Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.22 no.69 Murcia Jan. 2023 Epub 20-Mar-2023
https://dx.doi.org/10.6018/eglobal.521201
Originals
Evaluation of primary care during the COVID-19 pandemic in a Peruvian región
1Universidad Autónoma de Ica (UAI). Ica, Perú. icapredica@gmail.com
Introduction:
Primary care attention is the fundamental pillar of an effective health system; a failure to comply with its essential attributes could contribute to the collapse of the health systems in the event of pandemics.
Objective:
To evaluate the compliance of the primary attention's attributes and its associated factors, according to the external user's perspective in the context of the COVID-19 pandemic in a Peruvian region.
Method:
Cross-sectional study, which included 1064 randomly selected external users. Also, the sociodemographic and health characteristics were collected using the survey. And the compliance of the primary care attributes was valued using the modified version of the PCAT-A10 instrument. Finally, a descriptive and multivariate analysis was performed using generalized linear models of the Poisson family to evaluate certain factors associated with noncompliance with the attributes of primary care.
Results:
76.6% of the participants perceive that the essential basic attributes are not met; likewise, in the first contact (74.7%), continuity (87.7%), coordination (95.7%), globality (88.3%) and cultural competence (75.9%). The student condition (p<0,001), self-perception of regular health (p=0.010), adult from 30 to 59 years old (p<0.001), and the condition of users of Subtanjalla (p=0.001), Parcona (p<0.001) and Guadalupe (p<0.001) health centers were associated with a greater perception of non-compliance with the attributes of primary health care.
Conclusions:
From the external user's perspective the essential attributes are met in primary care centers; there are factors associated with a greater probability of perceiving that these attributes are not met.
Keywords: Primary Health Care; Comprehensive Health Care; Health System; Pandemic; COVID-19
INTRODUCTION
Primary care (PC) is conceptualized as the provision of unified health services and the access that oversees the sanitary professionals. These professionals are responsible to approach a range of individual health necessities, which has a sustained bond with the patients in a family and community context 1.
In the current context of the sanitary crisis of the COVID-19 pandemic, is necessary to reassess and resume the contributions of Barbara Starfield. Starfield has demonstrated that a strong PC, requires putting into practice its essential attributes (Accessibility, longitudinal continuity of care, coordination, and integrality) 2.
Likewise, it must be considered the primary ideas of the Declaration of Alma-Ata (1978), which are still considered valid. These invoke the necessity of countries to strengthen the PC 3) to guarantee the best sanitary results confirmed in recent studies4.
In Perú, Ministerial Resolution 278-2011/MINSA approves the National plan for strengthening the first level of care 5, and the recent legislation N° 30885 establishes the creation and operation of Integrated Health-RIS Networks 6; in addition, Ministerial Resolution 969-2021/MINSA approves the National plan for the implementation of Integrated Health Networks 7. Although these regulations reflect the efforts aimed at strengthening PC, there are still many challenges and pending gaps.
The COVID-19 pandemic highlighted the precariousness of the health systems. Due to its unpredicTable magnitude, and unique characteristics is responsible for the catastrophic consequences in the community and the breakdown of the sanitary system 8. In the initial stages, health centers and health job positions were closed, care accessibility and continuity of care were limited, and face-to-face care was drastically reduced. Also, preventive-promotional activities stopped, and only emergency and urgent care were available. Only cases of acute respiratory symptoms were treated at the hospital level 9; this reveals the weak implementation of the PC, a fact that could have contributed to the collapse of the sanitary system.
PC centers are in a unique position to manage the health crisis since it has been shown that they can resolve 80% of general morbidity 2,4; therefore, 80% of COVID-19 cases with mild symptoms and without hospital admission requirements 10.
In consequence, there is an urgent need to renew the PC by optimizing its essential attributes 11. These should be considered essential in the process of strengthening the PC strategy 12. In this way, PC evaluation represents a key instrument for the continuous improvement of health quality and allows evidence-based decision-making. Therefore, the study objective was to evaluate the fulfillment of the primary care attributes, according to the external user's perspective in the context of the COVID-19 pandemic in a Peruvian region.
