My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.20 n.64 Murcia Oct. 2021 Epub Oct 25, 2021
https://dx.doi.org/10.6018/eglobal.435321
Reviews
Nursing diagnoses for patients with traumatic brain injury: integrative review
1 Estudiante de Enfermería de la Universidad Regional de Cariri (URCA), Departamento de Enfermagem. Cariri. Brasil. mariaisabelcs28@outlook.com
2 Enfermera graduada por la Universidad Regional de Cariri (URCA). Brasil.
3 Enfermera. Maestra en Enfermería por el Programa de Posgraduación en Enfermería de la Universidad Regional de Cariri (URCA). Brasil.
4 Enfermera. Doctora en Ciencias de la Salud. Docente Adjunto de la Universidad Regional de Cariri (URCA). Brasil.
Introduction:
Traumatic Brain Injury (TBI) is any impact that affects the head region involving the scalp, skull, brain and blood vessels, affecting these structures. Nursing professionals play a fundamental role during the care of these patients.
Objective:
To list the Nursing Diagnoses (ND) of NANDA I that can be proposed for patients hospitalized with TBI.
Method:
Integrative literature review, performed at the following databases: LILACS, BDENF, IBECS, MEDLINE, CINAHL, SCOPUS and WEB OF SCIENCE, using the search terms: “Traumatismos Craniocerebrais/Craniocerebral Trauma”, “Diagnóstico de Enfermagem/Nursing Diagnosis” and “Enfermagem/Nursing”. Articles in Portuguese, English and Spanish were included.
Results:
The selection included 12 articles. From the reading of the studies, based on the clinical characteristics and the basic needs affected by patients with TBI, 18 ND were listed, organized alphabetically and according to their domain in NANDA I.
Final considerations:
The findings of this research allowed characterizing important aspects related to the patient with TBI and bringing the literature approach on nursing diagnoses to this population. There is a gap in the investigations that address ND for patients with TBI, taking into account that a significant part of the studies report on the clinical manifestations perceived during nursing care and do not bring the elaborated diagnoses.
Keywords: Craniocerebral Trauma; Nursing Diagnosis; Nursing
INTRODUCTION
Traumatic Brain Injury (TBI) means any impact that affects the head region involving the scalp, skull, brain and blood vessels, affecting these structures. The lesion may start at the time of occurrence, being considered as primary, or after a few days or weeks, known as secondary injury. Moreover, it can be classified as an open or closed trauma, the latter occurring when the brain performs impacting movements within the skull cap at the time of the accident, causing internal changes1.
In Brazil, the TBI is associated with high levels of morbidity and mortality, being estimated that approximately 50% of hospitalizations are due to trauma, and the TBI is its largest representative, causing a great impact on public health services and people’s lives, since, when the victim does not progress to death, the accident causes prolonged or permanent sequelae, requiring, according to the severity of the patient’s condition, hospitalization, which directly interferes with the quality of life of the individuals2.
Several etiologies cause TBI, with automobile accidents as the most frequent. The increased number of vehicles, associated with the behavior of users and the lack of general supervision, has contributed to this. However, other causes also cause trauma, such as falls, urban violence, firearm accidents, running over and sportive accidents3,4.
The severity of TBI is defined by the trauma impact, and, according to the parameters obtained in the Glasgow Coma Scale, it can be classified as mild patients with scores between 13 and 15, score between 9 and 12 moderate and between 3 and 8 severe. This scale is used worldwide to assess the level of consciousness, patient evolution, neurological dysfunctions and standardizes language among professionals5,6.
The care of users of the health service with TBI involves a systematized, comprehensive and effective care, performing a detailed neurological evaluation that allows observing the alterations, structures and functions compromised; maintenance of physiological parameters such as: blood pressure, cerebral perfusion pressure, oxygen saturation and ventilation, with a view to starting treatment early and minimizing the risks of secondary injuries7.
Nursing professionals, as active members of the health team, play a fundamental role during the care of these patients, developing techniques and attitudes according to the needs presented by each patient. To guide the work of these professionals, the Systematization of Nursing Care (SNC) is the strategy to organize the service regarding the work method, instrument and personnel in all institutions that have nursing actions8.
