Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.21 no.66 Murcia abr. 2022 Epub 02-Mayo-2022
https://dx.doi.org/10.6018/eglobal.501511
Reviews
Damage to the health of nursing workers due to the Covid-19 pandemic: an integrative review
1 Universidad Paulista (UNIP), Campus Brasília, Distrito Federal, Brasil. saraivaaguiarricardo@gmail.com
Objective:
To investigate, through an integrative review, the damage to nursing workers' health due to the Covid-19 pandemic.
Method:
Integrative literature review performed in MEDLINE/PubMed, SciELO, LILACS and BDENF databases in September 2020, which generated 1,772 references. After removing the duplicates and using the inclusion and exclusion criteria, the final sample was composed of 22 articles.
Results:
Sleep disorders, depression symptoms, somatic symptoms, anxiety, stress, fatigue, risk of Burnout syndrome, risk of post-traumatic stress, dermatitis and eczema of the hands were harms found in nursing professionals due to the Covid-19 pandemic. Among the protective factors, personal gratification, family relationship, resilience, and personal accomplishment stand out.
Conclusion:
The protection of nursing workers' health involves urgent efforts related to the provision of basic conditions of worker safety, requiring public policies and investments for the preservation of nursing workers' health. Protection actions are related to the implementation of psychological safety management, establishing clear guidelines, promoting continuing education, and ensuring better working conditions.
Keywords: Coronavirus infections; Coronavirus; Nursing; Risk factors; Occupational Health
INTRODUCTION
The Covid-19 pandemic has posed several challenges to health systems around the world due to the number of people infected and the increasing demand on resources needed to cope with it1. Thus, the speed with which Covid-19 has spread between and within countries has influenced the daily lives of billions of people on the planet2.
Healthcare workers are a risk group for Covid-19 because they are directly exposed to infected patients and thus receive a high viral load. In addition, they are under tremendous stress when caring for these patients, many of whom are severely ill, and under often inadequate working conditions2. Increased work hours, physical fatigue, and insufficient and/or negligent health protection and care measures are other factors that increase this risk3.
Thus, health workers involved, directly and indirectly, in facing the pandemic are exposed daily to the risk of getting sick from the coronavirus, and the heterogeneity that characterizes this contingent of the workforce determines different forms of exposure, both to the risk of contamination and to the factors associated with working conditions2)(4)(5.
Among these professionals are the nursing professionals, who represent about 2.2 million in Brazil and who work in different regions and in unequal proportions. They are professionals who are on the front line in the care provided, regardless of the type of care and the health situation, pandemic or not1.
Among those infected with Covid-19, nursing technicians and assistants are the most affected, followed by nurses. The working and socioeconomic conditions experienced by the vast majority of these workers, such as multiple jobs, lack of labor guarantees, and double work day is aggravated by the increased demand at work due to the pandemic situation, associated with the lack of personal protective equipment (PPE) and diagnostic tests, revealing a situation of negligence regarding the protection of professionals and devaluation of workers6)(7.
In this context, Covid-19 can be considered the first new work-related disease to be described in this decade, showing the practical importance of infection control in work environments not only for healthcare workers, but for the protection of all groups of workers involved in care and assistance to the population7.
Therefore, this study aims to investigate the damage to the health of nursing workers due to the Covid-19 pandemic. From this perspective, the question that guided this investigative proposal stands out: what are the damages caused to nursing workers in the exercise of their profession during the Covid-19 pandemic?
MATERIAL AND METHODS
This is an integrative literature review conducted in seven steps8: 1) delimitation of the guiding question of the review; 2) definition of the inclusion and exclusion criteria; 3) extensive search of the literature; 4) identification of potential studies through evaluation of the title and abstract; 5) selection of the articles based on the full text; 6) evaluation of the quality of the included studies; 7) synthesis of the included studies.
The guiding research question was developed based on the PICO strategy: P - population and problem; I - intervention; C - comparison; and O - outcome. Thus, we considered P: nursing professionals; I: pandemic Covid-19; C: normal epidemiological circumstances; O: harm to physical and mental health. In this direction, the constructed question was: what damage was caused to nursing workers in the exercise of their profession during the Covid-19 pandemic?