METHOD
Type of study and population
Cross-sectional study, conducted from April to July 2021. The population under study was the external users of the PC centers in a sanitary region (>850 765 habitants), in the province of Ica, Perú. A stratified probability sampling was performed in two stages, in the first stage, 12 health centers were selected and then the proportional sample was assigned to each of these facilities. As a previous step, it was determined an overall sample of 1 064 external users, using the mathematical algorithm for finite populations, a confidence level of 95%, a precision of 3%, and an expected proportion of 50%. The study included adults of both genders, who received outpatient consultation, who were used to going to a health facility in their jurisdiction, who had been referred to a more complex facility, and who agreed to participate in the study. Emergency patients and those who did not agree to participate in the study were excluded.
Variables, instruments, and procedur
The variable compliance with the attributes of primary care (PCCA), is operationally defined as ¨the degree of implementation of PC attributes (accessibility, coordination, continuity, comprehensiveness, and cultural competence), according to the perception of external users of health services. This variable was assessed with the modified version of the PCAT-A10 instrument 13. The Likert-type scale consists of 10 multiple-choice questions: Don't know (0), Not at all (1), Probably not (2), Probably yes (3), and Definitely Yes (4). It also includes four first contact questions (Items 1, 2, 3, and 4), three continuity of care questions (Items 5, 6, and 7), one coordination question (Item 8), globality (Item 9), and cultural competence (Item 10). The scale has a global score of 0 to 40 points, higher scores reflect a good PC performance, and lower scores, a poorer performance. For the present study, it was considered a limit is given by the average score of the global sample + 0.75 times the standard deviation. This to establish that score ≤ 22, means non-compliance with the attributes of primary care (NCAPC); likewise, first contact ≤ 10 points, continuity ≤ 8, and coordination, globality, and cultural competence ≤ 3 points respectively. Higher scores indicate PCCA.
The instrument has not been validated using the information of the Peruvian population; for this reason, minor changes were made to some statements. This proposal was presented to a team of experts formed by three medical professionals with doctorate degrees, who work in PC centers and did not suggest modifications to the instrument's items. Then a pilot test was carried out on 86 external users; as a result of this procedure there were no additional modifications to the items; the internal consistency was adequate with the McDonald Omega coefficient (ω=0,802).
Sociodemographic and health variables were analyzed, such as age, gender, educational level, occupation, type of insurance, self-perception of health, and PC center.
During the execution period of the study, dates and times were coordinated for the collection of the information, and the external users of the jurisdictional area of influence of the PC center were collected outside the health facility. To ensure the quality of the filling out of the form, twelve surveyors were duly trained. Once it was confirmed that the participant met the inclusion criteria, the purpose of the study and its procedures were explained. Then was obtained verbal consent and the hetero-administrated survey was carried out, this survey was filled out by the surveyors, seeking privacy in cases where more than one potential participant was found.
Statistics analysis
Descriptive statistics analysis included frequency measures, percentages, averages, and standard deviation. To evaluate differences, the main variable PCCA was categorized as NCAPC (Yes/No) and Chi-square was used to compare groups between the variable of interest with the sociodemographic and health variables. Generalized linear Poisson family models with logarithmic link function were used to assess certain factors associated with NCAPC. Crude (CPR) and adjusted (APR) prevalence ratios were calculated with their respective 95% CI; those variables with a p < 0,05 in the crude model were included in the adjusted model. For data processing, it was used the ¨Statistical Package for the Social Sciences¨ for Windows version 25.0 in Spanish. A value of p < 0,05 was considered significant.
RESULTS
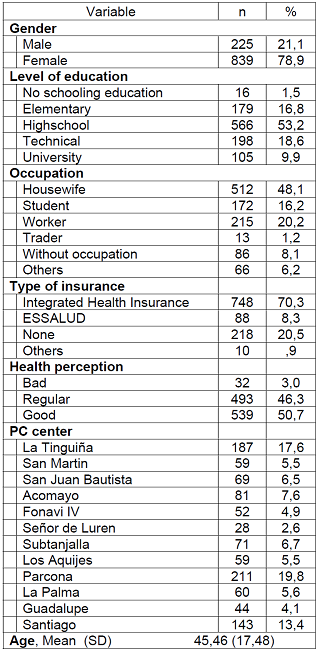
A total of 1,064 users participated, mostly female (78.9%); high school education (53.2%); housewife occupation (48.1%): Integrated Health Insurance (70,3%); self-perception of good health (50,7%); Parcona PC center (19,8%); average age was 45 years (Table 1).
