My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.21 n.65 Murcia Jan. 2022 Epub Mar 28, 2022
https://dx.doi.org/10.6018/eglobal.484091
Originals
Compliance with standard precaution measures by health professionals: comparison between two hospitals
1 Departamento de Enfermería de Rio das Ostras de la Universidad Federal Fluminense - UFF, Rio das Ostras, RJ, Brasil. priscilabrandao@id.uff.br
2 Universidad Federal del Estado de Rio de Janeiro - UNIRIO, Rio de Janeiro, RJ, Brasil.
3 School of Nursing, Tung Wah College, Kowloon, Hong Kong SAR.
Method:
This is a descriptive study, with a quantitative approach, conducted in two hospitals in the State of Rio de Janeiro. The sample is composed of health professionals who work in health care. Study developed in the period between February 2019 and February 2020. In order to collect data, the we used: 1- Individual and professional information form; 2- Brazilian Portuguese version of the Compliance with Standard Precautions Scale. Data were analyzed using descriptive statistics and hypothesis tests.
Results:
The study was attended by 366 (100.0%) health professionals. The overall score of compliance with standard precautions was 13.4 (66.8%), ranging from 4 to 20. As for the average of the scores between the institutions, the professionals from hospital 1 had an average of 12.6 and those from hospital 2 showed a compliance of 13.6.
Conclusions:
Compliance with standard precautions among health professionals did not happen in its entirety.
Keywords: Infection Control; Universal Precautions; Health Personnel
INTRODUCTION
Standard precautions (SP) are protective measures that should be used by health professionals considering their vulnerability to biological risk, exposure time, and direct contact with patients’ blood and body fluids. These measures consist of the hand hygiene (HH), the use of personal protective equipment (PPE), the care in the use and disposal of sharp materials, the care in the handling of contaminated or suspected contaminated artifacts and the care taken in the patient’s environment. SP were established by the Centers for Disease Control and Prevention (CDC) and are intended to protect health workers and ensure safe patient care, thus preventing infections in the provision of care1.
Systematic application of SP is the main strategy for infection prevention and they should be used throughout professional practice in health care, reducing workers’ exposure to pathogens and decreasing environmental contamination2. Nevertheless, in addition to emphasizing that SP are the basis of prevention, it is essential to highlight that, in some situations, they should be implemented with additional precautions based on how diseases are transmitted3.
Although health professionals know the risks to which they are exposed, there is a deficit in the compliance with these measures. Thus, it is noted the insufficiency of a safety culture with regard to biological risks4. In this sense, several studies have reported insufficient adherence to SP5,6.
Recent surveys show that factors influencing adherence to SP are related to lack of knowledge, workload, forgetfulness, as well as factors such as safety climate, inadequate work conditions, risky behavior, personal judgment and inadequate leadership skills3,7.
Nevertheless, several instruments have been designed and used to assess compliance with SP among health professionals8,9. The Compliance with Standard Precautions (CSPS) is a scale developed and validated in China that intends to carry out this assessment9. The Brazilian Portuguese version of the Compliance with Standard Precautions (CSPS-PB) was validated in Brazil and has the same purpose, with similar reliability, reiterating its trustworthiness to measure compliance with SP.
Considering that the SP should be adopted in the care of all patients, it is essential to assess the compliance with these measures by health professionals through a valid and reliable instrument, since its use can promote the safety of the professional and the patient, in addition to reducing exposure to occupational risks. The use of an instrument capable of measuring compliance with SP by these professionals makes it possible to identify possible limitations, and thus develop management, care and educational strategies that favor satisfactory adherence to these measures.
In this directive, this study was intended to assess compliance with standard precautions by health professionals from two hospitals.
MATERIAL AND METHOD
This is a descriptive study, with a quantitative approach, conducted in two hospitals in the State of Rio de Janeiro, one being a medium-sized municipal hospital located in the coastal lowlands, which will be identified in the text as “hospital 1”, and the other, a large-sized university hospital located in the metropolitan region of the state, identified in the text as “hospital 2”. The choice of scenarios for this study is justified because they are units intended for patient care and are internship fields for nursing students at the university to which the author of this research is linked. Health professionals allocated to the pediatric, emergency, gynecology/maternity, surgical center, medical and surgical clinic, intensive care unit and other patient care units were invited to participate in the research.
This study followed the guidelines recommended by Strengthening the Reporting of Observational Studies in Epidemiology (STROBE).
The study was developed in the period between February 2019 and February 2020. The population is composed of health professionals (nurses, technicians, assistants and physicians) who work in direct patient care in the institutions. Inclusion criteria: being a health professional in the units destined for research in the hospitals; being over 18 years old. Exclusion criteria: having exclusively administrative professional activities. The study sample was based on convenience, conducted in the sectors eligible for the research.
