Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.22 no.71 Murcia jul. 2023 Epub 13-Nov-2023
https://dx.doi.org/10.6018/eglobal.555361
Originals
Influence of Body Mass Index on assisted reproductive techniques
1Virgen del Rocío University Hospital. Andalusian Health Service. Seville. Spain
2Department of Nursing. Faculty of Nursing, Physiotherapy and Podiatry. University of Seville. Seville. Spain
Objective.
To analyze the relationship between the Body Mass Index in women and the results obtained in assisted reproductive techniques.
Methods.
A non-experimental, cross-sectional, descriptive and correlational design was carried out through an analysis of secondary data in several assisted reproduction clinics from Spain. 3,273 medical records of women undergoing In Vitro Fertilization between 2015 and 2018 were analyzed. Data on affiliation and treatment initiation, anthropometric data, personal history, current diseases, primary and secondary infertility, as well as the reference parameters to the results after the assisted reproduction treatment were collected. The statistical analysis was performed using SPSS v19.0 software.
Results.
A total of 798 women (24.42%) had a BMI values ≥ 25. The overweight women achieved a lower number of oocytes retrieved and fertilized, as well as fewer embryos obtained. The women with normal weight achieved a lower number of mature oocytes and those with low weight had a lower fertilization rate.
Conclusions.
It has been found that the results obtained in assisted reproductive techniques are related to women's Body Mass Index.
Keywords: Body Mass Index; Treatment Outcome; Reproductive Techniques, Assisted
INTRODUCTION
Currently, there is a high number of people affected by infertility and/or inability to end a pregnancy with the birth of a healthy child. According to the World Health Organization (WHO), it is estimated that 187 million people are affected by infertility at the global level, of which 10% and 90% suffer from primary and secondary origin infertility, respectively. We speak about primary origin when it is impossible for a woman to get pregnant without resorting to any treatment and about secondary origin when, after a woman gets pregnant without the aid of any treatment, the inability to conceive a new pregnancy without treatment emerges in a given period of time, over twelve months in the case of women up to 35 years old, and six months in those of that age or over(1)-(2). In this sense, Assisted Reproductive Techniques (ARTs) are a set of procedures that have received different names according to time and place, and whose objective is to help people with biological reproductive difficulties to procreate(3). Currently, between 0.2% and 4.3% of the births at the global level are through ARTs(2-4).
Infertile couples should be studied if the women cannot get pregnant after a period lasting between six and twelve months having unprotected sexual relations. However, the study can be initiated earlier in time in women with irregular menstrual cycles or known risk factors for infertility, such as endometriosis, pelvic inflammatory disease history, or malformations in the reproductive system(5). Currently, many infertile couples undergo no treatment, estimating that only 56% of them seek help, with only 22% of these couples receiving medical assistance due to factors such as lack of knowledge about infertility, limited access, treatment cost or social and personal barriers(4).
One of the factors that has been associated with the increase in the number of reproductive disorders is Body Mass Index (BMI) values above 25 kg/m2(6). The mechanism by which this association takes place is complex: on the one hand, adiposity increases the peripheral aromatization function of androgens to estrogens, with a simultaneous reduction in hepatic synthesis of the globulin carrying sexual steroids which, in turn, increase the free estrogen and testosterone levels; and, on the other hand, high BMI values have been associated with increased insulin levels, which stimulates the production of androgens in the ovarian stroma, an indication of deficient reproductive function(7). In addition to considering this association, other signs indicating deficient reproductive function should be taken into account, such as ovulation disorders, reduced conception rate, increased miscarriage rate or other disorders during pregnancy and delivery(6).
The endometrial function can be affected in women with high BMI values (≥ 30 kg/m2), causing a change in uterus receptiveness. Regarding this type of techniques, some authors have mentioned a reduction in the implantation and pregnancy rates(8). In relation to the embryonic factors, it has been shown that oocytes and embryos are negatively affected by maternal overweight or obesity. In these cases, oocytes are smaller when compared to normal weight women(9).