The Nursing Process (NP) is one of the most used methods to organize and direct nursing care, being divided into five interconnected and recurrent stages, which are: data collection, preparation of nursing diagnoses, planning of interventions, implementation and evaluation. The nursing diagnosis (ND), as one of the stages of the NP, consists of grouping the information collected during the patient’s complete anamnesis and identifying the affected human responses that require nursing interventions. The elaboration of the diagnoses is what will guide the definition of the care plan and the establishment of priorities at the time of care9,10.
To assist in the grouping of the collected data, the Taxonomy of Nursing Diagnoses of Nanda International (NANDA-I) is one of the languages of nursing that plays an important role for the profession, standardizing the terms used by the team, facilitating communication and developing nursing diagnostic research as a form of contribution to health care11.
Thus, it is essential that nurses have knowledge related to the care of patients who are victims of TBI in order to promote qualified nursing care. In this sense, the present study aimed to list the nursing diagnoses of NANDA I that can be proposed for patients hospitalized with TBI according to their affected basic needs verified during the care of the nursing team to these victims.
METHOD
This is an integrative literature review, which proposes to group findings obtained in studies on a given subject, gathering comprehensive information and allowing a more reliable understanding of the theme in interest12. The steps proposed by Mendes, Silveira and Galvão13 were followed in a systematized way: establishment of the research question; criteria for searches in the literature; categorization of studies; evaluation of the studies included in the review; interpretation of the results and presentation of the review.
For the development of the research, the following question was used: “What nursing diagnoses can be proposed to victims of traumatic brain injury?”. Based on this research question, the Health Sciences Descriptors (DeCS), Medical Subject Headings (MeSH), inclusion and exclusion criteria of the articles were established.
For the selection of the articles, the following databases were used: Latin American and Caribbean Health Sciences Literature (LILACS), Nursing Database (BDENF), Spanish Bibliographic Health Sciences Index (IBECS), Medical Literature Analysis and Retrieval System Online (MEDLINE), Cumulative Index to Nursing and Allied Health Literature (CINAHL), SCOPUS and WEB OF SCIENCE.
The search was conducted in February and March 2020 through online access to the aforementioned databases. Inclusion criteria were: Free full text; publications in Portuguese, English and Spanish; main subject nursing diagnoses related to the patient who is victim of TBI. There was no limitation of the year of publication, considering that the TBI has always been a public health problem in Brazil and in the world, thus being conFigured in a timeless study. Duplicated articles were excluded.
The descriptors used were: Traumatismos Craniocerebrais, Diagnóstico de Enfermagem and Enfermagem, with their respective Medical Subject Headings (MeSH): Craniocerebral Trauma, Nursing Diagnosis and Nursing. The crossing between the terms was carried out using the Boolean operator AND and resulted in 856 publications, adding the production of all bases before the application of the inclusion criteria as shown in Chart 1.
Chart 1: Search at LILACS, MEDLINE, BDENF, IBECS, CINAHL, SCOPUS and WEB OF SCIENCE databases according to the established inclusion criteria, Crato, Ceará, Brazil, 2020.

Source: Created by the authors.
For data collection from the articles, a guide was used to expose the characteristics of the research: authors, article title, year of publication, language, indexed database, objective, level of evidence, type of study, study population and main findings.
The levels of evidence of the articles were classified as: I. Evidence from systematic reviews or meta-analysis of all randomized controlled clinical trials (RCCT) relevant to or from clinical guidelines based on systematic reviews of RCT; II. Evidence derived from at least one well-delineated RCCT; III. Evidence obtained from well-delineated clinical trials, without randomization; IV. Evidence from a case-control study or a well-delineated cohort study; V. Evidence from a systematic review of qualitative and descriptive studies; VI. Evidence derived from a single descriptive or qualitative study and VII. Evidence from the opinion of authorities and/or reports of expert committees14.
Based on the nursing diagnoses found during the reading of the articles and the changes in basic human needs affected in patients with TBI, the main ND that can be proposed to this population were listed. To prepare the nursing diagnoses, the NANDA I taxonomy of the current version of 2018-2020 was used.
