My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.22 n.70 Murcia Apr. 2023 Epub June 26, 2023
https://dx.doi.org/10.6018/eglobal.541411
Originals
Evaluation of computed tomography and pulmonary SOFA score: relationship of findings in patients with covid-19 and mortality in ICU
1Nursing student at the State University of Ponta Grossa – Paraná – Brazil
2 Department of Nursing of the State University of Ponta Grossa – Paraná – Brazil
Objective:
To evaluate the pulmonary severity of COVID-19 patients throug the SOFA score computed with pulmonary involvement in Chest Computed Tomography.
Method:
This is a descriptive epidemiological study conducted out in an Intensive Care Unit, which aimed to study the pulmonary treatment of COVID-19 patients through the calculation of the pulmonary SOFA score relating to Chest Tomography and whether these were related to clinical treatment.
Results:
The study population consisted of 704 patients, of which 43.7% were women and 56.2% men, with a mean age of 61 years and a mean hospitalization time of 13 days. Most patients had a pulmonary behavior of 75%, a pulmonary SOFA score of 2 and a PaO²/FiO² ratio between 100 and 200.
Conclusion:
Patients who had more extensive pulmonary involvement/consequently had a lower PaO²/FiO² ratio and remained longer hospitalized with a higher incidence of death.
Keywords: COVID-19; Tomography; Organ Dysfunction Scores; Intensive Care Units; Nursing
INTRODUCTION
The COVID-19 pandemic had its first case at the end of 2019 in China, and by July 2022 there were 547,779,738 cases and 6,336,486 deaths worldwide, with 32,358,018 cases and 671,416 deaths registered in Brazil1. The literature highlights the higher prevalence of mortality among men2, people aged 60 years or older and with risk factors such as diabetes, hypertension, obesity and smoking3.
The damage caused by Sars-CoV-2 occurs by the infiltration of TCD4, TCD8 and macrophages in the interstitium, in the bronchiolar margins of the lungs and the presence of fibrin in the alveolar spaces that injure the tissue through fibrosis, degeneration, congestion and dilation of capillaries , leading to hypoxemia and respiratory failure where some of the individuals affected by the infection require intensive care and are admitted to Intensive Care Units (ICU) (4-6.
One of the diagnostic technologies used in ICU care is the Sequential Organ Failure Assessment (SOFA) Score. It predicts mortality risk by assessing organ dysfunction of six systems. It has been validated and widely used for diagnostic support in Covid-197. The increase in the SOFA score of patients with Covid-19 in the first 48 hours may suggest an increase in the mortality rate.
Even though the SOFA score is important in the diagnosis, chest Computed Tomography (chest CT) (7 represents the gold standard in the clinical evaluation of hospitalized and symptomatic patients(5). Findings on chest CT are similar to those of pneumonia, with bilateral, inferior and peripheral ground glass, making it possible to quantify the extent of pulmonary involvement and allow adequate intervention8.
Another important clinical assessment is the PaO2/FiO2 ratio. It demonstrates the amount of inspired air through the inspiratory fraction of oxygen (FiO2), which, upon reaching the alveoli, undergoes hematosis and is diffused through the blood and can be quantified through the arterial pressure of oxygen (PaO2)9. This clinical evaluation highlights the need for a rapid intervention in patients with Acute Respiratory Failure (ARF), especially due to COVID-19, with a rapid management that impacts the morbidity and mortality of patients with COVID-1910.
In view of the evidence presented and the emerging demands facing COVID-19, researchers from a Brazilian public university began innovative work involving the correlation between diagnostic support technologies (SOFA score, chest CT and PaO2/FiO2 ratio) to guide decision-making clinic with people affected by the disease.
In view of these aspects presented, it is observed that COVID-19 patients require continuous evaluation, which is essential for decision-making regarding the care of these patients, but there is little literature on the evaluation of the SOFA score, chest CT and the PaO2/FiO2 ratio, which is an important care and research gap.
No materials were found in the available literature that expressed this theme, thus establishing a relevant gap that deserves to be better explored. Therefore, this research aims at evaluating the pulmonary severity of COVID-19 patients through the correlation of the pulmonary SOFA score with pulmonary involvement in Chest Computed Tomography.