The search for articles was conducted in September 2020 in the electronic databases MEDLINE/PubMed, Scientific Electronic Library Online (SciELO), Latin American and Caribbean Scientific and Technical Literature (LILACS) and the Nursing Database (BDENF).
To define the search terms, the Health Sciences Descriptors (DeCS) and Medical Subject Headings (MeSH) were consulted. The descriptor "Covid-19" and its correlates were chosen and combined with the search terms "Nursing", "Risk factors", and "Occupational health" and their respective expressions in English. The Boolean operators "AND" and "OR" were used for combination. The strategies built with the search terms and their results are presented in Chart 1.
Table 1: Search strategies and results of the identified productions. Brasilia, Federal District, 2020.
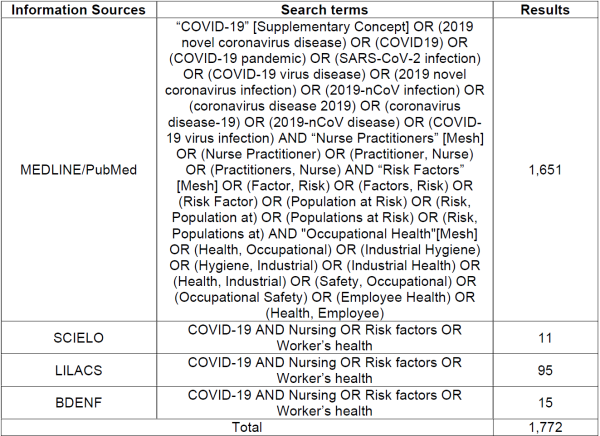
Development: Alves CLM, Aguiar RS (2020).
The inclusion criteria for the sample were: people aged 18 years or older; nursing professionals; addressing damage to the health of nursing workers due to the Covid-19 pandemic; studies with qualitative, quantitative, and mixed methods designs; articles published online in recent years (2019 to 2020), available in Portuguese, English, or Spanish, and in full. Literature reviews, editorials, letters to the editor, correspondence, comments, reflections, and essays were excluded.
The screening of the publications was carried out by two researchers, independently, after reading the titles and abstracts, and, under any divergence during the selection process of the articles, a third researcher could be consulted.
The database search generated 1,772 references. The selection of studies was conducted by exporting the search results from the electronic databases to the EndNote desktop® reference manager. With the program, 16 duplicates were removed, resulting in 1,756 for evaluation of the remaining inclusion criteria by reading the titles and abstracts. Of these, 1,711 were excluded due to the topic (n= 1,676), method (n= 15) or being letters to the editor, correspondence, comments, reflections and essays (n= 20). In the end, 45 articles presented potential for inclusion in the sample and, from these, 22 were chosen after full reading (Figure 1).
The results, the screening and the selection process were presented by means of a flowChart according to the recommendations of the Preferred Reporting Items for Systematic reviews and MetaAnalyses (PRISMA) and also by Tables and in a descriptive way with the objective of synthesizing and fostering discussion about the damage caused to nursing workers in the exercise of their profession during the Covid-19 pandemic.
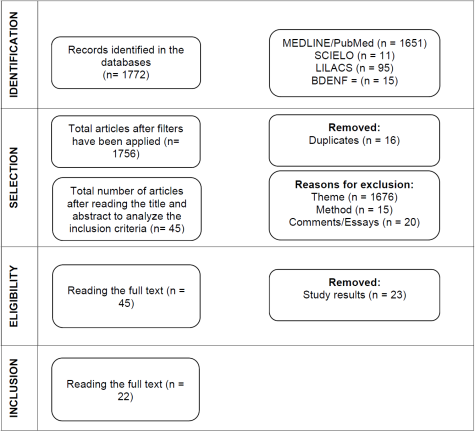
Figure 1: FlowChart of the database search according to PRISMA recommendations. Brasília, Federal District, 2020.
The evidence from the articles was classified into six levels: Level I - studies related tò meta-analysis of multiple controlled studies; Level II - single experimental studies; Level III - quasi-experimental studies, such as non-randomized clinical trial, single group pre- and post-test, and time series or case-control; Level IV - non-experimental studies, such as descriptive, correlational, and comparative research, with a qualitative approach, and case studies; Level V - systematically obtained program evaluation data; and Level VI - expert opinion, experience reports, consensus, regulations, and legislation9.
