safety as strengths: teamwork within the units and organizational learning - continuous improvement.16 Thus, despite the difficulties and barriers, professionals sought to work as a team in the three sectors of direct care for delivery and birth.
In this context, it is emphasized that integrative and cooperative teamwork between nursing professionals, as well as mutual respect for individual limits and time of each person during activities are fundamental to subsidize safe and qualified nursing care, with a high degree of professional satisfaction and consequent reduced mortality rates17. Thus, as health professionals improve the idea of collective responsibility during health care, they will advance towards satisfactory patient safety culture, with fewer failures and errors18.
A survey that assessed the opinion of nurses and midwives working in clinical departments and providing services in obstetrics, gynecology and neonatology, about patient safety culture and about exploring potential predictors for general perception of safety concluded that, in the hospital environment, the critical domains in health units that provide services in the abovementioned areas were: teamwork in hospital units and at the unit level, open communication, teamwork within units, and non-punitive response to personal errors. The other domains were seen with potential for improvement19.
In this study, there was a predominance of females. This agrees with another research carried out in 2015 about the profile of nursing professionals in Brazil. Through this study, it was possible to observe that, in the national scenario, 89% of the professionals were female and only 10.9%, male.20 Still, young adults and those with workloads over 20 hours prevailed, a fact evidenced also in another study.12
Regarding the professionals' assessment of the level of patient safety, the vast majority rated it as very good. A research carried out with 1,229 clinical and non-clinical employees from all public hospitals in the West Bank revealed that the majority of participants (70.5%) rated the level of patient safety in their units/hospitals as excellent/very good21.
In Brazil, authors identified that most professionals in Neonatal Intensive Care Units evaluated patient safety as regular (45%), very good (38%), and excellent (3%).22 Even though the positive coefficients were below the expected and desired for patient safety culture in the different areas, the Nursing team made a positive evaluation of the care provided with a certain degree of safety, thus reinforcing the need for improvement of the degree of safety in the evaluated dimensions.
With regard to reports of AE, there was low communication by the team as a whole. It is worth mentioning that international findings go against this study.22 Therefore, there is an urgent need for professionals of the nursing team to understand AE, as well as to adopt a non-punitive culture in face of the installed AE. This will contribute to a greater number of reports by professionals and, consequently, to the adequate management of the occurrences23.
It is necessary to train nurses and supervisors to improve the general patient safety culture and implement additional actions necessary to improve areas such as reporting AE and adopting non-punitive responses to errors24.
The voice of employees plays an important role in organizational intelligence about risks to patient safety, directly influencing the quality of care25. In this perspective, ombudsman services are suggested to communicate AE within health care institutions, in order to guarantee the anonymity and confidentiality of the reported events, in order to generate a safe environment for assertive communication.
Thus, it is clear that, given the context analyzed, safety culture in the sectors of childbirth assistance is still in the process of development, with no areas of strength. In this sense, it is suggested that specific strategies be drawn based on the dimensions identified with the greater number of weaknesses. In this regard, authors emphasize the importance of continuing education in health to encourage the diversification of strategies to share knowledge and experiences in the world of work14.
In this context, healthcare organizations should strive to improve their safety culture, creating environments where healthcare professionals trust each other, work collaboratively and share responsibility for patient safety and quality of care26. Measuring the current culture and understanding the gaps in practice, as well as creating strategies to overcome some of the main challenges for success in each of these areas will result in sustainable changes27.
It is important to note that this study has the limitation of covering a local and specific reality, and this prevents the generalization of the findings. It should also be noted that the universe researched corresponds to a single professional category, and cannot represent the other professionals involved in direct care to women in labor and childbirth. It is possible, therefore, that some of the information provided may have generated response bias, as it was the care provided to patients that was assessed.
CONCLUSION
In the present study, the patient safety culture in a maternity ward was assessed, and it was perceived by the nursing team as presenting no one area of strength in all areas and with possibilities for improvement in all dimensions, especially among those with low evaluation scores, particularly internal transfers and shift reports, as well as frequency of reported events. It was also possible to show that the safety culture is in the process of maturation, with no areas of strength, and thus requiring better development.
Thus, the importance of commitment on the part of professionals and managers in the search for patient safety is emphasized. Moreover, further research on the topic is necessary to incite more discussions and to achieve a strong culture of safety, with more qualified assistance and lower probability of AE within hospital institutions assisting women in labor and childbirth, making it possible to improve the quality of care to the mother/child binomial, based on the main scientific evidence.