Table 1. Distribution of frequencies, percentages, and descriptive statistics of the socio-demographic, and health variables of the study participants.
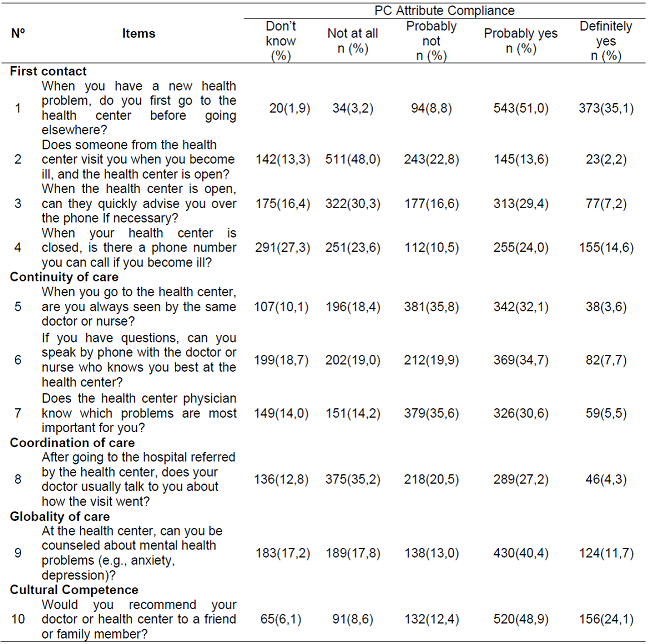
Results reveal that only 35,1% of the external users recognized their primary care center as a gateway to the health system, answering that they will go there when they had a health problem in the future, and 24,1% would recommend their doctor or health center to a friend or relative. The items with the most ¨not at all¨ responses were item 2, referring to the visit of health personnel on the same day if they were ill (48,0%); item 3, on immediate telephone attention, if necessary (30,3%), and item 8, referring to the coordination of care (35,2%) (Table 2).
The mean total score of the PCAT-A10 scale was 17,94 (SD 6,15); a low score indicates the poor performance of the PC during the COVID-19 pandemic. Similar results were revealed for the attributes; first contact 8,13 (SD 3,16), continuity 5,94 (SD 2,37), coordination 1,75 (SD 1,12), globality 2,12 (SD 1,31), and cultural competence 2,76 (SD 1,10).
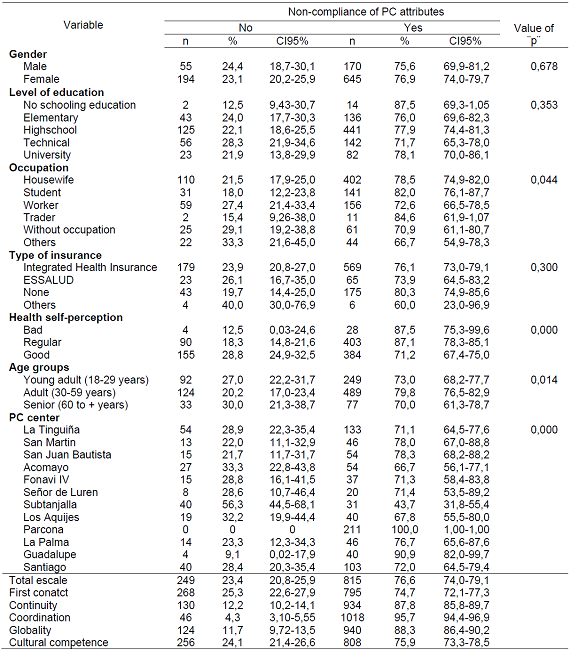
NCAPC was confirmed by 76,6% (CI 95%:74,0-79,1) of the external users, the highest perception of NCAPC was identified by females (76,9%; CI 95%:74,0-79,7), with no education (87,5%; CI 95%:69,3-1,05), and without any type of health insurance (80,3%; CI 95%:74,9-85,6); however, the differences were not significant (p>0,05). In addition, the perception of the NCAPC was higher in traders (84,6%; CI 95%:61,9-1,07), self-perception of poor health (87,5%; CI 95%:75,3-99,6) and regular (87,1%; CI 95%:78,3-85,1) respectively, in adults aged 30-59 years (76,5%; CI 95%:76,5-82,9) and external users of Parcona health center (100%; CI 95%:1,00-1,00), the statistical differences in these groups were significant (p<0,05). (Table 3)
Table 3. Descriptive and bivariate analysis of socio-labor and health variables according to non-compliance with PC attributes in the study sample.