To facilitate data extraction and synthesis, a synthesis matrix described in an Excel® spreadsheet was prepared. Data was collected as: journal, country and year of publication, author(s), title, study design, main results, and factors related to quality of care and level of evidence. In addition to forming a database, this tool was used to map relevant points, integrate data and characterize the sample reviewed. Thus, part of this data is represented in Chart 2.
Table 2: Final sample of articles. Brasília, Federal District, 2020.

Development: Aguiar RS, Alves CLM, 2020.
The compiled data was then analyzed using thematic analysis32, being organized and presented in thematic categories obtained from the following stages of analysis: 1) data familiarization (results of the studies that comprised the sample and were related to the research question); 2) generation of initial codes; 3) search for themes; 4) review of themes; 5) definition and titling of themes; 6) production of the report.
RESULTS
The final sample of this review was composed of twenty-two articles, as described in Table 2.
All publications refer to the year 2020. Quantitative and cross-sectional designs were the most prevalent among the researches, corresponding to nine articles in each type (40.9%). Regarding the place of publication and development, eight studies (36.3%) were conducted in China, three (13.6%) in Germany (one in conjunction with a report from Malaysia), three (13.6%) in Italy, two (9%) in Brazil, and one (4.5%) in Cuba, Spain, Greece, the Netherlands, Palestine, and Singapore. Regarding the level of evidence of the articles, all studies (100%) fit in level IV that corresponds to non-experimental studies, such as descriptive, correlational and comparative research, with a qualitative approach and case studies.
Thematic analysis of the articles' results allowed the organization into two main thematic categories: 1) Harms to the mental health and physical body of nursing workers in the Covid-19 pandemic; and 2) Opportunities for improvement.
Mental and physical health harms of nursing workers in the Covid-19 pandemic
Most of the articles brought aspects related to the mental health of the professionals. Thus, levels of anxiety, depression and stress were analyzed and emotional exhaustion, risk of post-traumatic stress and risk of Burnout were identified. The need for psychological support services to professionals was mentioned in several articles (N1, N2, N4, N6, N12, N14, N15, N17, N18, N22)10)(11)(13)(15)(16)(17)(18)(19)(20)(21)(23)(24)(26)(27)(28)(29)(30)(31.
Study N1 identified the need for the development of specific actions to manage the psychological safety of health professionals, indicating it as an indispensable point for care due to the professional's vulnerability for the close and constant contact with the pain and suffering of patients10.
Warning of prolonged negative effects and risk of post-traumatic stress disorder, study N2 highlights workers' struggle to cope with the challenge of the pandemic threatening their own health. The professionals reported significant psychological pressure, Burnout, and somatic symptoms. The study suggested offering counseling services and support systems for treatment and prevention of future problems arising from these situations11.
Added to this, according to study N15, are symptoms of post-traumatic stress and depression, anxiety, insomnia, and perceived stress, especially in young women and frontline pandemic workers. Additionally, experiencing hospitalization and death of coworkers was also identified as a contributor to post-traumatic stress24.
Moreover, it was revealed in studies N4 and N8, the great concern of professionals for their families13)(17. Nurses are afraid of infecting themselves and also of transmitting the virus to their relatives (N10, N12, N14, and N19)19)(21)(23)(28. As a measure to mitigate workers' fear for their health and that of their families, study N13 indicates the provision of high quality personal protective equipment (PPE)22. However, it was verified the lack of protective materials or the threat of lacking them, resulting in their reuse due to use limitations (N6, N12 and N14)15)(21)(23.
In addition, professionals have difficulty in meeting the increased demand at work and for their families during measures to close down establishments and circulate the population (N12)21. Corroborating with this result, study N11 in its analysis showed that children, working hours per week and anxiety were the main factors affecting nurse's stress20.
Among the workers' wearing-out processes, work overload, which generates stress, and fatigue were the most prominent (N11, N12, N14, N18, N20, N21, and N22)20,21,23,27,29-31. Study N11 warns about the risk of Burnout due to long working hours in a state of stress, since nurses are prevented from even performing physiological functions by the use of protective clothing20. In study N20, falling goggles was identified as a risk factor for pain symptoms; the study identified environmental stress along with personal disorders as a cause of somatic disorders29.