Different studies have mentioned the influence of high BMI values (≥ 30 kg/m2) on the effectiveness of ARTs, describing that they reduce the ovarian response capacity, as the ovarian stimulation periods are extended in time and the necessary gonadotropin dose to induce ovulation is increased. In addition, the number of oocytes obtained when applying the ARTs is lower and they are of less quality when compared to women that present normal weight BMI values(10). Given all of the aforementioned, the objective of the current study has been to analyze the relationship between BMI in women and the results obtained in the ARTs.
MATERIAL AND METHODS
Design and data collection
The study was conducted following a non-experimental, cross-sectional, descriptive and correlational design(11), by analyzing secondary data(12) from 5,651 medical records from several assisted reproduction clinics in Spain.
The inclusion criteria were as follows: 1. Data collected from the medical records of women who attended a consultation to undergo some In Vitro Fecundation (IVF) ART between January 1st, 2015, and February 11th, 2019; and 2. That all the data regarding the study variables were included in the records. The exclusion criteria were the following: Records from women who attended a consultation to undergo any gynecological treatment or ART other than IVF.
Study variables
Dependent variables
The anthropometric variables were weight and height, through which the BMI was calculated. Once these data were collected, they were categorized according to the WHO BMI classification, which is shown in Table 1.
Independent variables
The age of the women subjected to IVF was collected as sociodemographic variable. The clinical variables included in the study were the following: 1. Current personal and disease history, with categorization of the diseases according to their type (gynecological, endocrine, neoplasm, genetic, hereditary, sexually transmitted, mental or others); 2. Data about primary and secondary infertility, which were classified according to their origin (change in seminal quality, genetic causes, ovarian insufficiency, pelvic anomalies, endometriosis, mono/homoparental family causes, ovulation disorders, vasectomy and unknown origin infertility); and 3. Regarding the complementary and laboratory tests, the antral follicle counts were recorded by means of transvaginal ecographies, as well as data on the number of total oocytes retrieved, number of mature oocytes, number of fecundated ovules, fecundation rate and total number of embryos obtained.
Statistical analysis
Data analysis was performed in the SPSS v.19.0 statistical package. For the descriptive analysis, the quantitative variables were characterized by means of centralization and dispersion measures, and the qualitative variables were characterized in frequency and percentage distribution Tables. Normality tests with the Kolmogorov-Smirnov statistics were performed for the quantitative variables. The Kruskal-Wallis test was used for the hypothesis test, establishing those differences with p-values < 0.05 as statistically significant.
Ethical aspects
The study was conducted according to the Declaration of Helsinki (14) and to Organic Law No. 3/2018 of December 5th on Personal Data Protection and guarantee of digital rights (15), ensuring data confidentiality. Favorable ethical report from the Biomedical Research Ethics Portal of Andalusia (Spain) was obtained, with the following internal code: 1432-N-20.
RESULTS
After applying the inclusion and exclusion criteria, a total of 3,273 medical records were analyzed. The mean age of the women was 36.96 years old (σ: 4.23). The mean BMI value was 23.24 (σ: 4.07). In terms of weight, 2,323 (71%) were classified as with normal weight according to the WHO BMI classification (Table 2).
Table 2. Classification of the sample as per the BMI classification according to the WHO.

Source: The authors.
Regarding the previous diseases before applying the ARTs, it was observed that 92% of the women did not present any history of interest. However, histories of gynecological and endocrine diseases were in fact described, with 3% and 2.20% respectively.
Regarding the diseases found when the ARTs were applied, it was observed that 85% of the women did not present any disease of interest. However, the remaining 15% did present them: in the case of women with BMI values ≥ 30 kg/m2, the most frequently mentioned diseases were of endocrine origin, with 8.7%. In the case of women with BMI values < 18.5, it corresponded to gynecological origin in 11.8%, with endometriosis (46.5%), Polycystic Ovarian Syndrome (PCOS) (13.3%) and myomas (5.7%) standing out.