In order to collect data, we used: 1- Individual and professional information form; 2 - Brazilian Portuguese version of the Compliance with Standard Precautions Scale (CSPS-PB)10. The professionals received an envelope with the instruments and the Free and Informed Consent Form, which, after being filled out individually and upon availability, was collected.
CSPS-PB is a scale composed of 20 items with response options that vary among never, rarely, sometimes and always, indicating the frequency of compliance with SP. The scale is composed of five domains presented in its items that address issues related to clinical practice, which are: the use of PPE, disposal of sharp materials, waste disposal, decontamination of artifacts and surfaces, and the prevention of cross infection.
CSPS-PB is a valid and reliable instrument to measure compliance with SP. In the assessment of reliability in the analysis of the overall internal consistency of CSPS-PB, the scale shows a Cronbach’s alpha coefficient of 0.61. By assessing reliability/stability through test-retest, using the intraclass correlation coefficient (ICC), the result obtained was 0.87, indicating very good correlation10.
Data were analyzed using descriptive statistics, with central tendency and dispersion measures, such as absolute (n) and relative (%) frequencies. In order to analyze the scale scores, we considered the 20 items for the response options, which were “never”, “rarely” and “sometimes”, receiving a value of 0, and “always” scoring a value of 1. Accordingly, the score ranged between 0 (minimum score) and 20 (maximum score); thus, the higher the score, the better the compliance. Items 2, 4, 6, and 15 were reversed for the execution of the analyses9.
In order to compare compliance with SP, we considered the following variables: professional category and individual variables, such as: gender, age, acting profession, time in the position, number of places you work, hours worked during the week, knowledge of SP, training and sufficiency of training about SP in the hospital and the adoption of SP as a guideline in the institution. To this end, we used the Mann-Whitney U and Kruskal-Wallis tests. In order to check the existence of a statistically significant relationship, we considered the p value (p<0.05) among the variables. Data were tabulated in a spreadsheet editor, Microsoft Excel®. Normality was checked by means of the Kolmogorov-Smirnov test and statistical analysis was performed using the IBM® SPSS® software, version 21.0.
This is an international partnership project with the School of Nursing, The Hong Kong Polytechnic University. All ethical aspects were contemplated according to Resolutions 466/2012 and 510/2016 of the Brazilian National Health Council. The project was approved by the Research Ethics Committee (Certificate of Presentation for Ethical Appreciation [CAAE, as per its Portuguese acronym]: 61213916.4.0000.5243, opinion nº: 2.623.232). Participants were informed about their anonymity, their voluntary participation, as well as the possibility of minimal risk based on possible discomfort in responding to a questionnaire, culminating in the signing of the Free and Informed Consent Form (FICF).
RESULTS
A total of 366 (100.0%) health professionals participated in the study, of which 114 (31.1%) belonged to hospital 1 and 252 (68.9%) to hospital 2. Most of them were female, 274 (74.9%), with an average age of 42 years (SD=10.7), ranging from 23 to 79 years old. Regarding the acting profession, 167 (47.0%) were nursing technicians and assistants. Among the categories, 135 (36.9%) professionals reported having between 5 and 15 years of work in the position, and 223 (60.9%) had more than 40 hours per week (Table 1).