Additionally, study N14 mentions as of great concern the adaptation of professionals to the workload, dressing and increased complexity of care23. This change in work and increase in stressors impacts both frontline workers in hospitals, ICU care, and emergencies, as well as those attending to chronic and elective conditions, and there is also the possibility of burnout in these caregivers with the extended duration of the pandemic (N18)27.
Also identifying high levels of stress and exhaustion, study N21 suggested improvements such as sufficient staffing, maintenance of teams and work schedules, and also cited leisure time away from work as important30.
Study N3, aiming to better understand the relationship between physical activity and sleep disturbances in a stressful situation like the pandemic, revealed parameters related to sleep disturbances. The participants reported feeling sleepy during the working day and having to make a great effort to stay awake12.
Corroborating this result, study N15 observed that nurses and assistants were more prone to severe insomnia24. Study N17, on the other hand, observed that the prevalence of sleep disturbance was high (38%) in workers at a pediatric hospital during the Covid-19 outbreak. The analysis showed that sleep disturbance was independently associated with Covid-19 patient exposure and depression. Thus, heavy work interfering with the health status of professionals may impact the quality of patient care26.
Studies N7, N9, N16 and N19 were conducted with Covid-19 infected workers16)(18)(25)(28. Thus, study N7 aimed to explore the characteristics of infected workers, and fever, lethargy, and muscle pain were identified as the first symptoms, and the main form of transmission was during nasal and oropharyngeal swab collection. The study recommends annual training on PPE use and additional education during outbreaks. In addition, it was identified that workers also experienced psychological stress and emotional changes that required psychological intervention16.
Infected professionals in study N9 reported respiratory symptoms present in about half of the cases, in addition to anosmia and dysgeusia. About one in three had no symptoms at all. The frequency of anxiety disorder and depression was not higher than commonly recorded in pre-pandemic checks. There was significant risk of anxiety, especially in those with poor sleep quality. The study recommended mental health support, interventions to improve and promote sleep quality, especially for infected workers18.
Study N16 identified non-respiratory symptoms (contrary to study N9) and anosmia as strongly associated with coronavirus infection. Muscle pain, eye pain, general malaise, headache, fatigue, and fever were reported more frequently. The study suggests that the results may help in targeted screening in settings with a lack of diagnostic tests25.
In a retrospective analysis, the N19 study compared clinical, laboratory, and computed tomography (CT) characteristics between contaminated professionals and common patients. Symptoms and laboratory findings were similar to those of ordinary patients, being fever, fatigue, cough, and increased CRP, ESR, and LDH; lymphopenia in some cases and ground-glass opacity on CT consolidation were also similar28.
The differences observed were lower initial severity of opacities, credited to possible reduction in viral load and extent of infection due to careful use of protective equipment such as N95 mask and face screen reducing virus intrusion. In addition, probably greater awareness of symptoms and readiness to perform examinations resulted in less observation of opacifications. Thus the study suggested performing examinations and treatment as early as possible (N19)28.
Finally, study N5, aiming to raise awareness about occupational hand eczema identified a high prevalence of acute hand dermatitis in all professionals regardless of direct patient care with Covid-19 with the intensification of hand hygiene practice due to the pandemic14.
Opportunities for Improvement
Article N1 indicates the need for worker safety management with a system of actions to organize work by seeing the worker's vulnerabilities as a person10. Study N2, meanwhile, drew attention to the possibility of prolonged emotional distress caused by the stress professionals faced during the pandemic, including the risk of post-traumatic stress. The study suggests providing timely counseling services and support systems to mitigate today's damage and its consequences11.
Corroborating the indication of action to reduce stress and its effects over time, several studies point to mental health support actions by maintaining surveillance and monitoring (N4, N6, N7, N9, N10)13)(15)(16)(18)(19.
Promoting resilience as a protective factor was indicated in studies N6, N7, N8 and N11 for stress relief15)(16)(17)(20. With emphasis on social support and keeping in touch with family and friends, as well as fostering support among colleagues for encouragement (N11)20.