CI95%: Confidence intervals at 95%.
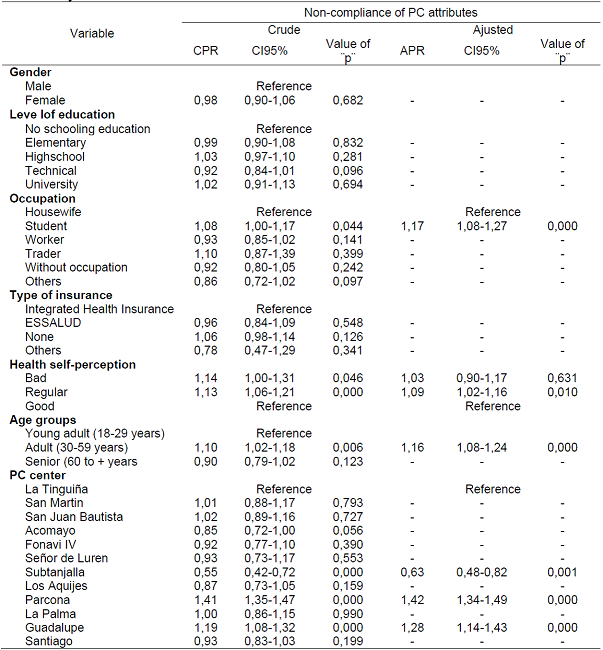
Due to the significant differences found, an adjustment was made using generalized linear models. Associated with greater perception of NCAPC were student status (APR = 1,17; CI95%: 1,08-1,27), self-perception of regular health (APR = 1,09; CI95%: 1,02-1,16), adult between 30 to 59 years old (APR = 1,16; CI95%: 1,08-1,24), and being users of Subtanjalla (APR = 0,63; CI95%: 0,48-0,82), Parcona (APR = 1,42; CI95%: 1,34-1,49), and Guadalupe (APR = 1,28; CI95%: 1,14-1,43) health centers, respectively. (Table 4)
DISCUSSION
The study describes the compliance of PC attributes in a sanitary region of Peru during the COVID-19 pandemic. Low scores were found in the sample of the study, which reveals a non-compliance of PC essential attributes. Seven out of ten external users reported that attributes were not complied with in PC centers, this is a fact that highlights the weaknesses of the health care system during the sanitary crisis. Before the context of the collapse of the health care system, similar results were reported in several studies 14)(15)(16)(17 since PC has had limited development in Latin America and Africa 18.
Although the differences were significant in the perception of NCAPC according to occupation, self-perception of health, age group, and PC center; the adjusted model showed that the student condition, self-perception of regular health, adults from 30 to 59 years old, and users from Subtanjalla, Parcona and Guadalupe health centers, inferred a higher probability of perceiving that PC attributes are not fulfilled. Therefore, these findings suggest redefining policies for the State's stewardship to guarantee the achievement of the ¨salud para todos¨ project.
Likewise, seven out of ten users consider that the accessibility attribute is not fulfilled in PC centers as reported in other studies 14,20. This result reveals that PC centers are not assuming their role as the gateway to the system. This fact could limit the resolution of 80% of general morbidity and promote behaviors aimed at seeking health care in the late stages of the disease. On the other hand, user dissatisfaction has increased in PC centers 21; with repercussions on user loyalty and first contact.
In addition, there is a persistence of a fragmented health care system in Peru, where 47% of SIS affiliates use care centers and health posts as a gateway to the system; affiliates of other insurance companies use hospitals or clinics, and those who are not insured use pharmacies and drugstores 22. Although, significant progress has been made to improve the accessibility attribute 5)(6)(7; there is still a limited investment and low-quality management; which results in an inefficient service that does not respond to the health needs of the population. This generates a crisis in the health sector 23.