Table 1. Professional and demographic characterization of health professionals (n=366). Rio de Janeiro, RJ, Brazil, 2019-2020
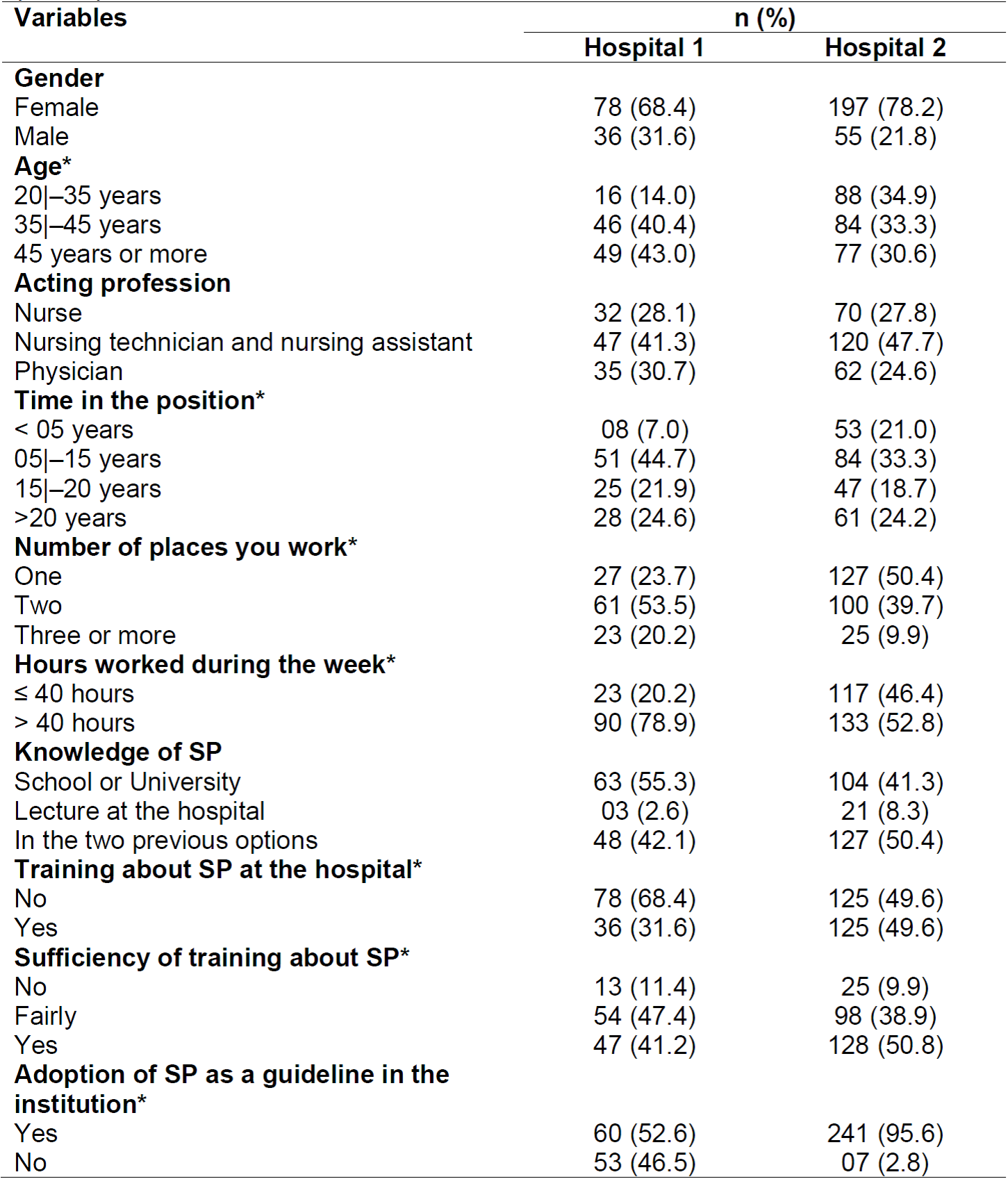
n = number of participants; * = the item was missing
Regarding the responses to the CSPS-PB items, we found that not all professionals comply with SP measures. As for the item that discusses hand washing between contacts with patients, 295 (80.6%) of the surveyed professionals responded that they “always” perform this practice (Table 2).
Table 2. Distribution of the responses of health professionals, facing the items of the CSPS-PB-Rio de Janeiro, RJ, Brazil, 2019-2020
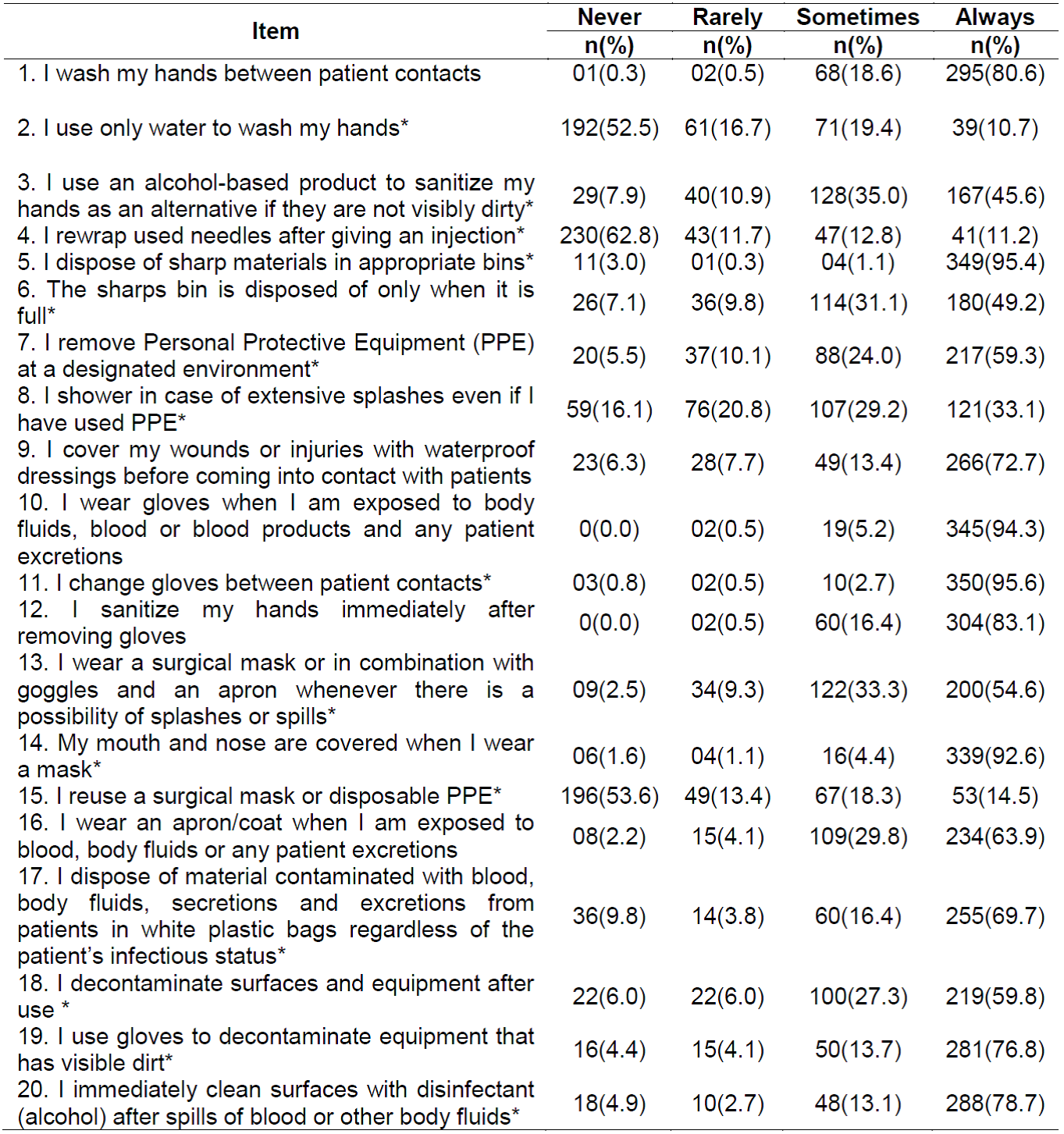
* = the item was missing
Concerning the rewrapping of needles after use, 230 (62.8%) professionals responded “never” for this practice, but a considerable number performs this activity “rarely” or “sometimes”, 90 (24.5%). Regarding item 5, almost all of them (349, 95.4%) dispose of them in appropriate bins. As for the item that corresponds to the act of showering in cases of extensive splashes, even when the professional has used PPE, 121 (33.1%) responded “always”.
Regarding the use of surgical mask or in combination with goggles and apron whenever there is a possibility of splashes or spills, 200 (54.6%) indicated the alternative “always”, followed by 122 (33.3%) for “sometimes”. In the item for the use of apron/coat when they are exposed to blood, body fluids or any excretion from patients, 234 (63.9%) always perform this practice.