METHOD
This is a retrospective, analytical and descriptive epidemiological study, carried out in five COVID-19 ICU at a University Hospital in Paraná - Brazil. This institution was a reference in the care of patients with COVID-19, with exclusive care from the Unified Health System (SUS). Its insertion as a health service covers 12 municipalities with an estimated population of 564,453 inhabitants, belonging to the eastern macro-region and linked to the 3rd Health Region of Paraná-Brazil11.
The inclusion criteria for this investigation were: suspected and confirmed patients admitted to the ICU due to COVID-19, over 18 years old, with chest CT and arterial blood gas analysis performed in the first 24 hours of hospitalization. Incomplete data in the clinical history were considered an exclusion criterion.
Data collection was carried out between November 2021 and March 2022 and sampling was by convenience. The extent of pulmonary involvement was assessed using chest CT reports in accordance with the Expert Consensus of the North American Society of Radiology8), using the institution's electronic medical record system. For this tomographic analysis of the pulmonary involvement, the extension was evaluated and classified as 25%, 50%, 75% and 100% of involvement.
Subsequently, the patient's clinical history was evaluated using the electronic medical record system, with the calculation of the pulmonary SOFA score, the PaO²/FiO² ratio using the PaO²/FiO²x100 formula, and the clinical evolution of this population.
The following independent variables were analyzed: gender, age, date of admission and discharge, days of hospitalization, diagnosis in relation to COVID-19, which can be suspected or confirmed by RT-PCR (polymerase chain reaction with reverse transcription) and the variables dependent: pulmonary SOFA score, pulmonary involvement and PaO²/FiO² ratio.
Quantitative data were first collected using a specific instrument and organized into a spreadsheet in the Microsoft Office Excel 365® program and subsequently statistically analyzed. To test the association between the variables, a non-parametric analysis was performed using the Kruskall-Wallis test, ANOVA and Bonferroni. Results where p < 0.05 were considered statistically significant.
This research obeyed the ethical precepts of research with human beings, being approved by the Research Ethics Committee, CAAE nº 31524820.9.0000.0105.
RESULTS
The study population consisted of 704 patients, of whom 43.7% were female and 56.2% were male. The patients' ages ranged from 21 to 98 years with a mean age of 61 years. The length of stay ranged from 1 to 183 days with an average of 13 (±0.60) days.
The study population consisted of 87.78% of COVID-positive patients, and this group represented 89.42% of the 25% involvement, 84.42% of the 50% involvement, 89.53% of the patients with pulmonary involvement 75% and 83.33% of patients with 100% involvement with a p-value of 0.49. It was identified in this study that 26.9% of patients were on MV during the first 24 hours of admission and 67.9% evolved to MV during hospitalization, resulting in a death rate of 54.1%.
Pulmonary involvement of 25% represents 14.7% of the cases, involvement of 50% represents 32.8%, involvement of 75% represents 51.5% and 100% of pulmonary involvement means 0.8% of the cases studied. When analyzing pulmonary involvement by CT, correlating with age, a p-value of 0.28 was obtained, that is, there was no statistical significance when associated to age and pulmonary involvement.
When comparing sex and pulmonary involvement, it was found that there was no statistical significance, with a p-value of 0.55, that is, pulmonary involvement was not related to the gender of patients admitted to this ICU COVID-19.
The second variable, the pulmonary SOFA, results from 0 to 4, with score 0 representing 2.4%, score 1 representing 5.6%, score 2 representing 67.9%, score 3 representing 9.0% and score 4 represents 14.9% of the cases, and the mean pulmonary SOFA found was 2.28.
The PaO²/FiO² ratio ranged from 24 to 686, results lower than 100 represented 32.9%, from 100-200 represented 40.9%, results among 200-300 represented 17.9%, those among 300-400 represented 5.9% and those greater than 400 accounted for 2.1%.
In Table 1 below, the relationship between the extent of pulmonary involvement and the gender of the participants is verified, with a p-value of 0.55, that is, there was no statistical significance when relating pulmonary involvement to gender. Pulmonary involvement of 25% had 44.2% of women and 55.7% of men, involvement of 50% showed 42.4% of women and 57.5% of men, pulmonary involvement with extension of 75% of lungs had 44.3% of women and 55.6% of men and the involvement of 100% showed 50% for each sex.