Eight out of ten external users perceive that the continuity attribute is not fulfilled and most of them refer that is likely that they will not be attended to by the same physician; similar results were reported in other studies 14,15. Although, health quality management 19 and human capital development 24 are essential elements to guarantee the continuity attribute, some factors such as health personnel rotation, the weakening of the support structures for the Health Quality Management System 25), and user dissatisfaction 21, may have repercussions on non-compliance with the longitudinal continuity of care. Another factor to be considered is the lack of resources in PC (26. Fifty-five percent of the PC centers do not have physicians and operate with other types of professionals and technical assistance 27. However, in recent years, significant progress has been made in the development and human capital (HC) management in Peru. Nevertheless, the allocation of human capital in the first level of care (FLC) continues to be a challenge and an obsolete provisional model persists, which has repercussions on the PC's poor functioning 24. There is an urgent need to formulate and develop a National human resources plan to guarantee adequate coverage of health care workers in PC centers 19. Having HC capable of responding to the health demands and needs of the population is a sectoral priority.
The care coordination attribute is perceived by nine out of ten external users as not very efficient and timely, its non-compliance evidence the limitation of its implementation. Similar results were found in other studies 14)(15)(28. There are important initiatives in Peru 29; that need to be strengthened to improve the coordination between the different levels of care. This improvement is made through the effective exchange of information between service providers, facilitating an adequate flow of information for integral patient care 30. It is necessary to implement an adequate information system that allows the coordination of health care at the different levels of the system. A good initiative would be to strengthen the implementation of an integrated information system within the Integrated health services network, increase the local management capacity, and have equiTable and sustainable finance 7.
The globality of care attribute is considered as the approach to mental health in the current times of pandemic. According to the perception of almost nine out of ten users, this attribute is not met which is consistent with findings from other studies 14)(15)(30. Although compliance may be limited by the deficient physician training for the PC, the scarce assignment of a psychologist to PC centers, financial resources, and the overload of care; it is necessary to bet on a strengthened PC, and provide it with the necessary resources, and give the leadership that requires and deserves 31. It is considered convenient to redirect the supply of health services and guarantee a range of services at the first care level, in, to solve the most frequent health problems of the population, such as physical and psychological sequelae of COVID-19.
Finally, seven out of ten users report that the cultural competence attribute has not been met, therefore, they would not recommend their physicians or health center to a friend or relative; this finding is consistent with studies that report high levels of dissatisfaction in PC centers, in the current context of the health crisis 21. Although the COVID-19 pandemic represents an opportunity to improve PC's attributes, it is essential to have social participation in public management, to position PC at the decision-making Table as a priority, and the role of the university in training, university extension, and research in PC an operative level, and a change in the attitude of basic PC teams.
The limitations of the study include the lack of similar research in the current context of the health crisis, which made it difficult to make comparisons. However, this can be also considered a strength since the study is the first of its kind to address this problem in times of pandemic. A casual relationship was not established; nevertheless, characterizing and comparing the study variable is important because it allows us to identify and address specific needs in the analyzed groups. Therefore, future research is required to search for new explanatory variables associated with NCAPC. On the other hand, the reduced 10-item scale could present limitations to assess the different PC attributes, as does the original extensive version. However, several countries have adopted the PCAT in reduced versions, showing strengths, given its applicability as a short instrument; useful content in the current context, accessibility to services, coordination between levels of care, and mental health care from PC are essential priorities.
FINDINGS
From the population's perspective, PC attributes are unfulfilled. This situation reveals weaknesses in the PC functioning, which could have contributed to the collapse of the health care system during the COVID-19 pandemic. There is an urgent need to renew or strengthen policies aimed to improve PC-based health systems to successfully address current health problems and future pandemic events.