With regard to item 10, compliance is 345 (94.3%) among the professionals. 350 (95.6%) change gloves between contacts with patients, revealing good compliance regarding the use of gloves, and 304 (83.1%) professionals reported that they always sanitize their hands immediately after removing the gloves. With respect to the item about the reuse of surgical mask or disposable PPE, 196 (53.6%) professionals said they “never” perform this activity and 53 (14.5%) do it.
Concerning item 2, 192 (52.5%) responded “never”; however, 39 (10.7%) said “always” for this practice. The use of alcohol-based products to sanitize the hands, as an alternative in case they are not visibly dirty, resulted in 167 (45.6%) responses for the option “always”. In case of decontamination of surfaces and equipment after use, 219 (59.8%) professionals “always” perform this activity, followed by 100 (27.3%) “sometimes”.
With regard to item 17, 255 (69.7%) responded “always” in this practice, and 288 (78.7%) said they “always” cleaned surfaces immediately with alcohol after spilling blood or other body fluids. As for the disposal of the sharps bin, 180 (49.2%) responded that they “always” empty it only when it is full, and 26 (7.1%) responded “never”.
The overall score of compliance with SP was 13.4 (66.8%), ranging from a minimum of 4 to a maximum of 20. As for the average scores between the institutions, the professionals from hospital 1 had an average of 12.6 and those from hospital 2 had an average compliance of 13.6.