The relationship between pulmonary involvement and age obtained a p-value of 0.28, also not showing statistical significance in relation to age and pulmonary involvement. The mean age according to the pulmonary involvement can also be seen in Table 1, with the pulmonary involvement of 25% having an average of 65 years, the involvement of 50% of 62 years, the pulmonary involvement of extension of 75% with an average of 59 years and that of 100% an average of 56 years of age. It is observed that the greater pulmonary involvement occurred in younger patients.
Table 1. Relationship between pulmonary involvement and gender of patients admitted to the COVID-19 ICU. Ponta Grossa, Paraná, Brazil. 2022.
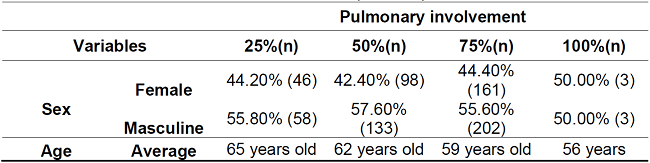
Source: The authors, 2022.
Table 2 shows the relationship between pulmonary involvement, pulmonary SOFA score, length of stay and clinical outcome. The pulmonary SOFA score had a p-value of 0.20 and had a mean of 1.88 for patients with 25% pulmonary involvement, 2.14 for 50% pulmonary involvement, for 75% involvement the mean SOFA score was 2.46 and for patients with 100% pulmonary involvement the mean SOFA score was 3.33.
The initial PaO²/FiO² ratio had a p-value of 0.0001 and showed that the 25% lung involvement had an average PaO²/FiO² ratio of 223.26, the 50% involvement showed an average of 177.94, the lung involvement with 75% extension had an average PaO²/FiO² ratio of 126.43 and 100% an average of 121.83. Pulmonary involvement associated to length of stay had a p-value of 0.0002, pulmonary involvement of 25% demonstrated an average of 10.2 days, patients with involvement of 50% an average of 12.8 days, patients with 75% of the lungs affected an average of 13.9 days and patients with 100% of the lungs affected had an average of 15 days of hospitalization.
45.19% of the patients with 25% of pulmonary involvement, 51.52% of the patients with 50% of involvement, 57.85% of the involvements in 75% and 83.33% of the patients with 100% of involvement died, the p-value being 0.01. In addition, patients who were discharged had a mean lung SOFA score of 2.18 (± 0.83), those who died had a mean lung SOFA score of 2.37 (± 0.89), with a p - value of 0.004.
DISCUSSION
This innovative study, carried out by Brazilian researchers, which involved people affected by COVID-19, identified a correlation between the worst clinical outcomes and even death with high SOFA score, low PaO²/FiO² ratios, greater extent of pulmonary impairment demonstrated on CT chest and longer hospitalization time.
It was found that the majority of hospitalized patients were men with an average age of 61 years. In addition, it was possible to establish a relationship between the increase in the extent of pulmonary involvement with a lower PaO²/FiO² ratio, longer hospitalization and a higher death outcome.
At the beginning of the pandemic, a mortality rate twice as high in men than in women was observed in China and Lombardy in Italy, being associated to pulmonary failure, cardiovascular and acute kidney injury, sepsis, multiple organ failure and thromboembolic events12,13. However, this disparity is not constant and varies between location and time of the pandemic. In some studies, it is suggested that the gender disparity is not large and stable, rather it can be interpreted as modest and varies according to age, ethnicity, occupation, immigration, health behavior and education13.
In the present study, the population studied was 56.2% male, and according to Table 2 (p-value 0.55) pulmonary involvement had a higher percentage among men, except for pulmonary involvement in 100% where men and women had equivalence.
On the other hand, other studies argue that men can die up to three times more than women, explained by premature aging, genetic mechanisms, metabolism, hormonal balance, defense against oxidative stress and immune system function12. In addition, there is the cultural component where poor knowledge and lower adherence to preventive measures are present in the male population compared to women, explaining the higher female survival rate. Another hypothesis defended is the testosterone concentration, since the Angiotensin-Converting Enzyme 2 (ACE 2) is essential for the entry of the virus into the cells, also expressed in the spermatogonia, infecting the testes and potentially producing testosterone. Lower levels of this component can cause damage to the cardiovascular system, impaired immune response, endothelial dysfunction and systemic inflammation12)(13)(14.
Another factor that interferes with the course of COVID-19 is the age of infected patients, in our study the age of patients ranged between 21 and 98 years, with an average of 61 years. Pulmonary involvement was slightly higher among the younger population, demonstrating a reduction in extent as age decreased (p-value 0.28).
