My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.20 n.63 Murcia Jul. 2021 Epub Aug 02, 2021
https://dx.doi.org/10.6018/eglobal.450481
Originals
Notification of incidents related to health care in a teaching hospital
1 Hospital Universitario Profesor Edgard Santos, Universidad Federal de Bahia. Salvador, Bahia, Brasil. valdenirenf@gmail.com
Method:
A quantitative research carried out based on notifications of incidents carried out between 2016 and 2018. The data were processed in STATA version 12.
Results:
The incidence of adverse events was 3.82 per 100 patient-days. The adult hospitalization units were the main notifiers, 57.20%; adult patients, 52.75%; females, 52.9%; blacks, 80.01%; singles, 47.62%; with low or no schooling, 50.91%, were the main ones. The nurses were the main notifiers, 80.38%. Phlebitis, 27.05%; surgeries, 19.20%; and falls, 17.27%, were the most reported incidents, whose damage was classified as mild in 91.52%, but there were three deaths in the period.
Conclusion:
The analysis of incidents allows us to highlight the importance of notifications for the planning and implementation of measures that can contribute to the strengthening of the patient safety culture.
Key words: Notification; Adverse events; Patient safety; Teaching hospitals; Nursing
INTRODUCTION
Patient safety is a global concern, affecting all health systems in both developed and developing countries1. In health organizations, such as complex organizations whose zero risk is impossible to obtain, the existence of mechanisms for managing incidents related to health care and minimizing their impacts contribute to the development of reliable/reliable systems2. As a strategy to improve care and care provided, issues related to patient safety have been gaining prominence. Globally, the World Health Organization (WHO) launched, in 2004, the World Alliance for Patient Safety to foster discussions on the subject and to stimulate the development of actions for patient safety and the reduction of adverse events (AE)3.
The approach to patient safety has been emphasized as a pressing need, according to an editorial in The Lancet “Patient safety is not a luxury”. This publication reinforces the importance of structuring systems and environments in health services capable of promoting reduction of errors4. The WHO infers that, in the world, there is an avoidable adverse event for every 10 patients during the use of health services5. An estimated 4.2 million patients worldwide suffer damage or death annually due to unsafe care practices or errors. The annual cost derived from these practices is estimated at US$ 42 billion, consuming about 1% of global health expenditures1.
Since safety risks in the care process are ineviTable, although partly prevenTable1,5, the role of reporting incidents related to health care, whose primary purpose is to communicate security threats, such as near failures, incidents or adverse events, and the possibility of supporting learning from experience, stands out. A good internal notification system can be used to identify threats to patient safety and ensure that everyone involved is aware of such threats. Thus, notifications are important for monitoring progress in error prevention, to allow the monitoring of safe practices and to improve patient safety1,6-8. Notification systems allow the collection of information, analysis and dissemination of lessons learned8.
The information obtained from the notifications are determinant for decision makers, responsible for the development and management of safety policies, health professionals and patients9, and may support the implementation of organizational improvements6,10. Decision-making based on data on incident notifications, then, should be a commitment made by the agents involved in public policies for patient safety2.
Given the importance attributed to the notifications of incidents related to health care for patient safety, it was decided to carry out this study, which aims to analyze incidents related to health care in a teaching hospital.
METHODOLOGY
This is a descriptive and exploratory research with a quantitative approach, carried out from secondary data from notifications of incidents related to health care, referring to the years 2016, 2017 and 2018.
The research was carried out in a large teaching hospital (TH), belonging to the Unified Health System (SUS), member of the Brazilian Hospital Services Company network, located in Salvador, Bahia, Brazil. It is an integral hospital of the Sentinel Hospitals Network of the National Health Surveillance Agency (ANVISA), whose primary objective is to be an active observatory of the performance and safety of products used in health. As such, it collaborates with the notification of adverse events and technical complaints related to products under post-use or post-marketing surveillance in the National Health Surveillance System (NOTIVISA). In addition, it has a structured Patient Safety Center with implementation of the basic patient safety protocols recommended by ANVISA, in addition to monitoring protocols and incidents, and continuing education activities in patient safety.
The hospital has a Hospital Surveillance application (VIGIHOSP) implemented in mid-2015 to receive notifications of incidents and technical complaints related to health care. Since then, it has received notifications from all sectors of the hospital being accessible to all professionals.