Study N4 mentions as coping strategies compliance with infection control procedures, getting enough sleep and exercise. It also highlights resting time as essential13. Sleep hygiene is also mentioned in several articles (N2, N7, and N9), in addition to maintaining a healthy life (N22)11)(16)(18)(31. Study N20 with ICU nurses who presented somatic symptoms also suggested as specific interventions physical exercises and guidelines related to infection control, in addition to behavioral therapy29.
Among the infection control measures, PPE stands out. The lack or rationing of PPE is mentioned as a reason for anxiety and fear. Therefore, several studies recommend the provision of adequate protective material in sufficient numbers for the worker to be safe and thus avoid psychological distress (N7, N12, N13, and N14)16)(21)(22)(23. Furthermore, training on the use and performance of procedures is fundamental for the professional's safety. (N7)16.
Other recommended measures regarding work were: increasing the number of professionals; maintaining teams; maintaining work schedules; and clear and updated guidelines (N22)31. In addition, essential policies for the protection and protection of workers such as work accident insurance benefits for infected workers were encouraged (N11)20.
Furthermore, early detection of contaminated workers facilitates isolation and is important for the protection of health care workers and the community. Thus, studies N4 and N19 recommend attention to symptoms and application of imaging tests promptly13)(28.
Chart 3 allows us to visualize a compilation of the results described by the studies that make up the final sample of this integrative review, as well as the possible solutions. Intervening in grievances requires specific management actions for psychological safety that include assessment, follow-up, and monitoring of the nursing team; preventive measures for occupational health; provision of PPE; improvement of the work environment and promotion of protective factors; promoting education of managers and nurses, as well as expansion of psychological support actions, counseling services, and social support.
Chart 3: Summary of the results and possible solutions described by the studies included in the integrative review. Brasília, Federal District, 2020.

Deveopment: Alves CLM, Aguiar RS, 2020
Finally, study N5 points to the need for greater awareness of occupational hand eczema and preventive measures that can be taken14.
DISCUSSION
The attention to the occupational health of nursing staff should be based on the prevention of diseases and improvement of the level of health of workers.18) To achieve occupational health and productivity, strategies must be used to reduce risks, as well as to ensure that the work environment is improved, sufficient human resources and supplies are allocated, training is provided, and communication and recognition of the worker is promoted30)(31.
Nursing work is known to be heavy and physically and mentally exhausting19. In a pandemic situation especially, it is necessary to take preventive and interventional measures to reduce work-related health risks by providing mental health support, monitoring and interventions during and after the outbreak to prevent prolonged illness and to maintain work capacity16)(24)(31.
Therefore, investments in PPE, training, standardization of procedures, and clear guidelines are necessary for the worker's physical and mental safety and primordial for the promotion of resilience, because they increase the feeling of control over adverse situations17)(19)(29)(31.
Furthermore, the use of systematic analysis of occupational examinations22, the evaluation and monitoring of mental health need to be carried out as strategies for minimizing risks in the practice of workers' management in health institutions. The work environment also needs to be improved, maintaining the conformation of teams, adjusting them to the mode of work and hours according to the workload, not jeopardizing rest, because long shifts and intense work with great wear and tear due to the necessary paramentation, complexity of work and emotional exposure contribute to the exhaustion of the workforce, also putting at risk the safety of patients23)(31.
In addition to these needs, problems with food, transportation, and family provision demand worker social support and humanistic care in order to reduce personal difficulties21)(31.
The nursing worker is in constant and close contact with patients, being witness to their suffering. Thus, it is important to see them as vulnerable people and to adopt psychological support measures with peer support systems and counseling services10)(11)(19.
Therefore, specific permanent actions for the management of the psychological safety of the professionals are necessary for the qualification and improvement of the protection of the worker's health in the scope of the health institutions, and the creation of partnerships with institutions such as class entities may serve as support for the realization of this measure10)(27)(31.
But in addition to training to manage the psychological stress of the nursing worker, it is necessary to reflect on more structural changes regarding the deficiency of basic human, material and equipment resources, pointing to the need for better funding19)(31.
Therefore, by exploring the potential solutions for protecting workers' health and maintaining their working capacity, the articulation between health institutions, class entities, governments and society with the participation of the worker can ease the difficulties of deficit health systems19)(21)(31.