When comparing the overall score of compliance with SP among the variables, there was a statistically significant difference for gender, age, professional category, hours worked during the week, knowledge of SP, training about SP, sufficiency of training and adoption of SP as a guideline in the work institution (Table 3).
Table 3. Comparison of average compliance scores among occupational variables. Rio de Janeiro, RJ, Brazil, 2019-2020
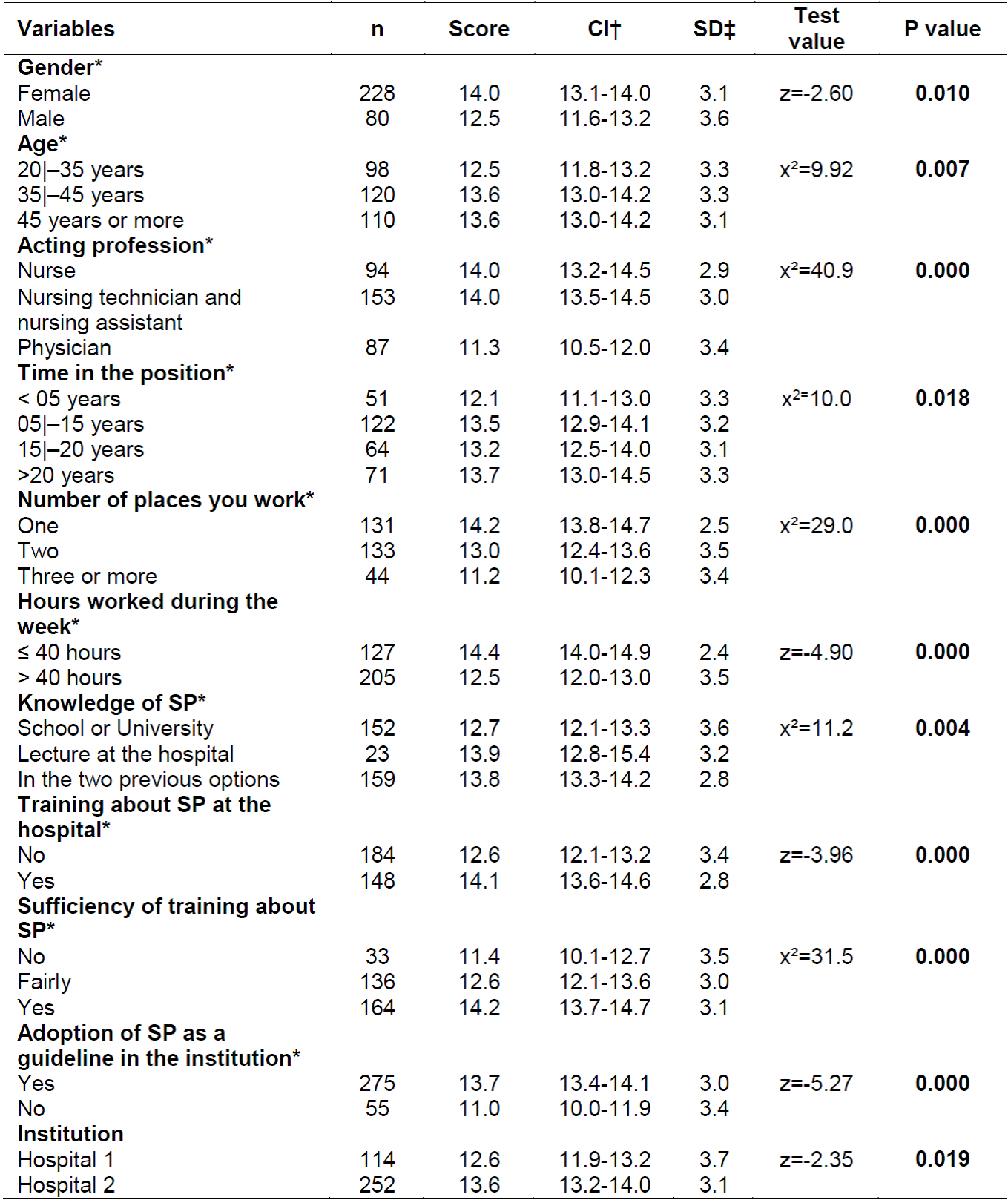
* = the item was missing; †CI = Confidence Interval; ‡SD = Standard Deviation; z = Mann-Whitney Test; x² = Kruskal-Wallis Test.
Regarding the average compliance with SP between genders, women showed a higher score when compared to men (p=0.010). As for the average compliance among professional categories, the nursing staff showed the highest score compared to the medical category (p=0.000).