Data were collected from August 2019 to March 2020 by a research initiation fellow duly trained and supervised by the researchers responsible. As VIGIHOSP was implemented in the hospital in mid-2015, the research period was determined the years 2016 to 2018, the latter being the full year prior to the preparation of the project.
All reports of incidents related to health care performed at VIGIHOSP during the research period were included. Variables related to patients and incidents were collected, such as: age, race, gender, marital status, level of education, origin, turn of occurrence, professional category of the notifier, nature of the notification (anonymous or identified); date and place of occurrence; type and characteristics of the incident; and degree of damage (mild, moderate, severe, death).
The classification of the degree of damage according to the World Health Organization (WHO)11) was adopted, in: 1) none - there was no consequence for the patient; 2) mild - the patient presented mild symptoms, minimal or intermediate short-term damage without intervention or with a minimal intervention (small treatment or observation); 3) moderate - the patient required intervention, such as the performance of additional procedure or additional therapy, prolongation of hospitalization, loss of function, permanent or long-term damage; 4) severe - necessary intervention to save life, major medical-surgical intervention or caused major permanent or long-term damage; fetal disturbance/risk or congenital anomaly; and 5) death. It should be noted that an incident related to health care is an event or circumstance that could result or that resulted in unnecessary damage to the patient. When such an incident results in damage to the patient, it is called an adverse event11.
The data were analyzed using STATA statistical software version 12 by applying descriptive statistics. The incidence rate of incidents related to health care was calculated by the relationship between the number of incidents reported during the study period, divided by the total number of patients admitted in the same period x 100.
The project complied with the ethical principles of research involving human beings and met the recommendations of Resolution 466/2012 of the National Health Council. The research protocol was approved by a Research Ethics Committee through CAAE NO 09076619.2.0000.0049.
RESULTS
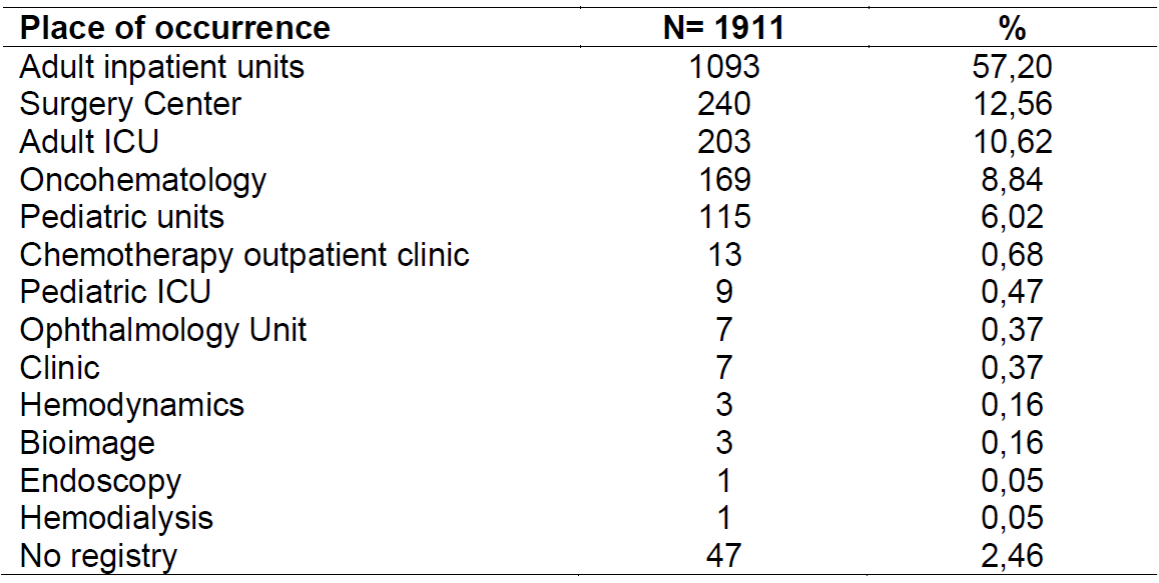
During the research period, 1911 incidents were reported in HE, of which 259 occurred in 2016, 617 in 2017 and 1035 in 2018. The overall incidence of notifications during the study period was 7.94 per 100 hospitalized-day patients, 3.46 in 2016; 7.91 in 2017 and 11.78 in 2018. The main notifying units were adult hospitalization units, with 1093 (57.20%) notifications; operating room, which performed 240 (12.56%) notifications; Adult Intensive Care Unit (ICU), with 203 (10.62%) notifications; and the oncohematology unit, with 169 (8.84%). (Table 1)
Table 1: Characterization of reported health care incidents, according to the place of occurrence. Salvador Bahia Brazil, 2020.