Studies conducted in China reveal that people over 60 years of age have shown a higher risk of death when infected. In Italy, 95.3% of deaths were concentrated in the population aged over 60 years. In turn, Brazil shows a lower percentage, 71.4%, this is attributed to the younger age structure and the profile of comorbidities of individuals. The length of stay appears longer among those aged over 45 years, but without association with gender15,16.
As for the length of stay, a retrospective cohort study carried out in southern Brazil, the average length of stay in the ICU was 23 days and the use of MV was 29.5 days. The mean duration of MV among patients who died was 36 days and 20 days for those who survived. Advanced age was the only variable independently associated to the need for MV17. An integrative review carried out shows that the mortality rate among patients on MV found in a previous study was 42.7%, to the detriment of the rate of 54.1% in the present study18.
It is observed that MV can have several consequences when not properly managed, including an indicator of greater probability of mortality. Biotrauma, oxitrauma, atelectrauma, volutrauma and barotrauma may occur as a result of flows, high volume administration and inadequate pressure17. Patients with Covid-19 demonstrate a greater chance of presenting barotrauma on MV compared to patients who do not have Covid-19, generating a vicious cycle between the lungs and the MV, increasing the patient's dependence on this treatment18.
For the diagnosis and understanding of the extent of COVID-19, CT is often used. Its pattern is similar to that of pneumonia, with bilateral, inferior and peripheral peripheral ground glass, other less common findings include bilateral and multilobar nodular or mass-like formations, linear, curved or perilobular opacities and opacities of nonspecific distribution. Some quantitative scoring systems are used to measure pulmonary involvement8.
In the present study, ita was sought to correlate variables with the clinical outcome, including CT, which was used to measure pulmonary involvement. It was found that the 75% rate was the most prevalent in 51.5% of cases and the death rate increased as the extent of pulmonary involvement increased (p-value 0.01).
The literature indicates that the most significant alterations in the image were found in the group symptomatically classified as severe and with a greater chance of death. The opacities progress in extension and attenuation over time, evolving to consolidation that tend to regress after the tenth day. Among patients with the severe form, this does not seem to occur, as the case may not have complete resolution. Consolidation areas are found to be more extensive than those of ground-glass opacity in critically ill patients19,20.
Among the scores used in the ICU to predict mortality is the SOFA score. This score predicts mortality risk and assesses organ dysfunction of six systems, being validated for use in COVID-19. It is calculated on admission and every 24 hours during the stay using the worst parameters measured at the time of calculation and is applied to all patients admitted to the ICU, its score varies from 0 to 4 for each organ system, totaling 24 points. It can be used as an individual score for each organ or in general7. This score is essential to promote the rapid identification of critical cases, to support decision-making in the treatment and prognosis offered to the families of those affected, as well as to allow early intervention for the patient.
The literature is divided when reporting the effectiveness of SOFA for COVID-19. Some studies demonstrate a significant correlation between CT and the admission SOFA, stating that the SOFA is a good tool for predicting the severity and outcome of the disease21. A SOFA greater than or equal to 2 at the time of hospital admission may be a predictor of the need for ICU admission22) and a high SOFA in the first 48 hours may suggest a high mortality rate7. On the other hand, some studies argue that the SOFA was not an adequate score to be used in the ventilatory screening of COVID-19 patients and that a specific score is needed that contains disease-specific variables23.
In our study, the pulmonary SOFA was not significant (p-value 0.20) but it proved to be an effective score to be used for the identification of severe cases and higher death rates, since as the pulmonary involvement increased the mean pulmonary SOFA also increased, with a direct impact on the mortality rate. A parameter used in the calculation of the pulmonary SOFA is the PaO²/FiO² ratio, which is given by the formula PaO²/FiO²x100, which mathematically demonstrates the amount of air inspired by the inspiratory fraction of oxygen (FiO²) that, upon reaching the alveoli, undergoes hematosis and is diffused through of the blood and can be quantified by the arterial oxygen pressure (PaO²)9. The PaO²/FiO² index, especially in an ICU environment, is considered a predictor of adverse outcomes, and results below 300 mmHg were strongly associated to negative outcomes24.