The findings were analyzed, descriptively exposed and presented through Charts, discussed reflectively according to the literature and the studied theme.
RESULTS
In order to answer the main question of this research, 12 original articles were selected, organized according to the identification variables: authors, year of publication, title, objective (Chart 2); and methodological design: level of evidence, type of study, population and main findings (Chart 3).
Of the selected articles, ten were in English and are indexed in MEDLINE, and two in Spanish that were found in the IBECS and LILACS databases. The studies were published between 1991 and 2018, and most were published in 2018.
Chart 2: Characteristics of the selected studies. Crato, Ceará, Brazil, 2020. (15)(16)(17)(18)(19)(20)(21)(22)(23)(24)(25)(26
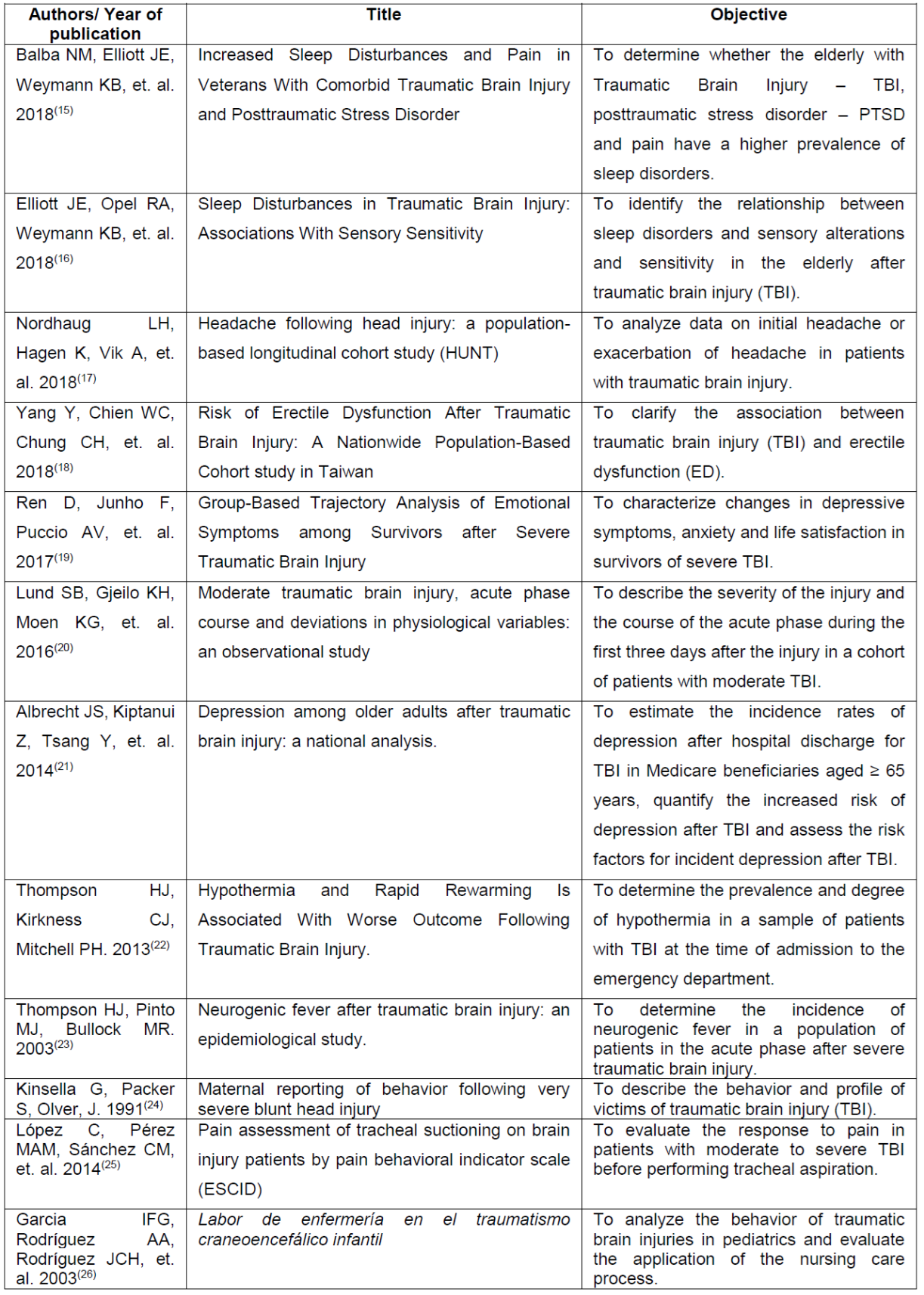
Source: Created by the authors.