The sociodemographic characterization of patients who have reported incidents points to mostly adult people, 1,008 (52.75%) and old women, 649 (33.96%); female, 995 (52.9%); self-declared as black, 1529 (80.01%); single, 910 (47.62%); with low or no schooling, 973 (50.91%); and coming from Salvador - Bahia, 1030 (53.90%). (Table 2)
Table 2: Sociodemographic characterization of patients with notification of health care-related incidents. Salvador, Bahia, Brazil, 2020.

Regarding the characterization of reported incidents (Table 3), the majority occurred during the hospitalization of the individual in the TH, 1827 (95.70%); in the morning shift, 414 (21.66%); with identified notification, 1446 (75.67%); with the nurse professional being the main notifier, 1536 (80.38%). We highlight the high proportion of lack of registration in the incident shift, 815 (42.65%).
Regarding the type of incident (Table 4), the highest proportions of notifications were related to phlebitis, 517 (27.05%); surgeries, 367 (19.20%); falls, 330 (17.27%); problems related to the drug chain, 233 (12.19%); skin lesions, 181 (9.47%); and problems with patient identification, 72 (3.77%).
Regarding damage, 920 (48.14%) of the incidents were classified as adverse events, with repercussions on the health of individuals. The incidence of adverse events was 3.82 per 100 hospitalized patients/day. The incidents that presented the highest proportion of damage to health were phlebitis, skin lesions, medical-hospital articles and equipment, catheter loss, blood and/or blood components, accidental extubation and diagnostic error, with damage to patients in 100% of cases, being therefore classified as adverse events; nutritional therapy, in 18 (56.26%); falls, in 43 (13.03%); and problems related to the drug chain, with 30 (12.88%) cases.
Regarding the degree of damage resulting from the adverse event (Table 5), the majority had mild damage, 842 (91.52%); 64 (6.96%) caused moderate damage; and three (0.32%) culminated in the death of the individual. The events that presented the highest proportions of damage considered moderate or severe were surgery (36.84%), medical-hospital equipment (25%), medications (20%), accidental extubation (12.50%), falls (11.63%) and skin lesion (8.84%).
DISCUSSION
During the study period, the overall incidence of reports of incidents related to health care was 7.94 per 100 patient-days. Among the reported incidents, 48.14% caused some harm to patients and were thus classified as adverse events. The incidence of adverse events was 3.82 per 100 hospitalized patients. A study conducted in a teaching hospital in Minas Gerais based on spontaneous notifications in an electronic notification system, over a period of four years, found a similar result, with a prevalence of 33.8 incidents per 1,000 hospitalizations12.
These data differ from other Brazilian and international studies regarding the percentage of adverse events among the incidents studied. A study conducted in three teaching hospitals in Rio de Janeiro - RJ showed an incidence of adverse events of 7.6%, with a proportion of 0.8 AE per 100 patient-days13. Another study identified a percentage of 7.9%(14); and 8.2%, and 24% of patients suffered between two and five different events15 In other publications, there is still a higher percentage of adverse events in specialized units, such as ICU, whose incidence was 32.4%, with an average of 2.8 adverse events per 100 patient-days16 and among hospitalized elderly, with a prevalence of 58.8% and an average of 2.04 events per 100 hospitalizations17. At the international level, it is noteworthy that in Kenya, a prevalence of 1.4% of adverse events was identified, based on a review of medical records18; in Canada, a study showed a percentage of AS of 12.5%19 and in Portugal, the incidence of AE was estimated at 15.3%20.
It is necessary to recognize that several factors influence the occurrence of AE, such as quantity and quality of available materials and equipment, structural conditions of the service and access to new technologies14; undersizing nursing staff, training and qualification14, professional experience time shorter than five years, for lighter incidents and greater than five years for more severe damage1. The implementation of security policies, on the other hand, favors the identification and notification of incidents, steps necessary to strengthen the security culture.
A study conducted in a university hospital in southern Brazil that has adequate staff dimensioning identified that the occurrence of adverse events was higher than in other hospitals that also have dimensioning within the recommended legislation, thus, it is evident that other factors such as inadequate preparation for surgical procedures and diagnoses, inadequate transportation, insufficient team training also influence the occurrence of adverse events14.