Regarding the time in the position, the professionals who have more than 20 years of experience showed the highest score compared to the others (p=0.018).
The compliance rate for those who work only in one institution was higher than for those who have more than one institutional link, with a score of 14.2 (SD=2.5). Professionals who work less than 40 hours have a higher score, 14.4 (SD=2.4), compared to those who work more than 40 hours (p=0.000).
As for those who claimed to have received training at the institution and feel sufficiently trained regarding SP, they had average scores of 14.1 (SD=2.8) and 14.2 (SD=3.1), respectively, signaling higher compliance when compared to the other professionals (p=0.000).
DISCUSSION
This study assessed the compliance on the part of health professionals in relation to SP. The sociodemographic data of the participants of this research corroborates other investigations carried out on this theme, with a predominance of the female gender5,6 and with the statistics of professional categories in Brazil, highlighting that most nursing professionals are technicians and assistants11.
Records of the Federal Council of Medicine from 2020 highlight that, in Brazil, there are around 500 thousand active physicians. Reiterating that they are part of the smallest group of professionals that make up the staff of a health institution in Brazil12. Currently, there are more than 2 million nursing professionals, showing that it is a category four times larger than the medical category11.
With regard to training about SP, although most professionals reported feeling sufficiently trained, most reported not having received training in the institution. The responses to the CSPS-PB items showed that not all health professionals comply with these measures as a whole. This finding corroborates other studies conducted in Brazil and worldwide5,6. In an ideal scenario, it would be essential for the institution to offer training to its employees in order to promote a safe environment for the professional and the patient.
With regard to the practice of HH, the health professionals who participated in this research did not comply with this practice in its entirety. This result is similar to the research conducted in a hospital in Sergipe, Brazil, which analyzed the HH adherence by health professionals in oncology and high-complexity services units, and nurses showed a higher rate of adherence compared to other professionals, including physicians and physical therapists13, corroborating the results of this study. It is noteworthy that HH is an indispensable measure for safe care.
Concerning the use of PPE, the results showed good compliance regarding the use of gloves against exposure to body fluids, blood and excretions. Nevertheless, the use of apron/coat for the same purpose was not sufficient. Most professionals reuse disposable PPE, such as surgical mask, showing that it is not a safe practice. In a study conducted in the Federal District (DF), Brazil, among health professionals in an intensive care unit, there was low adherence to PPE when used together, but high adherence when used separately14.
Regarding the disposal of sharp materials, most professionals responded that they disposed of them in their appropriate bins, characterizing a satisfactory result; however, the disposal of material contaminated with blood, body fluids, secretions and excretions of patients in white plastic bags was not sufficient, which may imply a health risk to hospital cleaning teams to the extent that they are directly exposed to the disposal of contaminated materials. Recent surveys show that exposure to blood predominates in accidents with biological material, with percutaneous exposure being the most frequent15.
With regard to the rewrapping of needles, the result obtained in this study shows a risky practice, given that, at some point of their practice, most professionals perform it. Research conducted in two university hospitals in Brazil and Colombia, which assessed the prevalence of accidents with biological material revealed that health professionals, almost in their totality (93.5%), perform the rewrapping of needles; however, the professionals who reported having suffered the accident had a greater perception of occupational risk and the possibility of acquiring diseases16.
In the overall analysis of compliance with SP, we found that professionals do not fully use these measures in their practice, making them more vulnerable. Failures in compliance with HH, inappropriate use of PPE and in the handling of sharp materials are some examples of insufficient compliance, which is also in line with findings from other studies in Brazil and worldwide17,5. Although it is not the objective of this study to assess the factors related to insufficient compliance with these measures, surveys have reported that it may be related to psychosocial and organizational factors3,4.
Individuals between the ages of 20 and 35 had a lower score of compliance with SP. This result may increase the risk of exposure for these professionals. In this directive, a study conducted with secondary data recorded in the Brazilian Information System for Notifiable Diseases, which aimed to describe the characteristics adopted post-exposure among health professionals facing occupational accidents with biological material in Brazil, found that the occurrence of accidents was higher among individuals in the age group between 25 and 31 years18.
Compliance with SP among professional categories was lower among physicians, corroborating a study that assessed the rate of use of PPE during procedures, being lower when compared to nurses14. This result raises an important concern considering that these professionals are also in direct contact with patients in health care.
This research revealed that the higher the number of employment bonds, the lower the compliance rate, which is consistent with studies showing that the workload can directly affect safety issues, impacting on adherence to SP, which is a factor conducive to the occurrence of occupational accidents4.