Chart 3: Methodological design of the selected studies. Crato, Ceará, Brazil, 2020. (15)(16)(17)(18)(19)(20)(21)(22)(23)(24)(25)(26

Source: Created by the authors.
From the reading of the articles, based on the clinical characteristics and the affected basic needs of patients with TBI, 18 ND were listed, as shown in Chart 4, organized alphabetically and according to their domain in NANDA I.
DISCUSSÃO
The articles address the profile of patients with TBI, the care to these individuals at health services, clinical characteristics presented during the evaluation by nursing professionals and portray information that provides support for the elaboration of a reflective critical thinking by the team in the establishment of nursing diagnoses that affects people victims of TBI.
The practice of the nursing process as a methodological instrument of work in health services is of fundamental importance, because it guides the actions to be carried out by nursing professionals, standardizes the dialogue between those involved in care, values the category when appropriating something that is private in the performance of their work and allows applying the scientific technical knowledge of nursing27.
The passage through traumatic events that result in damage to health causes stress in people’s lives. Patients with TBI tend to present psychological changes after injury that may even interfere with the normal sleep pattern. The ND found related to these alterations were mainly anxiety, unsTable emotional control, impaired memory, low situational self-esteem and sleep pattern disorder15)(16)(18)(19)(24.
When considering patients victims of accidents that cause physical injuries, the health team’s concern often focuses on meeting these impacts, normally disregarding or missing other important aspects related to the person’s coping and acceptance during treatment and passage through such a situation. A significant finding was observed in the number of people with TBI who, after the trauma, presented anxiety, showing that, although it is a feeling frequently reported by the general population currently, it bothers and interferes with the quality of life of individuals, because not all are prepared to deal with concerns15)(16)(18)(19.
Regarding physical impairments, the ones that most caused instability in the condition were: altered respiratory pattern, impaired gas exchange resulting in poor tissue perfusion, impaired verbal communication, impaired physical mobility, deficient fluid volume and impaired skin integrity, thus favoring the risk of infections18)(20)(24)(26.
Acute pain was also a frequent diagnosis verified during care. Although, in some patients, this parameter was tested during nursing procedures, such as tracheal aspiration, pain is commonly observed in trauma victims and evidence shows that some factors, such as mobilization and execution of techniques, influence its perception by the patient16)(17)(25)(26. This demonstrates that pain control measures are essential to provide the best possible comfort to patients, especially in trauma victims, who have severe repercussions and acute pain.
A study conducted in southern Brazil in 2015 sought to know the factors that act in the perception of acute pain and the consequences of this experience in patients victims of mild trauma, unveiling that trauma-related acute pain can be influenced by factors of various orders: biological, emotional, spiritual and sociocultural. Furthermore, the alterations highlighted are from biological impairments, such as tachycardia and dyspnea, even emotional, such as nervousness, confusion, despair and feeling of impotence28.
Other nursing diagnoses found, such as hyperthermia and ineffective thermoregulation, have important characteristics to be investigated during physical evaluation and vital signs in patients with TBI. In the victims of severe TBI, during the acute phase of the injury, temperature change occurs frequently, including the incidence of neurological fever and the risk of developing it, because severe TBI is assumed to be associated with lower GCS scores and lesions in deep brain structures such as the hypothalamus, thermoregulatory center20)(23)(26.
The effects of hypothermia on the patient were also investigated and, since people arriving at the health service after suffering a TBI with hypothermia presented lower values on the Glasgow scale, the hospitalization period was prolonged and the mortality rate was higher22. For patients who demonstrated temperature changes, the proposed ND were: Hyperthermia, hypothermia and ineffective thermoregulation, all included in domain 11 of NANDA-I regarding safety/protection.