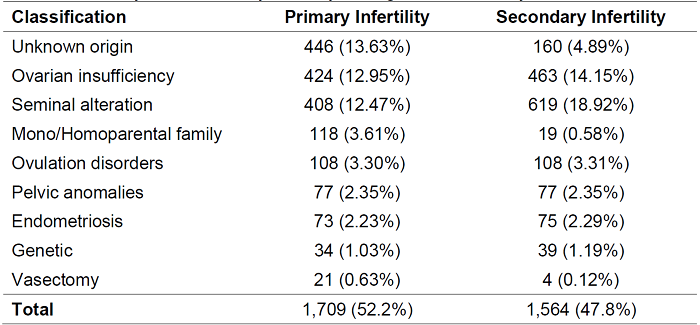
Regarding the type of infertility, 1,709 (52.20%) women had primary origin infertility and, of these, 13.63% were of unknown origin. On the other hand, 1,564 (47.80%) were of secondary origin and, of these, 18.92% were due to seminal alterations (Table 3).
Regarding the follicle counts in the women subjected to ARTs and following the Spanish Society of Fertility (2007) classification (5), we found that 1,600.5 (48.90%) women had low ovarian reserves (Table 4). The mean antral follicle count obtained was 8.36 (σ: 7.98).
Table 4. Follicle count corresponding to the women subjected to ARTs.

Source: Spanish Society of Fertility, 2007 (5).
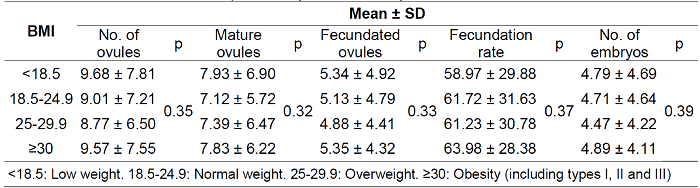
In relation to the complementary and laboratory tests (Table 5), the following results were obtained in the overweight women: number of ovules (8.77), number of mature ovules (7.39), number of fecundated ovules (4.88), fecundation rate (61.23) and number of embryos (4.47).
DISCUSSION
The mean age of the women subjected to ARTs was 36.96 years old, in line with other studies which also assert that there is a reduction in normal fecundation rates after the age of 35 (16).
In relation to BMI, its mean value was 23.24, which corresponds to the normal weight group according to the classification proposed by the WHO. 71% of the sample had normal weight, whereas 24% belonged to the overweight or obesity groups. In this sense, in the study by Chavarro et al. (17) conducted with women subjected to IVF, 65% of them had normal weight and 46% were overweight or obese.
Considering the previous and current diseases among the women participating in this study, 92% had no previous history of interest and 15% presented some diseases causing infertility when undergoing the ARTs, with those of gynecological origin as the most prevalent: 46.5% endometriosis, 13.3% PCOS and 5.7% myomas. Other studies indicate that from 25% to 50% of infertile women have endometriosis and that PCOS is the cause of infertility in more than 27% (18),(19).
Regarding the women who had endometriosis, 2.8% obtained BMI values ≥ 30 (Obesity). In this sense, Liu & Zhang (20) described an inverse association between endometriosis and BMI, where the higher the BMI the lower the risk of suffering endometriosis; however, they indicate that the BMI clinical categories may not provide sufficient etiological information to reflect the nature of obesity.
Regarding the women with PCOS, 19% obtained BMI values ≥ 30. Cui et al. (21) state that between 4% and 6% of the women suffer from PCIS and that half of them have BMI values ≥ 25 (Overweight or Obesity). Other authors have mentioned that 34.63% of the women with PCOS present BMI values above 23 kg/m2 ((5). Nevertheless, other authors indicate that there is no association between PCOS and BMI (22,23).
Regarding the women with myomas, 25% obtained BMI values between 25 and 29.9 (Overweight) and none of them had BMI values ≥ 30, reason why it was not possible to analyze the relationship between obesity and presence of myomas. In this sense, various authors state that there is no relationship between obesity and presence of myomas (24),(25). However, others have described higher risks of developing myomas in obese adults (26,27).