Another important finding of this research was that the longer the professional has been working, the better were the results of compliance with SP, diverging from another study14 in which it was revealed that the longer the time of work, the more difficult was the adherence. Therefore, it is necessary that educational strategies are carried out to encourage the use of these measures at the time of hiring professionals and continuously throughout the professional practice.
Moreover, it is important to highlight that the professionals who had training showed greater adherence to SP than those who did not receive it; therefore, the continuing education of professionals is crucial for the execution of safe practices19,4.
A study conducted in a district in Ghana, Africa, also indicates that educational programs in conjunction with a national policy and the application of a training manual in the health services should take place in order to reinforce positive attitudes towards SP20.
Regarding the results between the institutions, although hospital 1 receives academics, it is not a university hospital, being a medium-sized hospital with inferior infrastructure and resources when compared to hospital 2, which, besides being a university hospital, has the necessary resources for professionals to have a satisfactory compliance. It is necessary that essential care is taken, especially regarding the resources available and the structure in small and medium-sized hospitals, since they are more prone to negligence in infection control7.
Given the occupational risk, nursing professionals are the most prone to exposure due to direct contact and invasive and continuous activities. In this case, SP comprise prevention measures against exposure to body fluids, secretions, mucous membranes and injured skin, which have clinical picture of infection regardless of diagnosis1.
Since factors such as lack of time; of habit; of PPE, as well as lack of knowledge; of practice; of updates, among others, contribute to the non-compliance with SP, it is essential that training and continuing education are part of the routines of health institutions, because knowledge is dynamic and workers need to be constantly updated16.
The limitation of this study is the self-reported compliance with SP by health professionals through the use of a validated scale with established response options. In this sense, additional studies that assess compliance with these measures through direct observation of clinical practice are valid and necessary.
CONCLUSIONS
The compliance with SP by health professionals did not happen completely, with emphasis on hand hygiene, use of gloves, use of masks and aprons. We also found that a significant portion performs the the rewrapping of needles.
The nursing staff showed higher compliance than the medical category. Longer professional experience and training favored compliance with SP. Nevertheless, professionals with a high workload and more than one employment bond showed lower compliance than the others.
As for the institutions, hospital 2 showed superior compliance compared to hospital 1, although it did not achieve sufficient compliance. In this sense, this study highlights the need to strengthen the safety culture among health professionals.
Therefore, we understand that training is essential upon admission to the institution and the need for a continuing education strategy to ensure compliance with SP in its entirety and over time. Management, care and educational strategies are required to encourage compliance with these measures among health professionals during care procedures, as they are indispensable for the safety of professionals and patients.
It is important to underline that this study was conducted before the pandemic of COVID-19 in Brazil. In this directive, with the change of culture in the use of PPE caused by the pandemic, further studies in the same scenarios may bring different results about compliance with the SP showed in this research.
REFERENCIAS
1. Siegel JD, Rhinehart E, Jackson M, Chiarello L, and the Healthcare Infection Control Practices Advisory Committee, 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Disponível em: https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html [ Links ]
2. Donati D, Biagioli V, Cianfrocca C, De Marinis MG, Tartaglini D. Compliance with Standard Precautions among Clinical Nurses: Validity and Reliability of the Italian Version of the Compliance with Standard Precautions Scale (CSPS-It). Int J Environ Res Public Health. 2019 Jan;16(1):121. Disponível em: doi:10.3390/ijerph16010121 [ Links ]