REFERENCIAS
1. Donaldson MS, Yordy KD, Lohr KN, Vanselow NA. Primary Care: America's Health in a New Era. Washington, DC: National Academy Press; 1996. [ Links ]
2. Starfield B. Is primary care essential? Lancet. 1994;344(8930):1129-33. [ Links ]
3. OMS. Informe sobre la salud en el mundo 2008: La atención primaria de salud más necesaria que nunca. Ginebra: OMS; 2008. [ Links ]
4. Schäfer WLA, Boerma WGW, van den Berg MJ, De Maeseneer J, De Rosis S, Detollenaere J, et al. Are people's health care needs better met when primary care is strong? A synthesis of the results of the QUALICOPC study in 34 countries. Prim Health Care Res Dev. 2019; 20(e104). Disponible en: https://pubmed.ncbi.nlm.nih.gov/32800009/ [ Links ]
5. Ministerio de Salud. Plan Nacional de Fortalecimiento del Primer Nivel de Atención 2011-2021 [Internet]. Lima: Dirección General de Salud de las Personas; 2011 [citado el 21 de febrero del 2022]. Disponible en: http://bvs.minsa.gob.pe/local/minsa/1620.pdf [ Links ]
6. Perú, Ministerio de Salud. Ley N°30885, Ley que establece la conformación y el funcionamiento de las Redes Integradas de Salud. Lima: MINSA; 2018. [ Links ]
7. Ministerio de Salud. Resolución Ministerial N° 969-2021-MINSA: Plan Nacional de Implementación de Redes Integradas de Salud [Internet]. El Peruano. 29 de julio del 2021. [citado el 21 de febrero del 2022]. Disponible en: https://www.gob.pe/institucion/minsa/normas-legales/2046143-969-2021-minsa [ Links ]
8. Becerra-Canales BD, Becerra-Huamán D. Inteligencia Consciencial en adultos peruanos en tiempos de pandemia por COVID-19. Rev. cuba. enferm. 2021; 37: e4117. [ Links ]
9. Ministerio de Salud. 2020. RM Nº 95-2020/MINSA: Documento técnico: "Plan Nacional de Reforzamiento de los Servicios de Salud y Contención del COVID-19". Disponible en: https://cdn.www.gob.pe/uploads/document/file/568975/RM_095-2020-MINSA.PDF [ Links ]
10. McIntosh K. Coronavirus disease 2019 (COVID-19). UpToDate. Febrero 2020. (Citado el 24 de febrero del 2022). Disponible en: https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19 [ Links ]
11. Batalla C, Gené J, Mascort J. ¿Y la Atención Primaria durante la pandemia? Aten Primaria. 2020;52:598-9. [ Links ]
12. Solera-Albero J, Tárraga-López PJ. La Atención Primaria de Salud: Más necesaria que nunca en la crisis del coronavirus. JONNPR. 2020;5:468-72. [ Links ]
13. Rochaa K, Rodríguez-Sanzb M, Carme S, Pasarín I. Evaluación de la atención primaria, versión modificada del instrumento PCAT-A10. Aten Primaria. 2020;53:3-11. Disponible en: https://www.sciencedirect.com/science/article/pii/S0212656719303786 [ Links ]
14. Almeida F, Sousa A, Caniçali C, et al. Evaluación de los atributos de la atención primaria en la perspectiva de las usuarias que experimentan el cuidado. Rev. Latino-Am. Enfermagem 2015;23:553-9. Disponible en: https://www.scielo.br/j/rlae/a/mMQNVVTvsQQcfCfGvmBcfnP/?lang=es [ Links ]
15. Araujo JP, Viera CS, Oliveira BRG, Gaiva MA, Rodrigues RM. Assessment of the essential attributes of Primary Health Care for children. Rev Bras Enferm. 2018;71:1366-72. Disponible en: https://www.scielo.br/j/reben/a/46TyRwg84HzMRVmKsSTDv5d/?format=pdf&lang=en [ Links ]
16. Rebelo A, Aparecida R, Carvalho E. Coordinación y longitudinalidad del cuidado en la atención primaria de salud en la Amazonia brasileña. Rev Bras Enferm. 2020;73:e20180841. Disponible en: https://www.scielo.br/j/reben/a/t3zBZDr4F7RYBwyZXWH6w5s/abstract/?lang=es [ Links ]
17. Araujo M, Seabra M, Castello M, et al. Evaluación de la calidad de los servicios de Atención Primaria de Salud en São José de Ribamar, Maranhão, Brasil. Artigos-Interface 2020; 24 (1) Disponible en: https://doi.org/10.1590/Interface.190628 [ Links ]