Thus, TBI causes significant changes in people’s lives, including changes in lifestyle and important functions of the body. Considering this, upon listing nursing diagnoses, the team directs care to solve the problem and promotes quality care, individually meeting patients and their affected basic needs.
CONCLUSION
The findings of this research allowed characterizing important aspects related to the patient with TBI and bringing the literature approach on nursing diagnoses to this population. Although the number of articles included is considerable, there is a gap in the investigations that address ND for patients with TBI, taking into account that a significant part of the studies report on the clinical manifestations perceived during nursing care and do not bring the diagnoses elaborated. It was possible to verify that most publications had a cohort design, classified as level of evidence IV.
Eighteen NANDA-I nursing diagnoses were listed based on clinical characteristics, affected basic needs of patients with TBI and information from selected studies. The diagnoses of domain 11 - safety/protection were more frequent, being entitled: Hyperthermia, hypothermia, impaired skin integrity and ineffective thermoregulation.
There was a distribution in relation to the nursing diagnoses found related to the physical and emotional aspects of patients, revealing the importance of an integral, individualized evaluation and consistent with the compromised real basic human needs, in order to minimize the sequelae resulting from trauma and ensure greater quality during care.
The strengthening of nursing depends on professional performance in the work environment and on his/her work and appropriation of the methods that organize his/her care. From this perspective, nurses should develop more studies focused on nursing diagnoses in patients who are victims of TBI, in order to contribute to the proper management and care offered to this portion of the population.
REFERENCIAS
1. Reis LRA, Santos CJSF, Fraga FV, et. al. Traumatismo craniano em acidentes de trânsito: cuidados prestados pela equipe de atendimento pré-hospitalar. Revista de Saúde da Reages. 2019 Jan; 1(4):36-38 [acesso em 14 mar 2020]. Disponível: https://www.faculdadeages.com.br/uniages/wp-content/uploads/2019/07/p.-36-38.pdf. [ Links ]
2. Rodrigues MS, Santana LF, Silva EPG, et. al. Epidemiologia de traumatismo craniencefálico em um hospital. Rev Soc Bras Clin Med. 2018 Jan; 1(16):21-24 [acesso em 14 mar 2020]. Disponível: http://docs.bvsalud.org/biblioref/2018/06/884987/dezesseis1_vinteum.pdf. [ Links ]
3. Arruda BP, Andreza PX, Akamatsu PYF, et. al. Traumatic brain injury and its implications on cognition and quality of life. Acta Fisiátrica. 2015 Jan; 22(2):55-59 [acesso em 14 mar 2020]. Disponível: https://www.revistas.usp.br/actafisiatrica/article/view/114498/112327. [ Links ]
4. Santos WC, Vancini-Campanharo CR, Lopes MCBT, et. al. Assessment of nurse's knowledge about Glasgow coma scale at a university hospital. Einstein (são Paulo). 2016 Jun; 14(2):213-218 [acesso em 17 mar 2020]. Disponível: https://www.scielo.br/pdf/eins/v14n2/1679-4508-eins-14-2-0213.pdf. [ Links ]
5. Silva JA, Souza AR, Feitoza AR, et. al. TRAUMATISMO CRANIOENCEFÁLICO NO MUNICÍPIO DE FORTALEZA. Enfermagem em Foco. 2017 Abr; 8(1):22-26 [acesso em 17 mar 2020]. Disponível: http://revista.cofen.gov.br/index.php/enfermagem/article/view/724/368. [ Links ]