It was observed that there was an increase in the number of notifications over the years analyzed. In other studies, the same growth trend was also observed with years1)(6)(7)(12 It is believed that this increase is due to the dissemination of information about the application used to receive notifications, the implementation of patient safety protocols and the performance of educational activities with the professionals of the organization, when the importance and stimulation of the practice of notification is emphasized. In-service education is also highlighted by other authors who found an increase in the number of notifications correlated to monthly training6.
In the on-screen study, the main origins of the notifications were the adult hospitalization units (57.20%); surgical center (12.56%); Adult ICU (10.62%); and the oncohematology unit (8.84%). These data confirm a trend pointed out in the literature regarding the places with higher occurrences of incidents related to health care1)(6)(12)(21. The higher incidence in inpatient units may be related to the greater number of beds and, consequently, to the greater number of hospitalized patients. It is also considered the profile of severity, complexity, hemodynamic instability, use of a greater number of medications and greater submission to diagnostic and therapeutic procedures of patients16, as is the case of the operating room, ICU and oncohematology unit as factors that predispose patients to suffer safety incidents.
The characteristics of the people who suffered some incidents indicate that the elderly group was the second largest (33.96%), behind adults. There was also a highlight for females; self-declared as black, 80.01%; single women, 47.62%; and with low or no schooling, 50.91%. Other studies also show that adults and the elderly make up the age group that suffers the most incidents related to health care1)(12)(15)(16)(22. There is also a predominance of females14,15) and with only elementary school14. The percentage of self-declaration as belonging to the black race can be justified by the fact that about 80% of the population of the city of Salvador - Bahia is Afrodescendant, the most vulnerable population and that most of them use SUS services, thus coinciding with the origin of hospitalized patients who suffered incidents.
Among the reported incidents, 95.7% occurred during hospitalization, which can be justified by the longer length of the patient's stay in the service and thus be more exposed to risk. It is noteworthy that 40.13% of the records were incidents that occurred during the day, mainly in the morning, and can be explained by the greater number of professionals in the services, greater surveillance and greater possibility of identification and notification of incidents. In a study conducted in an ICU of a hospital in São Paulo - SP, the shift of the most reported occurrence was the night (36.8%) and there was a close distribution between the morning and afternoon shifts, but 77.4% of the notifications did not inform the shift of the occurrence, whereas in this research this percentage was 42.65%12. At night, there are fewer nursing professionals and the multidisciplinary team in the service, however, the distribution of incidents in this shift was lower. It is understood, however, that it is not always possible to identify the turn of the occurrence of the incident, as is the case of events that result from procedural evolution, such as phlebitis and pressure injury.
Nurses were the highest notifiers, accounting for 80.38% of the total notifications in the three years of the research. This data is confirmed by other authors6,7, however, in other publications physicians appear as the largest notifiers2, in addition to administrative assistants, nursing technicians6 and pharmacists21. It is known that the risks for incidents should be shared among the multidisciplinary team23, as well as the responsibility for notifications.
The incidents with the highest proportions were phlebitis, 27.05%; those related to surgeries, 19.20%; falls, 17.27%; problems related to the drug chain, 12.19%; skin lesions, 9.47%; and problems with patient identification, 3.77%. Despite the relevance for patient safety and the high proportion found, this incident is not among the most common notifications in health services24. This result leads to the possibility that there may be underreporting of phlebitis, since infusional therapy and the existence of patients with risk factors for phlebitis, such as the elderly, are part of the daily life of health services25. Although phlebitis is considered an adverse event, it is not yet part of ANVISA's basic patient safety protocols. This may be a factor that negatively influences its identification and notification since the adoption of protocols can contribute to the performance of more safe care due to the fact of guiding conducts and failure prevention26.
Regarding incidents related to surgeries, part of them concern the non-follow-up of the safe surgery protocol, indicating that there may be a maturing of the team regarding the concerns with patient safety in the surgical context and thus contributing to the safety culture.
It is observed that the most reported incidents, apart from phlebitis and surgeries, agree with the literature, only with some variations in percentage terms12)(14)(15)(17)(19)(20)(21)(27)(28. A study conducted in 12 large hospitals in the metropolitan region of Salvador - Bahia reported as most prevalent adverse events pressure injury (88.9%), falls (77.8%), medication errors (75%), unscheduled removal of drains and tubes (42.9%), and failures in patient identification (33.3%)24. In Kenya, a study shows that the most reported events were associated with medications, blood use and medical-hospital equipment18. In Austria, research indicates that the most reported incidents relate to surgeries (45%), patient identification (12%), errors in drug management (9%), medical-hospital equipment (10%) and communication failures (6%)7.