CONCLUSION
From the data obtained in the review, we identify the existence of risk factors and deteriorating conditions of the nursing staff in the Covid-19 pandemic that impact the physical and mental health of the worker, as well as the quality of care offered by these professionals. Aspects involving lack of PPE, training, clear guidelines and protocols, human resources, infrastructure, and psychosocial support were identified.
Moreover, by associating this with the reality of underfunding of some health systems, precarious working conditions are seen as a difficult, complex, and already sickening problem for nursing professionals. Parallel to this, protection factors, resilience and personal accomplishment were identified as positive aspects for the health of the worker, as well as the need to value the recognition of professionals about their work.
Thus, this review suggests the need for recognition of the need for greater protection of the nursing worker in the sense of adopting effective safety measures, because the already precarious working conditions, in a public health emergency situation with increased patient demand and complexity of care are aggravated.
Therefore, short, medium and long term efforts are necessary related to the provision of basic safety conditions and the formulation of public policies for the preservation of workers' health, considering that wear and tear and illness are a reality in nursing work and impact not only on the health of workers, but also on the health of the population they care for.
Regarding the limitations of the study, it is believed to be related to the novelty of the theme, a fact that may have limited the supply of scientific articles in Portuguese about the Brazilian reality.
REFERENCIAS
1. Miranda FMDA, Santana LL, Pizzolato AC, Saquis LMM. Condições de trabalho e o impacto na saúde dos profissionais de enfermagem frente a Covid-19. Cogitare Enferm [Internet]. 2020 [acesso em 25 Set 20];25:e72702. Disponível em: http://dx.doi.org/10.5380/ce.v25i0.72702 [ Links ]
2. Teixeira CFS, Soares CM, Souza EA, Lisboa ES, Pinto ICM, Andrade LR et al. A saúde dos profissionais de saúde no enfrentamento da pandemia de Covid-19. Cien. Saude Colet [Internet]. 2020 [acesso em 25 Set 20];25(9):3465-74. Disponível em: http://dx.doi.org/10.1590/1413-81232020259.19562020 [ Links ]
3. Duprat IP, Melo GC. Análise de casos e óbitos pela Covid-19 em profissionais de enfermagem no Brasil. Rev. Bras. Saúde Ocup [Internet]. 2020 [acesso em 25 Set 20];45:e30. Disponível em: http://dx.doi.org/10.1590/2317-6369000018220 [ Links ]
4. Moraes CCMS, Aguiar RS. A notificação de eventos adversos e suas lacunas no processo da segurança do paciente. Nursing (São Paulo) [Internet]. 2020 [acesso em 25 Set 20];23(271):5025-32. Disponível em: https://doi.org/10.36489/nursing.2020v23i271p5025-5040 [ Links ]
5. Aguiar RS, Silva HS. Segurança do paciente na atenção primária à saúde: uma reflexão teórica. Saúde Colet [Internet]. 2020 [acesso em 25 Set 20];10(59):4442-48. Disponível em: https://doi.org/10.36489/saudecoletiva.2020v10i59p4442-4455 [ Links ]
6. Helioterio MC, Lopes FQRS, Sousa CC, Souza FO, Pinho PS, Sousa FNF et al. Covid-19: por que a proteção da saúde dos trabalhadores e trabalhadoras da saúde é prioritária no combate à pandemia? Trab. Educ. Saúde [Internet]. 2020 [acesso em 25 Set 20];18(3):e00289121. Disponível em: http://dx.doi.org/10.1590/1981-7746-sol00289 [ Links ]
7. Silva LS, Machado EL, Oliveira HN, Ribeiro AP. Condições de trabalho e falta de informações sobre o impacto da Covid-19 entre trabalhadores da saúde. Rev. Bras. Saúde Ocup [Internet]. 2020 [acesso em 25 Set 20];45:e24. Disponível em: http://dx.doi.org/10.1590/2317-6369000014520 [ Links ]
8. Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health [Internet]. 2014 [acesso em 10 Set 20];35:29-45. Disponível em: http://dx.doi.org/10.1146/annurev-pubhealth-032013-182440. PMid:24188053 [ Links ]
9. OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford: Oxford Centre for Evidence-Based Medicine; 2011. Disponível em: Disponível em: https://www.cebm.net/2016/05/ocemb-levels-of-evidence/ [ Links ]
10. Alvarez AKG, Almaguer AYC, Santos EDZ. Gestión de seguridade psicológica del personal sanitário em situaciones de emergência por COVID-19 en el contexto hospitalário o de aislamiento. Rev Cuba Enferm [Internet]. 2020 [acesso em 05 Set 20];36(2):e3704. Disponível em: http://www.revenfermaria.sld.cu/index.php/enf/article/view/3704 [ Links ]
11. Barello S, Palamengui L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professional at the peak of the Italian COVID-19 pandemic. Psychiatry Res [Internet]. 2020 [acesso em 05 Set 20];290:113129. Disponível em: https://doi.org/10.1016/j.psychres.2020.113129 [ Links ]
12. Diomidous M. Sleep and Motion Disorders of Physicians and Nurses Working in Hospitals Facing the Pandemic of COVID-19. Med Arch [Internet]. 2020 [acesso em 05 Set 20];74(3):210-15. Disponível em: https://doi.org/10.5455/medarh.2020.74.210-215 [ Links ]
13. Dong ZQ, Ma J, Hao YN, Shen XL, Liu F, Gao Y et al. The social psychological impacto of the COVID-19 pandemic on medical staff in China: a crosssectional study. Eur Psychiatry [Internet]. 2020 [acesso em 05 Set 20];63(1):e65. Disponível em: https://doi.org/10.1192/j.eurpsy.2020.59 [ Links ]
14. Guertler A, Moellhoff N, Schenck TL, Hagen CS, Kendziora B, Giunta RE et al. Onset of occupational hand eczema among healthcare workers during the SARS-CoV-2 pandemic: Comparing a single surgical site with a COVID-19 intensive care unit. Contact Dermatitis [Internet]. 2020 [acesso em 05 Set 20];26:10.1111/cod.13618. Disponível em: http://doi.org/10.1111/cod.13618 [ Links ]
15. Huang L, Wang Y, Liu J, Ye P, Chen X, Xu H et al. Factors influencing anxiety of health care workers in the radiology departament with high exposure risk to COVID-19. Med Sci Monit [Internet]. 2020 [acesso em 05 Set 20];26:e926008-1-e926008-9. Disponível em: https://doi.org/10.12659/MSM.926008 [ Links ]
16. Jin YH, Huang Q, Wang YY, Zeng XT, Luo LS, Pan ZY et al. Perceived infection transmission routes, infection control practices, psychosocial changes, and management of COVID-19 infected healthcare workers in a tertiary acute care hospital in Wuhan: a crosssectional survey. Mil Med Res [Internet]. 2020 [acesso em 05 Set 20];11(7):24. Disponível em: https://doi.org/10.1186/s40779-020-00254-8 [ Links ]
17. Luceño-Moreno L, Talavera-Velasco B, García-Albuerne Y, Martin-García J. Symptoms of Posttraumatic Stress, Anxiety, Depression, Levels of Resilience and Burnout in Spanish Health Personnel during the COVID-19 Pandemic. Int J Environ Res Public Health [Internet]. 2020 [acesso em 05 Set 20];30(17):5514. Disponível em: https://doi.org/10.3390/ijerph17155514 [ Links ]
18. Magnavita N, Tripepi G, Prinzio RRD. Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey. Int J Environ Res Public Health [Internet]. 2020 [acesso em 05 Set 20];17(14):5218. Disponível em: https://doi.org/10.3390/ijerph17145218 [ Links ]
19. Maraqa B, Nazzal Z, Zink T. Palestinian health care workers' stress and stressors during COVID-19 Pandemic: a cross-sectional study. J Prim Care Community Health [Internet]. 2020 [acesso em 05 Set 20];11:2150132720955026. Disponível em: https://doi.org/10.1177/2150132720955026 [ Links ]
20. Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag [Internet]. 2020 [acesso em 05 Set 20];28(5):1002-1009. Disponível em: https://doi.org/10.1111/jonm.13014 [ Links ]
21. Nasicmento VF, Hattori TY, Terças-Trettel ACP. Dificultades y temores de las enfermeiras que enfrentam la pandemia de COVID-19 en Brasil. Humanidad Med [Internet]. 2020 [acesso em 05 Set 20];20(2):312-333. Disponível em: https://pesquisa.bvsalud.org/controlecancer/resource/pt/biblio-1116227 [ Links ]
22. Nienhaus A, Hod R. COVID-19 among health workers in Germany and Malaysia. Int J Environ Res Public Health [Internet]. 2020 [acesso em 05 Set 20];17(13):4881. Disponível em: https://doi.org/10.3390/ijerph17134881 [ Links ]
23. Rodrigues NH, Silva LGA. Gestão da pandemia Coronavírus em um hospital: relato de experiência profissional. J. Nurs. Health [Internet]. 2020 [acesso em 05 Set 20];10(esp):e20104004. Disponível em: https://doi.org/10.15210/jonah.v10i4.18530. [ Links ]
24. Rossi R, Socci V, Pacitti F, Lorenzo GD, Marco AD, Siracusano A et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open [Internet]. 2020 [acesso em 05 Set 20];3(5):e2010185. Disponível em: https://doi.org/10.1001/jamanetworkopen.2020.10185 [ Links ]
25. Totmann A, Bradley J, Bousema T, Yiek WK, Holwerda M, Bleeker-Rovers C et al. Strong associations and moderate predictive value of early symptoms for SARS-CoV-2 test positivity among healthcare workers, the Netherlands, March 2020 [Internet]. Euro Surveill. 2020 [acesso em 05 Set 20];25(16):2000508. Disponível em: https://doi.org/10.2807/1560-7917.ES.2020.25.16.2000508 [ Links ]
26. Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep distrubances among medical workers during the outbreack of COVID-19. Occup Med (Lond) [Internet]. 2020 [acesso em 05 Set 20];70(5):364-69. Disponível em: https://doi.org/10.1093/occmed/kqaa074 [ Links ]
27. Wong KC, Han XA, Tay KS, Koh SB, Howe TS. The psychological impact on na orthopaedic outpatient setting in the early phase of the COVID-19 pandemic: a crosssectional study. J Orhtop Surg Res [Internet]. 2020 [acesso em 05 Set 20];15:322. Disponível em: https://doi.org/10.1186/s13018-020-01862-9 [ Links ]
28. Xiong Y, Zhang Q, Sun D, Zhu W. Clinical and CT characteristics of health care workers with COVID-19: a single-centered, retrospective study. Medicine (Baltimore) [Internet]. 2020 [acesso em 05 Set 20];99(30):e21396. Disponível em: https://doi.org/10.1097/MD0000000000021396 [ Links ]
29. Yifan T, Ying L, Chunhong G, Jing S, Rong W, Zhenyu L et al. Symptom cluster of ICU nursers treating COVID-19 pneumonia patients in Wuhan, China. J Pain Symptom Manage [Internet]. 2020 [acesso em 05 Set 20];60(1):e48-e53. Disponível em: https://doi.org/10.1016/j.jpainsymman.2020.03.039 [ Links ]
30. Zerbini G, Ebigbo A, Reicherts P, Kunz M, Messman H. Psychosocial burden of healthcare professional in times of COVID-19: a survey conducted at the University Hospital Ausburg. Ger Med Sci [Internet]. 2020 [acesso em 05 Set 20];18. Disponível em: https://doi.org/10.3205/000281 [ Links ]
31. Zhan YX, Zhao SY, Yuan J, Liu H, Liu YF, Gui LL et al. Prevalence and influencing factors on fatigue of first-line nurses combating with COVID-19 in China: descriptive cross-sectional study. Curr Med Sci [Internet]. 2020 [acesso em 05 Set 20];7:1-11. Disponível em: https://doi.org/10.1007/s11596-020-2226-9 [ Links ]
32. Braun V, Clarke V. Using thematic analysis in psychology. Quali Res Psychol [Internet]. 2006 [acesso em 05 Set 20];3(2):77-101. Disponível em: https://dx.doi.org/10.1191/1478088706qp06oa [ Links ]
Received: November 16, 2021; Accepted: January 18, 2022











 texto en
texto en 