6. Silva PF, Silva AS, Olegário WKB. Caracterização das vítimas de traumatismo encefálico que evoluíram para morte encefálica. Revista Cuidarte. 2018 Set; 9(3):1-12 [acesso em 03 abr 2020]. Disponível: https://revistacuidarte.udes.edu.co/index.php/cuidarte/article/view/565/1018. [ Links ]
7. Amorim CF, Júnior JEM, Alves TEA, et. al. Avaliação Neurológica Realizada por Enfermeiros em Vítimas de Traumatismo Cranioencefálico. Rev. Neurocienc. 2013; 21(4):520-524 [acesso em 03 abr 2020]. Disponível: http://www.revistaneurociencias.com.br/edicoes/2013/RN2104/original/819original.pdf. [ Links ]
8. Louro ALF. Estratégias para o cuidado humanizado à pessoa em situação crítica [dissertação de mestrado]. Lisboa: Universidade Católica Portuguesa, Curso de Enfermagem, Instituto de Ciências de Saúde; 2014 [acesso em 09 abr 2020]. Disponível: https://repositorio.ucp.pt/bitstream/10400.14/15337/1/Estrat%C3%A9gias%20para%20o%20Cuidado%20Humanizado%20%C3%A0%20Pessoa%20em%20Situa%C3%A7%C3%A3o%20C.pdf. [ Links ]
9. Ferreira AM, Rocha EN, Lopes CT, et. al. Diagnósticos de enfermagem em terapia intensiva: mapeamento cruzado e Taxonomia da NANDA-I. Revista Brasileira de Enfermagem. 2016 Abr; 69(2):307-315. 2016 [acesso em 09 abr 2020]. Disponível: https://www.scielo.br/pdf/reben/v69n2/en_0034-7167-reben-69-02-0307.pdf. [ Links ]
10. Bugs TV, Matos FGOA, Oliveira JLC, et. al. Avaliação da acurácia dos diagnósticos de enfermagem em um hospital universitário. Revista eletrônica trimestral de enfermagem. 2018; 52:179-191 [acesso em 23 mar 2020]. Disponível: http://scielo.isciii.es/pdf/eg/v17n52/pt_1695-6141-eg-17-52-166.pdf. [ Links ]
11. Okuno MFP, Costa N, Lopes MCBT, et. al. DIAGNÓSTICOS DE ENFERMAGEM MAIS UTILIZADOS EM SERVIÇO DE EMERGÊNCIA. Cogitare Enfermagem. 2015 Jun; 20(2):385-391 [acesso em 17 mar 2020]. Disponível: https://revistas.ufpr.br/cogitare/article/view/38606/25536. [ Links ]
12. Ercole FF, Melo LS, Alcoforado CLGC. Integrative review versus systematic review. Reme: Revista Mineira de Enfermagem. 2014; 18(1):9-11 [acesso em 05 abr 2020]. Disponível: https://www.reme.org.br/artigo/detalhes/904. [ Links ]
13. Mendes KS, Silveira RCCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto & Contexto - Enfermagem. 2008 Dez; 17(4):758-764 [acesso em 05 abr 2020]. Disponível: https://www.scielo.br/scielo.php?pid=s0104-07072008000400018&script=sci_arttext. [ Links ]
14. Pinto LLN, Corrêa AR, Donoso MTV, et. al. Strategies for reducing door-to-balloon time in patients with acute myocardial infarction. Reme: Revista Mineira de Enfermagem. 2016; 20:01-10 [acesso em 17 mar 2020]. Disponível: https://cdn.publisher.gn1.link/reme.org.br/pdf/e954_en.pdf. [ Links ]
15. Balba NM, Elliott JE, Weymann KB, et. al. Increased Sleep Disturbances and Pain in Veterans With Comorbid Traumatic Brain Injury and Posttraumatic Stress Disorder. Journal Of Clinical Sleep Medicine. 2018 Nov; 14(11):1865-1878 [acesso em 20 mar 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6223555/pdf/jcsm.14.11.1865. [ Links ]
16. Elliott JE, Opel RA, Weymann KB, et. al. Sleep Disturbances in Traumatic Brain Injury: Associations With Sensory Sensitivity. Journal Of Clinical Sleep Medicine. 2018 Jul; 14(7):1177-1186 [acesso em 23 mar 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6040790/pdf/jcsm.14.7.1177.pdf. [ Links ]
17. Nordhaug LH, Hagen K, Vik A, et. al. Headache following head injury: a population-based longitudinal cohort study (HUNT). The Journal Of Headache And Pain. 2018 Jan; 19(1):2-9 [acesso em 26 mar 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5777966/pdf/10194_2018_Article_838.pdf. [ Links ]