Most incidents (91.52%) resulted in minor damage; events with moderate damage corresponded to 6.96%; the severe were 0.22%; and 0.32% led the patient to death. Other studies indicate the occurrence of 79.6% of mild damage, with temporary effects on patients. Incidents related to the drug chain were more prevalent as well as severe (82%)12. Data on reports of adverse events in Indonesia point to the occurrence of 19.71% of mild injuries, 2.19% of permanent injuries and 8.76% of deaths29. A study based on notifications in the NOTIVISA system between 2014 and 2016 identified that, out of a total of 63,933 adverse events related to health care, 417 9 (0.6%) led to death. According to research data, only one Brazilian state did not receive notification of death in the period studied. The incidents were associated with infection related to health care, the administration of intravenous drugs and fluids, the use of blood and blood products, medical articles and equipment, and structural and facility problems30.
The World Health Organization recognizes that the occurrence of adverse events is a failure in patient safety and that about 60% of the incidents that occurred could be avoided. Patient safety strategies should be measures capable of preventing risks and reducing the possibility of harm due to health care11. Adverse events impose consequences on patients and health services, such as increased hospital costs with hospitalizations, longer bed stay, additional need for diagnostic and therapeutic procedures, increased consumption of medications, absenteeism at work and risk of premature death20.
This study presents as a limitation the fact that it was performed with data of voluntary notifications made in an electronic system. As such, one cannot rule out the possibility of underreporting and therefore may not reveal the incident panel in its entirety. Another limiting factor is the lack of information on some items, such as the location and shift of the occurrence, data on the characterization of patients and incidents, and the degree of damage. Nevertheless, it is known that voluntary notifications are widespread throughout the world, being one of the most useful methods for generating behavioral changes because it allows learning with one's own mistakes. It is noteworthy that the non-use of notifications with punitive and disciplinary purposes favors the adhering to their practice, as well as the investment in permanent education activities to disseminate safe and necessary health practices to strengthen the culture of patient safety12.
CONCLUSION
The analysis of incidents related to health care voluntarily reported over a period of three years showed a general incidence of notifications of 7.94 per 100 patient-days, of which 48.14% caused some harm to patients. The incidence of adverse events was 3.82 per 100 daily hospitalized patients. Phlebitis was the most reported incident, followed by the group of surgeries and falls. Overall, 91.52% of the events caused mild damage, but there were three deaths in the period.
The results found allow us to highlight the importance of voluntary notifications of incidents as one of the factors that contribute to the strengthening of safety programs and culture. Knowledge and determination of the magnitude of incidents and their related characteristics, as well as the analysis of the profile of patients affected, can support local planning and the implementation of various measures, such as educational actions. These can help professionals understand the meaning and importance of notifications, and ultimately favor the improvement of patient quality and safety.
Funding:
Project financed with a research initiation grant by the Remaining Program, 2019/2020 edition, Pro-Rectory of Affirmative Actions and Student Assistance, Federal University of Bahia
REFERENCES