3. Bouchoucha SL, Moore KA. Factors Influencing Adherence to Standard Precautions Scale: A psychometric validation. Nurs Health Sci. 2019 jun; 21(2):178-185. Disponível em: DOI: 10.1111/nhs.12578 [ Links ]
4. Cunha QB, Camponogara S, Freitas EO, Pinno C, Dias GL, Cesar MP. Fatores que interferem na adesão às precauções padrão por profissionais da saúde: revisão integrativa. Enferm Foco. 2017 [citado 2020 ago 24];8(1):72-76. Disponível em: http://revista.cofen.gov.br/index.php/enfermagem/article/view/980/358 [ Links ]
5. Donati D, Miccoli GA, Cianfrocca C, Di Stasio E, De Marinis MG, Tartaglini, D. Effectiveness of implementing link nurses and audits and feedback to improve nurses' compliance with standard precautions: A cluster randomized controlled trial. Am J Infect Control. 2020;1-7. Disponível em: doi: 10.1016/j.ajic.2020.01.017 [ Links ]
6. Floriano DR, Rodrigues LS, Dutra CM, Toffano SEM, Pereira FMV, Chavaglia SRR. Cumprimento às precauções-padrão por profissionais de enfermagem no atendimento de alta complexidade. Esc Anna Nery. 2019; 23(2). Disponível em: DOI: 10.1590/2177-9465-EAN-2018-0263 [ Links ]
7. Oh E, Choi JS. Factors influencing the adherence of nurses to standard precautions in South Korea hospital settings. Am J Infect Control. 2019;1346-1351. Disponível em: https://doi.org/10.1016/j.ajic.2019.05.015 [ Links ]
8. Chan MF, HO A, Day MC. Investigating the knowledge, attitudes and practices patterns of operating room staff towards standard and transmission- based precautions; results of a cluster analysis. J Clin Nurs. 2008;17:1051-1062. Disponível em: https://doi.org/10.1111/j.1365-2702.2007.01998.x [ Links ]
9. Lam SC. Universal to standard precautions in disease prevention: Preliminary development of compliance scale for clinical nursing. Int J Nurs Stud. 2011 dez;48(12):1533-9. Disponível em: DOI: 10.1016/j.ijnurstu.2011.06.009 [ Links ]
10. Pereira FMV, Lam SC, Gir E. Cultural Adaptation and Reliability of the Compliance with Standard Precautions Scale (CSPS) for Nurses in Brazil. Rev Latino-Am. Enfermagem. 2017;25:e2850. Disponível em: http://dx.doi.org/10.1590/1518-8345.1204.2850 [ Links ]
11. Conselho Federal de Enfermagem [Internet]. Enfermagem em números. 2021 - [citado 2021 abr 19]. Disponível em: http://www.cofen.gov.br/enfermagem-em-numeros [ Links ]
12. Conselho Federal de Medicina [Internet]. Explode número de médicos no Brasil, mas distorções na distribuição dos profissionais ainda é desafio para gestores. 2020 - [citado 2021 abr 19]. Disponível em: https://portal.cfm.org.br/noticias/explode-numero-de-medicos-no-brasil-mas-distorcoes-na-distribuicao-dos-profissionais-ainda-e-desafio-para-gestores/ [ Links ]
13. Llapa-Rodríguez EO, Oliveira JKA de, Menezes MO, Silva LSL, Almeida DM, Neto DL. Aderência de profissionais de saúde à higienização das mãos. Rev enferm UFPE on line. 2018;12(6):1578-85. Disponível em: DOI: https://doi.org/10.5205/1981-8963-v12i6a230841p1578-1585-2018 [ Links ]
14. Castro AF, Rodrigues MCS. Audit of standardized precautionary and contact practices in the Intensive Care Unit. Rev Esc Enferm USP. 2019;53:e03508. Disponível em: https://doi.org/10.1590/s1980-220x2018018603508 [ Links ]
15. Soares RZ, Schoen AS, Benelli KRG, Araújo MS, Neves M. Análise dos acidentes de trabalho com exposição a material biológico notificados por profissionais da saúde. Rev Bras Med Trab. 2019;17(2):201-8. Disponível em: DOI: 10.5327/Z1679443520190341 [ Links ]
16. La-Rotta EIG, Garcia CS, Pertuz CM, Campos IO, Camisão AR, Trevisan DD et al. Conhecimento e adesão como fatores associados a acidentes com agulhas contaminadas com material biológico: Brasil e Colômbia. Ciênc Saúde Colet. 2020;25(2):715-727. Disponível em: DOI: 10.1590/1413-81232020252.04812018 [ Links ]
17. Porto JS, Marziale MHP. Motivos e consequências da baixa adesão as precauções-padrão pela equipe de enfermagem. Rev Gaúcha Enferm. 2016 jun;37(2). Disponível em: doi: http://dx.doi.org/10.1590/1983-1447.2016.02.57395. [ Links ]
18. Gomes SCS, Caldas AJM. Incidence of work accidents involving exposure to biological materials among healthcare workers in Brazil, 2010-2016. Rev Bras Med Trab. 2019;17(2):188-200. Disponível em: DOI: 10.5327/Z1679443520190391 [ Links ]
19. Rosinski J, Rózanska A, Jarynowski A, Wójkowska-Mach J, Team PSHI. Factors Shaping Attitudes of Medical Staff towards Acceptance of the Standard Precautions. Int J Environ Res Public Health. 2019;16(1050). Disponível em: doi:10.3390/ijerph16061050. [ Links ]
20. Akagbo SE, Nortey P, Ackumey MM. Knowledge of standard precautions and barriers to compliance among healthcare workers in the Lower Manya Krobo District, Ghana. BMC Res Notes. 2017;10:432. Disponível em: DOI 10.1186/s13104-017-2748-9 [ Links ]
Received: June 21, 2021; Accepted: September 21, 2021











 text in
text in 