18. Yang Y, Chien WC, Chung CH, et. al. Risk of Erectile Dysfunction After Traumatic Brain Injury: A Nationwide Population-Based Cohort study in Taiwan. American Journal Of Men's Health. 2018 Jan; 12(4):913-925 [acesso em 25 mar 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6131467/pdf/10.1177_1557988317750970.pdf. [ Links ]
19. Ren D, Junho F, Puccio AV, et. al. Group-Based Trajectory Analysis of Emotional Symptoms Among Survivors After Severe Traumatic Brain Injury. Journal Of Head Trauma Rehabilitation. 2017; 32(6)29-37 [acesso em 28 mar 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5552452/pdf/nihms832631.pdf. [ Links ]
20. Lund SB, Gjeilo KH, Moen KG, et. al. Moderate traumatic brain injury, acute phase course and deviations in physiological variables: an observational study. Scandinavian Journal Of Trauma, Resuscitation And Emergency Medicine. 2016 Mai; 24(1):02-08 [acesso em 28 mar 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4878035/pdf/13049_2016_Article_269.pdf. [ Links ]
21. Albrecht JS, Kiptanui Z, Tsang Y, et. al. Depression Among Older Adults After Traumatic Brain Injury: A National Analysis. The American Journal Of Geriatric Psychiatry. 2015 Jun; 23(6):607-614 [acesso em 30 mar 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4306647/pdf/nihms627129.pdf. [ Links ]
22. Thompson HJ, Kirkness CJ, Mitchell PH. Hypothermia and Rapid Rewarming Is Associated With Worse Outcome Following Traumatic Brain Injury. Journal Of Trauma Nursing. 2013 Jan; 17(4):173-177 [acesso em 07 abr 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3556902/pdf/nihms434069.pdf. [ Links ]
23. Thompson HJ, Pinto MJ, Bullock MR. Neurogenic fever after traumatic brain injury: an epidemiological study. J Neurol Neurosurg Psychiatry. 2003 Mai; 74(5):614-619 [acesso em 07 de abr 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1738450/pdf/v074p00614.pdf. [ Links ]
24. Kinsella G, Packer S, Olver, J. Maternal reporting of behaviour following very severe blunt head injury. Journal Of Neurology, Neurosurgery & Psychiatry. 1991 Mai; 54(5)422-426 [acesso em 16 abr 2020]. Disponível: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC488542/pdf/jnnpsyc00503-0038.pdf. [ Links ]
25. López C, Pérez MAM, Sánchez CM, et. al. Valoración del dolor en la aspiración de secreciones traqueales en pacientes con traumatismo craneal mediante la Escala de conductas indicadoras de dolor (ESCID). Enfermería Intensiva. 2014 Jul; 25(3):114-121 [acesso em 16 abr 2020]. Disponível: https://www.elsevier.es/es-revista-enfermeria-intensiva-142-articulo-valoracion-del-dolor-aspiracion-secreciones-S1130239914000273. [ Links ]
26. Garcia IFG, Rodríguez AA, Rodríguez JCH, et. al. Labor de enfermería en el traumatismo craneoencefálico infantil. Rev Cubana Enfermer. 2003 Abr; 19(1) 294-311 [acesso em 19 abr 2020]. Disponível: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-03192003000100009. [ Links ]
27. Malucelli A, Otemaier KR, Bonnet M, et. al. Sistema de informação para apoio à Sistema de informação para apoio à Sistematização da Assistência de Enfermagem. Revista Brasileira de Enfermagem: REBEN. 2010 Ago; 4(63): 629-636. [acesso em 26 jun 2020]. Disponível: https://www.scielo.br/pdf/reben/v63n4/20.pdf. [ Links ]
28. Martin AR, Soares JR, Vieira VCL, et. al. Acute pain from the perspective of minor trauma patients treated at the emergency unit. Revista Gaúcha de Enfermagem. 2015 Jun; 36(2): 14-20. [acesso em 28 jun 2020]. Disponível: https://www.scielo.br/scielo.php?script=sci_arttext&pid=S1983-14472015000200014&lng=en&tlng=en. [ Links ]
Received: July 02, 2020; Accepted: January 10, 2021











 text in
text in 