Referring to the type of infertility, higher prevalence of primary infertility was observed in this study, with 52.20% versus 47.80% for secondary infertility. These results are in line with the study by Benksim et al. (28), where the proportion of women affected by primary infertility was also higher (67.37%) when compared to secondary infertility (32.63%).
In the study, 48.9% of the women presented low ovarian reserves, with a mean antral follicle count of 8.36. In the study by Bonilla-Musoles et al. (29), where the antral follicle counts are compared to previous ART failures, it is determined that 49% of the women presented low ovarian reserves, with a mean antral follicle count of 5.7.
In the study, it is observed that the number of total oocytes retrieved (8.77), the number of fecundated ovules (4.88) and the number of embryos (4.47) were lower in the overweight women. However, the number of mature ovules (7.12) was lower in the women with BMI values between 18.5 and 24.9 (Normal weight) and the fecundation rate (58.97) was lower in those with BMI < 18.5 (Low weight).
Regarding the number of total oocytes retrieved, it was lower in the women with BMI values between 25 and 29.9 kg/m2. Leary et al. (9) concluded that the total oocytes retrieved were smaller and of lower quality after applying the ARTs in women with BMI values over 25 kg/m2, presenting lower chances of concluding development after the fertilization process. In this sense, Yang et al. (30) mention that overweight or obese women present lower oocyte recruitment.
Regarding the number of mature ovules, it was lower in the women with BMI values between 18.5 and 24.9 kg/m2. Other authors, such as Chavarro et al. (17), have stated that the short-term weight loss in the women subjected to ARTs was associated with a higher proportion of mature oocytes retrieved, and that this association was higher among the women with BMI values over 25 kg/m2 at the beginning of the study.
Regarding the number of fecundated ovules, it was lower in the women with BMI values between 25 and 29.9 kg/m2. In this sense, in their study, Beydoun et al. examined the effects of BMI on the ART success indicators, not describing significant effects between BMI and the total number of fertilized mature oocytes obtained.
In the results obtained, it is observed that the fecundation rate was higher in women with BMI values ≥ 30. In order to examine if BMI exerts any influence on the IVF results, the study conducted by Orvieto et al. (27) described that the women with obesity presented significantly lower fertilization rates than those who were not obese. However, Sarais et al. (28), who analyzed the effect of BMI on the In Vitro Fertilization results, did not detect statistically significant differences in the fecundation rates across the BMI groups.
Regarding the number of embryos, it was lower in the women with BMI values between 25 and 29.9 kg/m2. Authors such as Sarais et al. have analyzed the effects of BMI on the In Vitro Fertilization results, not detecting statistically significant differences in terms of the number of transferred embryos across the BMI groups. In their studies, Orvieto et al. (27) and Loveland et al. (29) described that an identical number of transferred embryos was obtained in the group of women with BMI values ≥ 25 and in the group with BMI < 25.
Limitations
We found a limitation related to the analysis of secondary data, as the option to collect other data that might be of interest for the research was precluded, such as abdominal perimeter or number of live births, this latter due to the fact that, when a woman got pregnant, she was referred to another specific center for follow-up. However, Munares-García et al. (30) state that, when the data required for a given research study already exist, as in this case, it is not necessary to obtain the same information again.
CONCLUSIONS
The mean age of the women subjected to ARTs was approximately 37 years old, and three out of four had normal weight. More than 90% had no previous diseases and 15% suffered from some disease when the ARTs were applied, mostly of gynecological origin (endometriosis). Slightly more than half of the women presented primary origin infertility (mostly of unknown origin) and slightly less than half of the participants had low ovarian reserves.
Regarding the complementary and laboratory tests, on the one hand, the number of total oocytes retrieved, the number of fecundated ovules and the number of embryos were lower in the women with overweight. On the other hand, the number of mature ovules was lower in the women with normal weight and the fecundation rate was lower in those with low weight.