1. Gao X, Yan S, Wu W, Zhang R, Lu Y, Xiao S. Implications from China patient safety incidents reporting system.Therapeutics and Clinical Risk Management. 2019;15:259-267. http://dx.doi.org/10.2147/TCRM.S190117 [ Links ]
2. Fragata J, Sousa P, Santos RS. Organizações de saúde seguras e fiáveis/confiáveis. Cap. 1. In.: Sousa P, Mendes W (Org.). Segurança do paciente: criando organizações de saúde seguras. 2.ed (revista e ampliada). Rio de Janeiro, RJ: CDEAD, ENSP, Fiocruz, 2019:20-40. https://doi.org/10.7476/9788575416426 [ Links ]
3. Alves SAC, Pereira AGD, Delduque MC. Segurança do Paciente: Aspectos comparativos entre Brasil e Portugal. In.: Santos AO, Lopes LT. Coletânea direito à saúde: boas práticas e diálogos institucionais. [Internet]. Brasília: CONASS, 2018: 168-182. [cited 2020 Sep 15]. Available from: http://www.resbr.net.br/coletanea-direito-a-saude-conass/#.XyqPzChKi73 [ Links ]
4. Patient safety is not a luxury. The Lancet. 2016; 387(19):1133 doi: https://doi.org/10.1016/S0140-6736(16)30003-4 [ Links ]
5. World Health Organization (WHO).World Alliance for Patient Safety. WHO patient safety curriculum guide: multi-professional edition [Internet]. Geneva: WHO; 2011 [cited 2016 Oct 31]. Available from: http://apps.who.int/iris/bitstream/10665/44641/1/9789241501958_eng.pdf. [ Links ]
6. Ramírez E, Martín A, Villán Y, Lorente M, Ojeda J, Moro M, et al. Effectiveness and limitations of an incident reporting system analyzed by local clinical safety leaders in a tertiary hospital. Prospective evaluation through real-time observations of patient safety incidents. Medicine. 2018; 97:38(e12509). http://dx.doi.org/10.1097/MD.0000000000012509 [ Links ]
7. Sendlhofer G, Schweppe P, Sprincnik U, Gombotz V, Leitgeb K, Tiefenbacher P, et al. Deployment of critical Incident reporting system (CIRS) in public Styrian hospitals: a five year perspective. BMC Health Services Research. 2019;19:412. https://doi.org/10.1186/s12913-019-4265-0 [ Links ]
8. Dhamanti I, Leggat S, Barraclough S, Liao HH, Abu Bakar N. Comparison of patient safety incident reporting systems in Taiwan, Malaysia, and Indonesia. Journal of Patient Safety. 2020; Volume Publish Ahead of Print. doi: 10.1097/PTS.0000000000000622 [ Links ]
9. Golder S, Loke YK, Wright K, Norman G. Reporting of adverse events in published and unpublished studies of health care interventions: a systematic review. PLoS Med. 2016; 13(9): e1002127. doi:10.1371/journal.pmed.1002127 [ Links ]
10. Whitaker J, Ibrahim F. Incident reporting feedback experience in a UK secondary care setting. Are staff increasingly reluctant to complete incidence forms? The Bulletin. 2016; 98(2):82-84. doi: 10.1308/ rcsbull. 2016.82 [ Links ]
11. World Health Organization (WHO). Conceptual Framework for the International Classification for Patient Safety [Internet]. Patient Safety: WHO Press; 2009. [cited 2020 Sep 15]. Available from: https://www.who.int/patientsafety/implementation/taxonomy/icps_technical_report_en.pdf [ Links ]
12. Figueiredo ML, Oliveira e Silva CS, Brito MFSF, D'Innocenzo M. Analysis of incidents notified in a general hospital. Rev Bras Enferm [Internet]. 2018;71(1):111-9. DOI: http://dx.doi.org/10.1590/0034-7167-2016-0574 [ Links ]
13. Mendes W, Martins M, Rozenfeld S, Travassos C. The assessment of adverse events in hospital in Brazil. Int J Qual Health Care [Internet]. 2009 [cited 2017 Out 27]; 21(4): 279-84. Available from: https://www.aeciherj.org.br/publicacoes/evento-adverso-Brasil-2009.pdf [ Links ]
14. Sell BT, Amante LN, Martins T, Sell CT, Senna CVA, Loccioni MFL. Dimensionamento dos profissionais de enfermagem e a ocorrência de eventos adversos em internação cirúrgica. Cienc Cuid Saude. 2018; 17(1). doi: 10.4025/cienccuidsaude.v17i1.33213 [ Links ]
15. Ortega DB, D'Innocenzo M, Silva LM, Bohomol E. Análise de eventos adversos em pacientes internados em unidade de terapia intensiva. Acta Paul Enferm. 2017; 30(2):168-73. http://dx.doi.org/10.1590/1982-0194201700026 [ Links ]