It was found that the PaO²/FiO² ratio had a significant relationship with lung involvement (p-value 0.0001). As lung involvement increased, lung tissue injury occurred through fibrosis, degeneration, congestion and dilation of capillaries, leading to a decrease in the PaO²/FiO² index, hypoxemia and respiratory failure4. In addition, the length of hospital stay was strongly associated with the degree of extension of the pulmonary involvement (p-value 0.0002), and as the pulmonary involvement increased, the length of hospital stay increased.
A retrospective cohort study shows that patients with a smaller extent of lung injury on CT had a mean hospital stay of 21.8 days and the group with a higher degree of pulmonary involvement had a mean of 21.2 days25. Another retrospective cross-sectional study demonstrated a mean length of stay of 10.1 days and a longer length of stay in ICU patients, with high rates of invasive ventilatory support and high mortality26.
In view of the discussion of pulmonary SOFA, the PaO²/FiO² ratio and pulmonary involvement, nursing care for patients with respiratory failure is necessary. An article reporting the clinical case of an adult with respiratory failure due to COVID-19 brings as points of attention the proper management of the airways and identification of obstacles to patient safety. In addition, quality respiratory monitoring allows the early identification of the worsening of the condition and the data can support therapeutic decision-making. Care for respiratory and muscle fatigue is related to COVID-19 because it has a rapid and negative evolution and potentially makes it impossible to perform basic activities of daily living if there is an imbalance in ventilation, breathing and gas exchange, leading the patient to a self-care deficit making attention to these symptoms is essential for the patient's recovery27.
For early identification of morbidity and mortality in COVID-19, the tools used in the present study still need further deepening by Nursing. With regard to CT, the studies mostly deal with the role of Nursing in radiological units as well as the preparation of patients to perform the procedure, but not with the interpretation of images and reports. The nurse based on scientific evidence is competent to read and interpret CT, however, there is still a gap where the professional needs to take over this attribution28.
In turn, SOFA and the PaO²/FiO² ratio are characterized as low-cost, accessible and simple technologies when predicting the chance of illness and mortality in COVID-19. In order for them to be applied, Nursing needs to be able to understand its purpose and way of use, in this way it will allow critical patients to be identified early, since the Nursing team is characterized by being the professional class that most stays at the bedside, and will provide conducts in a timely manner29)(30)(31.
The correlation established between the variables studied can help in the evolution of the condition by supporting medical decision-making and the prognoses provided to the family, acting to improve the quality of care and making early intervention possible for patients, improving the chance of survival. As limitations, mainly incomplete data in medical records and absence of CT on admission are pointed out, which reduced the research sample.
CONCLUSION
This innovative study, which identified, from the analysis of the correlation between the most critical clinical outcomes and even the death of people affected by COVID-19 with the diagnostic support technologies SOFA score, chest CT, PaO²/FiO² ratio, is configured as an important guiding instrument for the clinical practice of ICU teams. The results are promising as they anticipate the clinical evolution and gradually point to positive or negative outcomes throughout the process of pulmonary infection.
In this context, the Nursing team needs to understand the care for respiratory failure, since it is the professional responsible for direct assistance to these patients. In this study, the results made it possible to identify that the SOFA score can help in the decision-making process on predicting clinical outcomes, and can therefore be considered as a tool for directing therapeutic treatment, ensuring a better prognosis and chance of survival for patients with respiratory failure.