18. Bitton A, Fifield J, Ratcliffe H, Karlage A, Wang H, Veillard JH, et al. Primary healthcare system performance in low-income and middle-income countries: a scoping review of the evidence from 2010 to 2017. BMJ Glob Health. 2019; 4(Suppl 8):e001551. Disponible en: https://gh.bmj.com/content/4/Suppl_8/e001551 [ Links ]
19. Ugarte-Ubilluz Ó. Gobernanza y rectoría de la calidad en los servicios de salud en el Perú. Rev Peru Med Exp Salud Publica. 2019;36(2):296-303. Disponible en: http://dx.doi.org/10.17843/rpmesp.2019.362.4495. [ Links ]
20. Cuba-Fuentes M, Jurado G, Estrella E. Evaluación del cumplimiento de los atributos de la Atención Primaria y grado de satisfacción de los usuarios de un esTablecimiento de primer nivel de atención. Rev Med Hered. 2011; 22:4-9. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1018-130X2011000100002 [ Links ]
21. Becerra-Canales B, Pecho-Chávez L, Gómez-León M. Satisfacción del usuario externo en un esTablecimiento de atención primaria, durante la pandemia COVID-19. Rev Méd Panacea. 2020;9:165-170. Disponible en: https://revistas.unica.edu.pe/index.php/panacea/article/view/369 [ Links ]
22. Ypanaqué-Luyo P, Martins M. Uso de los servicios de salud ambulatorios en la población peruana. Rev Peru Med Exp Salud Pública. 2015;32:464-70. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1726-46342015000300008 [ Links ]
23. Ineficiencias del sector salud están afectando a millones de peruanos [Informe][En línea]. Perú: Perú 21; 2018. [Citado el 28 de febrero del 2022] URL disponible en: https://peru21.pe/peru/situacion-salud-peruineficiencias-sector-afectando-millonesperuanos-396225 [ Links ]
24. Inga-Berrospi F, Arosquipa Rodríguez C. Avances en el desarrollo de los recursos humanos en salud en el Perú y su importancia en la calidad de atención. Rev Peru Med Exp Salud Pública. 2019;36(2):312-8. Disponible en: http://dx.doi.org/10.17843/rpmesp.2019.362.4493. [ Links ]
25. Becerra-Canales B, Condori-Becerra A. Satisfacción de usuarios en hospitales públicos: experiencia del plan "Cero Colas" en Ica, Perú. Rev Peru Med Exp Salud Pública. 2019;36:658-63. Disponible en: https://rpmesp.ins.gob.pe/rpmesp/article/view/4299 [ Links ]
26. Ministerio de Salud del Perú. Registro Nacional de Personal de la Salud 2016. Información de Recursos Humanos en Salud. Lima: Ministerio de Salud. Dirección General de Personal de la Salud. 2016. (Citado el 12 de marzo del 2022). Disponible en: http://bvs.minsa.gob.pe/local/MINSA/4041.pdf [ Links ]
27. Superintendencia Nacional de Salud [Internet]. Registro Nacional de Instituciones Prestadoras de Servicios de Salud - RENIPRESS. (Citado el 13 de marzo del 2022). Disponible en: https://tinyurl.com/y8yawbjg [ Links ]
28. Lizana M, Flores E, Carhuayo-Luján S. Evaluación de los atributos de atención primaria de salud en establecimientos del primer nivel atención de Ayacucho, Perú. Rev Med Hered. 2020; 31: 175-80. Disponible en: https://revistas.upch.edu.pe/index.php/RMH/article/view/3807 [ Links ]
29. Ministerio de Salud del Perú. Norma Técnica N° 018-MINSA/DGSP-V01: Norma Técnica del Sistema de Referencia y Contrarreferencia de los Establecimientos del Ministerio de Salud. Resolución Ministerial N° 751-2004/MINSA. (Citado el 18 de marzo del 2022). Disponible en: https://tinyurl.com/yc9ctam3 [ Links ]
30. Cuba-Fuentes M, RomeroAlbino Z, Dominguez R, Rojas L, Villanueva R. Dimensiones claves para fortalecer la atención primaria en el Perú a cuarenta años de Alma Ata. An Fac med. 2018:79:346-50. Disponible en: http://www.scielo.org.pe/pdf/afm/v79n4/a13v79n4.pdf [ Links ]
31. Minué Lorenzo S. Contra el coronavirus, más Atención Primaria que nunca. AMF 2020. (Citado el 22 de marzo del 2022). Disponible en: https://amf-semfyc.com/web/article_ver.php?id [ Links ]
Received: April 17, 2022; Accepted: July 11, 2022











 texto em
texto em