16. Roque KE, Tonini T, Melo ECP. Adverse events in the intensive care unit: impact on mortality and length of stay in a prospective study. Cad. Saúde Pública. 2016; 32(10):e00081815. http://dx.doi.org/10.1590/0102-311X00081815 [ Links ]
17. Teixeira CC, Bezerra ALQ, Paranaguá TTB, Pagotto V. Prevalência de eventos adversos entre idosos internados em unidade de clínica cirúrgica. Rev baiana enferm. 2017; 31(3):e22079. doi: 10.18471/rbe.v31i3.22079 [ Links ]
18. Macharia WM, Muteshi CM, Wanyonyi SZ, Mukaindo AM, Ismail A, Ekea H, Abdallah A, Tole JM, Ngugi AK. Comparison of the prevalence and characteristics of inpatient adverse events using medical records review and incident reporting. S Afr Med J. 2016;106(10):1021-1036. doi:10.7196/SAMJ.2016.v106i10.10619 [ Links ]
19. D'Amour D, Dubois CA, Tchouaket E, Clarke S, Blais R. The occurrence of adverse events potentially attribuTable to nursing care in medical units: cross sectional record review. Int J Nurs Stud. 2014; 51(6):882-91. http://dx.doi.org/10.1016/j. ijnurstu.2013.10.017 [ Links ]
20. Sousa P, Uva AS, Serranheira F, Uva MS, Nunes C. Patient and hospital characteristics that influence incidence of adverse events in acute public hospitals in Portugal: a retrospective cohort study. Int J Qual Health Care. 2018; 30(2):132-7. http://dx.doi.org/10.1093/intqhc/mzx190 [ Links ]
21. Moreira IA. Notificação de eventos adversos: o saber e o fazer de enfermeiros. Dissertação (mestrado). Universidade Federal de Goiás. [Internet].Goiânia, 2018. [cited 2020 Sep 15]. Available from: http://repositorio.bc.ufg.br/tede/handle/tede/8759 [ Links ]
22. Araújo ACQ, Silva VA, Mota RS, Mendes AS, Barros AS, Sant'Anna MV, et al. Incidentes relacionados à assistência à saúde em idosos hospitalizados. Rev enferm UFPE online. 2020;14:e244639. https://doi.org/10.5205/1981-8963.2020.244639 [ Links ]
23. Amaral RT, Bezerra ALQ, Teixeira CC, Paranaguá TTB, Afonso TC, Souza ACS. Riscos e ocorrências de eventos adversos na percepção de enfermeiros assistenciais. Rev Rene. 2019;20:e41302. doi: 10.15253/2175-6783.20192041302 [ Links ]
24. Costa EAM, Lobão WM, Ribas CLM, Passos NM. Segurança do paciente em serviços de saúde: uma análise na cidade de Salvador, Bahia. Rev. SOBECC. 2020; 25(1):17-24. doi: 10.5327/Z1414-4425202000010004 [ Links ]
25. Mota RS, Silva VA, Mendes AS, Barros AS, Santos OMB, Gomes BP. Incidência e caracterização das flebites notificadas eletronicamente em um hospital de ensino. Rev baiana enferm. 2020;34:e35971. doi:10.18471/rbe.v34.35971 [ Links ]
26. Aozane F, Cigana DJ, Benetti ERR, Herr GEG, Kolankiewicz ACB, Pizolotto MF. Percepções de enfermeiros de um hospital privado sobre eventos adversos na assistência de enfermagem. Revenferm UFPE online. 2016;10(2):379-86. doi: 10.5205/reuol.8557-74661-1-SM1002201601 [ Links ]
27. Costa NN, Silva AEBC, Lima JC, Barbosa MRS, Freitas JS, Bezerra ALQ. O retrato dos eventos adversos em uma clínica médica: análise de uma década. Cogitare Enferm [Internet]. 2016; 21(esp): 01-10. [cited 2020 Sep 15]; Available from: https://revistas.ufpr.br/cogitare/article/view/45661/pdf_1 [ Links ]
28. Vossoughi S, Perez G, Whitaker BI, Fung MK, Rajbhandary S, Crews N, Stotler B. Safety incident reports associated with blood transfusions. Transfusion. 2019;59;2827-2832. doi: 10.1111/trf.15429 [ Links ]
29. Komite Keselamatan Pasien Rumah Sakit. Pedoman Pelaporan Insiden Keselamatan Pasien (IKP). [Internet]. Jakarta: KKPRS; 2015. [cited 2020 Sep 15]. Available from: http://rspmanguharjo.jatimprov.go.id/wp-content/uploads/2020/02/1.-PEDOMAN-PELAPORAN-INSIDEN-KESELAMATAN-PASIEN-IKP-KKPRS-2008-EDISI-2.pdf [ Links ]
30. Maia CS, Freitas DRC, Gallo LG, Araújo WN. Registry of adverse events related to health care that results in deaths in Brazil, 2014-2016. Epidemiol. Serv. Saude. 2018;27(2):e2017320. doi: 10.5123/S1679-49742018000200004 [ Links ]
Received: October 14, 2020; Accepted: March 03, 2021











 text in
text in 