REFERENCIAS
1. Silva ACAB, Rosa DOS. Patient safety culture in hospital organization. Cogitare Enferm 2016;21:1-10. [ Links ]
2. Santos FJ, Nascimento HM, Santos JMJ, Cunha JO, Santos JCS, Pena JÁ. Cultura de segurança do paciente em uma maternidade de risco habitual. ABCS Health Sci. 2019; 44(1):52-57 [ Links ]
3. Ministério da Saúde (BR). Agência Nacional de Vigilância Sanitária. Documento de referência para o Programa Nacional de Segurança do Paciente. 2014. [ Links ]
4. Notaro KAM, Manzo BF, Corrêa AR, Tomazoni A, Rocha PK. Safety culture of multidisciplinary teams from neonatal intensive care units of public hospitals. Rev Latino-Am Enfermagem. 2019;27:e3167. [ Links ]
5. Nahid A. et al. Safety culture in the maternity unit of hospitals in Ilam province, Iran: a census survey using HSOPSC tool. Pan Afr Med J 2017;27:268. [ Links ]
6. Naidoo, M. et al. The impact of a modified World Health Organization surgical safety checklist on maternal outcomes in a South African setting: A stratified cluster-randomised controlled trial. S Afr Med J 2017; 107(3): 248-257. [ Links ]
7. Golle L, Ciotti D, Herr GEG, et al. Cultura de segurança do paciente em hospital privado J res: fundAm care. 2018; 10(1): 85-89. [ Links ]
8. Kryzanowski J, Bloomquist CD, Dunn-Pierce T, Murphy L, Clarke S, Neudorf C. Quality improvement as a population health promotion opportunity to reorient the healthcare system. Can J Public Health. 2019; 110(1):58-61. [ Links ]
9. Farokhzadian J, Dehghan Nayeri N, Borhani F. The long way ahead to achieve an effective patient safety culture: challenges perceived by nurses. BMC Health Serv res 2018;18(1):654. [ Links ]
10. Secretaria de Saúde do Estado do Piauí (BR). Portal da saúde [Internet]. 2014; Disponível em: http://www.saude.pi.gov.br/ [ Links ]
11. Reis CT, Laguardia J, Vasconcelos AG, Martins M. Reliability and validity of the Brazilian version of the Hospital Survey on Patient Safety Culture (HSOPSC): a pilot study. Cad Saúde Pública [Internet]. 2016; 32(11):e00115614. [ Links ]
Agency for Healthcare Research and Quality (AHRQ). Hospital survey on patient safety culture [Internet]. 2016 [citado em 2018 nov 05];15(16):0049. [ Links ]
12. Minuzzi AP, Salum NC, Locks MOH, Amante LN, Matos E. Contributions of healthcare staff to promote patient safety in intensive care. Esc Anna Nery. 2016;20(1):121-9. [ Links ]
13. Galvão TF, Lopes MCC, Oliva CCC, Araújo MEA, Silva MT. Patient safety culture in a university hospital. Rev Latino- Am Enfermagem. 2018;26:e3014. [ Links ]
14. Ministério da Saúde (BR). Agência Nacional de Vigilância Sanitária. Documento de referência para o Programa Nacional de Segurança do Paciente. Brasília: Ministério da Saúde; 2014. [ Links ]
15. Ministério da Saúde (BR). Ministério da Saúde. Portaria nº 529, de 1 de abril de 2013: institui a Política Nacional de Segurança do Paciente (PNSP). Brasília: Ministério da Saúde; 2013. [ Links ]
16. Alquwez N, Cruz JP, Almoghairi AM, Al-Otaibi RS, Almutairi KO, Alicante JG et al. Nurses' Perceptions of Patient Safety Culture in Three Hospitals in Saudi Arabia. J Nurs Scholarsh [Internet]. 2018 [citado em 2018 nov 05];50(4):422-431. [ Links ]
17. Oliveira RM, Leitão IMTA, Aguiar LL, Oliveira ACS, Gazos DM, Silva LMS, et al. Evaluating the intervening factors in patient safety: focusing on hospital nursing staff. Rev Esc Enferm USP. 2015 ;49(1):104-13. [ Links ]
18. Wegner W, Silva CS, Kantorski KJC, Predebon CM, Sanches MO, Pedro ENR. Education for culture of patient safety: implications to professional training. Esc Anna Nery. 2016;20(3):e20160068. [ Links ]
19. Ribeliene J, Blazeviciene A, Nadisauskiene RJ, Tameliene R, Kudreviciene A, Nedzelskiene I et al. Patient safety culture in obstetrics and gynecology and neonatology units: the nurses' and the midwives' opinion. J Matern Fetal Neonatal Med 2018;22:1-7. [ Links ]
20. Conselho Federal de Enfermagem (COFEN). Pesquisa perfil da Enfermagem no Brasil. 2016. [ Links ]
21. Hamdan M, Saleem AA. Changes in Patient Safety Culture in Palestinian Public Hospitals: Impact of Quality and Patient Safety Initiatives and Programs. J Patient Saf. 2018;14(3):e67-e73. [ Links ]
22. Tomazoni A, Rocha PK, Kusahara DM, Souza AIJ, Macedo TR. Evaluation of the patient safety culture in neonatal intensive care. Texto Contexto Enferm [Internet]. 2015; 24(1):161-9. [ Links ]
23. Duarte SCM, et al.Eventos adversos e segurança na assistência de enfermagem. Rev Bras Enferm 2015;68(1):144-54. [ Links ]
24. Amiri M, Khademian Z, Nikandish R. The effect of nurse empowerment educational program on patient safety culture: a randomized controlled trial. BMC Med Educ. 2018;18(1):158. [ Links ]
25. Dixon-Woods M, Campbell A, Martin G, Willars J, Tarrant C, Aveling EL et al. Improving Employee Voice About Transgressive or Disruptive Behavior: A Case Study. Acad Med 2018; Sep 11. [ Links ]
26. Lee SE, Vincent C, Dahinten VS, Scott LD, Park CG, Dunn Lopez K. Effects of Individual Nurse and Hospital Characteristics on Patient Adverse Events and Quality of Care: A Multilevel Analysis. J Nurs Scholarsh. 2018;50(4):432-440. [ Links ]
27. Black JM, Salsbury S, Vollman KM. Changing the Perceptions of a Culture of Safety for the Patient and the Caregiver: Integrating Improvement Initiatives to Create Sustainable Change. Crit Care Nurs Q. 2018;41(3):226-239. [ Links ]
Received: July 03, 2019; Accepted: January 17, 2020











 text in
text in