REFERENCIAS
1. Johns Hopkins University (JHU). COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). 2022;7594740. Available from: https://gisanddata.maps.arcgis.com/apps/dashboards/bda7594740fd40299423467b48e9ecf6 [ Links ]
2. Maisa Leitão de Queiroz, Hellen Oliveira dos Santos, Milena Monte da Silva E et al. Perfil epidemiológico dos óbitos ocasionados por coronavírus. braz j infect dis. 2021;25(S1):8. [ Links ]
3. Nascimento IMG do, Alencar Neta RL de, Souza AC de, Bezerra YCP, Silva CJS e, Lima ER de, et al. Perfil clínico-epidemiológico dos casos de hospitalização por COVID-19 na nona região de saúde da Paraíba, Brasil. Res Soc Dev. 2022;11(1):e29011124761. [ Links ]
4. Da Silva CC, De Carvalho CMO, De Lima DC, Costa ES, De Andrade VMB, Tenorio BM, et al. Covid-19: Aspectos da origem, fisiopatologia, imunologia e tratamento - uma revisão narrativa. Rev Eletrônica Acervo Saúde. 2021;13(3):e6542. [ Links ]
5. Camila Melo Coelho Loureiro, Juliane Penalva Costa Serra, Bruna Melo Coelho Loureiro, Thais Dourado Matos de Souza, Thiago Meira Góes, José de Souza Almeida Neto, et al. Alterações Pulmonares na COVID-19. Rev Científica Hosp St Izabel. 2020;4(2):89-99. [ Links ]
6. Wu J, Yu J, Zhou S, Zhang J, Xu J, Niu C, et al. What can we learn from a COVID-19 lung biopsy? Int J Infect Dis [Internet]. 2020;99:410-3. Available from: https://doi.org/10.1016/j.ijid.2020.07.067 [ Links ]
7. Andres Chacon Martinez, Nakeya Dewaswala FRTE et al. Validation of sofa score in critically ill patients with covid-1. Chest. 2020;158(4). [ Links ]
8. Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, et al. Radiological society of North America expert consensus document on reporting chest CT findings related to COVID-19: Endorsed by the society of thoracic radiology, the American college of radiology, and RSNA. Radiol Cardiothorac Imaging. 2020;2(2). [ Links ]
9. Brasileiro da Silva V, Castro Ribeiro A. Relação PaO2/FiO2, volume corrente, lactato e prognóstico em sepsis. Rev Bras Pesqui em Saúde/Brazilian J Heal Res. 2021;22(4):137-46. [ Links ]
10. Carvalho EB de, Leite TRS, Sacramento RF de M, Nascimento PRL do, Samary CDS, Rocco PRM, et al. Justificativa e limitações da SpO2/FiO2 como possível substituta da PaO2/FiO2 em diferentes cenários pré-clínicos e clínicos. Rev Bras Ter intensiva. 2022;34(1):185-96. [ Links ]
11. (SESA) Secretaria de Saúde do Estado do Paraná. Macrorrregionais de saúde do Estado do Paraná. Secr Estado da Saúde [Internet]. 2022;1-3. Available from: http://www.saude.pr.gov.br/modules/conteudo/conteudo.php?conteudo=2752 [ Links ]
12. Giagulli VA, Guastamacchia E, Magrone T, Jirillo E, Lisco G, De Pergola G, et al. Worse progression of COVID-19 in men: Is testosterone a key factor? Andrology. 2021;9(1):53-64. [ Links ]
13. Danielsen AC, Lee KM, Boulicault M, Rushovich T, Gompers A, Tarrant A, et al. Sex disparities in COVID-19 outcomes in the United States: Quantifying and contextualizing variation. Soc Sci Med [Internet]. 2022;294 (June 2021):114716. Available from: https://doi.org/10.1016/j.socscimed.2022.114716 [ Links ]
14. López-Romero R, Nambo-Lucio M de J, Salcedo-Carrillo E, Hernández-Cueto M de los Á, Salcedo-Vargas M. The big challenge of SARS-CoV-2 latency: Testes as reservoir. Gac Med Mex. 2020;156(4):328-33. [ Links ]
15. Souza LG, Randow R, Lima PC. Reflexões em tempos de COVID-19: diferenciais por sexo e idade. Comun ciênc saúde [Internet]. 2020;31(suppl.1):1-10. Available from: http://www.escs.edu.br/revistaccs/index.php/comunicacaoemcienciasdasaude/article/view/672/294 [ Links ]
16. Camilla Mandarine Ferreira, Denyse Diomedes Constantino de Almeida, Manuela Lavareda Ayres Drummond de Mattos TK de B de O. COVID 19: Relationship of the epidemiological pattern of COVID-19 between China and Italy. Res Soc Dev. 2020;9(7):e754974840. [ Links ]
17. Bastos GAN, de Azambuja AZ, Polanczyk CA, Gräf DD, Zorzo IW, Maccari JG, et al. Clinical characteristics and predictors of mechanical ventilation in patients with covid-19 hospitalized in southern brazil. Rev Bras Ter Intensiva. 2020;32(4):487-92. [ Links ]
18. Cruz DA, Sousa I de L, Santana PVD, Oliveira LK de A, Sousa FW dos S, Araújo ÁMX de, et al. Impactos da ventilação mecânica invasiva em pacientes de COVID-19: revisão integrativa. Res Soc Dev. 2021;10(11):e380101119656. [ Links ]
19. Pitta LS da C, Hipolito RL, Rocha LC dos S, Sales FM, Silva LPM da, Flores PVP. Alterações tomográficas pulmonares no COVID-19: revisão integrativa da literatura. Res Soc Dev. 2021;10(13):e308101321194. [ Links ]
20. Rosa MEE, Matos MJR de, Furtado RSO de P, Brito VM, Amaral LTW, Beraldo GL, et al. COVID-19 findings identified in chest computed tomography: a pictorial essay. Einstein (Sao Paulo). 2020;18(December 2019):eRW5741. [ Links ]
21. Hejazi ME, Malek Mahdavi A, Navarbaf Z, Tarzamni MK, Moradi R, Sadeghi A, et al. Relationship between chest CT scan findings with SOFA score, CRP, comorbidity, and mortality in ICU patients with COVID-19. Int J Clin Pract. 2021;75(12):1-12. [ Links ]
22. L.M. Vaquero-Ronceroa, E. Sánchez-Barradoa, D. Escobar-Macias E al. C-Reactive protein and SOFA scale: A simple score as early predictor of critical care requirement in patients with COVID-19 pneumonia in Spain. Rev Esp Anestesiol Reanim. 2021;68:513-22. [ Links ]
23. Robert A. Raschke, Sumit Agarwal, Pooja Rangan, C. William Heise MSCC. Discriminant Accuracy of the SOFA Score for Determining the Probable Mortality ofPatientsWith COVID-19 Pneumonia Requiring Mechanical Ventilation. JAMA - J Am Med Assoc. 2021;325(14):1469-70. [ Links ]
24. Sartini S, Massobrio L, Cutuli O, Campodonico P, Bernini C, Sartini M, et al. Role of sato2, pao2/fio2 ratio and pao2 to predict adverse outcome in covid-19: A retrospective, cohort study. Int J Environ Res Public Health. 2021;18(21). [ Links ]
25. Costa dos Santos JP, da Cunha MR, Balchiunas LN, Júnior IJ de C, Garcia NG, Jordan RFR, et al. O Grau De Acometimento Do Parênquima Pulmonar Em Pacientes Covid-19 Está Associado a Maior Tempo De Internação E Necessidade De Ventilação Mecânica? Brazilian J Infect Dis. 2022;26:102043. [ Links ]
26. Nathália Moreir de Almeida França, Gabriella Santos Pinheiro, Larissa Almeida Oliveira Barbosa K de MA. Síndrome Respiratória Aguda Grave por Covid-19: perfil clinico e epidemiológico dos pacientes internados em Unidades de Terapia Intensiva no Brasil. braz j infect dis. 2020;25(S1):35-6. [ Links ]
27. Visallante I, Espejo J, Guerra M. Proceso del cuidado enfermero aplicado en un adulto con insuficiencia respiratoria por COVID-19. Investig e Innov Enfermería [Internet]. 2022;2(1):48-54. Available from: https://revistas.unjbg.edu.pe/index.php/iirce/article/view/1393 [ Links ]
28. Algamdi M, Alghamdi A, Dauod K, Alatawi K, Alrawaili M, Alhwiti M, et al. Nurses' knowledge and practice toward computed tomography safety protocols. Rev Rene. 2022;23:e77891. [ Links ]
29. Cebriano GC y M, Silva DLC da, Ramos LGA, Passos ICGA, Barbosa KLR, Andrade PP de, et al. O enfermeiro como protagonista da identificação precoce da sepse: Cuidados no manejo e evolução do agravo. Res Soc Dev. 2021;10(2):e56010212922. [ Links ]
30. Santos GPG, Costa RMPG, Gouveia MT de O, Fernandes MA. Transições da prática profissional da enfermagem no enfrentamento do novo coronavírus. Enferm em Foco. 2020;11(2.ESP):84-8. [ Links ]
31. Sousa AR de, Santos GLA, Da Silva RS, Carvalho ES de S. Reflexões sobre o Processo de Enfermagem no trabalho de enfermeiras frente à pandemia da Covid-19. Enferm em Foco. 2020;11(1.ESP):62-7. [ Links ]
Received: October 05, 2022; Accepted: January 16, 2023











 text in
text in 