REFERENCIAS
1. Damario M. General Aspects of fertility and Infertility. Hertfordshire, United Kingdom: Editorial Human Press; 2014. Doi: https://doi.org/10.1016/j.rbmo.2019.10.008. [ Links ]
2. Viera-Molina M, & Guerra-Martín MD. Análisis de la eficacia de las técnicas de reproducción asistida: una revisión sistemática. An Sist Sanit Navar 2018; 41 (1): 107-116. Doi: https://dx.doi.org/10.23938/assn.0254 [ Links ]
3. Bonfill X, & Urrutia G. Análisis y generación de evidencias en reproducción medicamente asistida [Tesis Doctoral]. España, Universidad Autónoma de Barcelona; 2015. https://ddd.uab.cat/pub/tesis/2015/hdl_10803_322783/rbgv1de1.pdf [ Links ]
4. Matorras WR. La infertilidad en España: Situación actual y perspectivas. Madrid: Editorial Imago Concept & Image Development; 2011. https://www.sefertilidad.net/docs/biblioteca/libros/libroBlanco.pdf [ Links ]
5. Matorras R, & Hernández J. Estudio y tratamiento de la pareja estéril: Recomendaciones de la Sociedad Española de Fertilidad. Madrid: Adalia; 2007. https://www.sefertilidad.net/docs/biblioteca/recomendaciones/completo.pdf [ Links ]
6. Brewer CJ, & Balen A. The adverse effects of obesity on conception and implantation. Reproduction 2010;140 (3): 347-364. Doi: https://doi.org/10.1530/REP-09-0568 [ Links ]
7. Levens E, & Skarulis M. Assessing the role of endometrial alteration among obese patients undergoing assisted reproduction. Fertility and sterility 2008; 89 (6):1606-1608. Doi: https://doi.org/10.1016/j.fertnstert.2007.03.079 [ Links ]
8. Luke B, Brown M, Stern J, Missmer S, Fujimoto V, & Leach R. Female obesity adversely affects assisted reproductive technology (ART) pregnancy and live birth rates. Human Reproduction 2011; 26 (1): 245-252. Doi: https://doi.org/10.1093/humrep/deq306 [ Links ]
9. Leary C, Leese HJ, & Sturmey RG. Human embryos from overweight and obese women display phenotypic and metabolic abnormalities. Human Reproduction 2015; 30 (1): 122-132. Doi: https://doi.org/10.1093/humrep/deu276 [ Links ]
10. Ozekinci M, Seven A, Olgan S, Sakinci M, Keskin U, Akar ME, Ceyhan ST, Ergun A. Does obesity have detrimental effects on IVF treatment outcomes? BMC Women's Health 2015; 19 (15): 61. Doi: https://doi.org/10.1186/s12905-015-0223-0 [ Links ]
11. Organización Mundial de la Salud. Obesity: preventing and managing the global epidemic [Internet]. Geneva; 2000. [Citado 03/2020]. Recuperado a partir de: https://apps.who.int/iris/handle/10665/42330 [ Links ]
12. Zegers-Hochschild F, Crosby J, Musri C, Souza M, Martinez G, Silva A, Mojarra J, Masoli D, & Posada N. Assisted reproductive techniques in Latin America: The Latin American Registry, 2017. JBRA Assisted Reproduction 2020; 24 (3): 362-378. Doi: https://doi.org/10.5935/1518-0557.20200029 [ Links ]
13. Chavarro J, Ehrlich S, Colaci D, Wright D, Toth T, Petrozza JC, & Hauser R. Body mass index and short-term weight change in relation to treatment outcomes in women undergoing assisted reproduction. Fertility and Sterility 2012; 98 (1): 109-116. Doi: https://doi.org/10.1016/j.fertnstert.2012.04.012 [ Links ]
14. Pisarska MD, Chan JL, Lawrenson K, Gonzalez TL, & Wang ET. Genetics and Epigenetics of Infertility and Treatments on Outcomes. The Journal of clinical endocrinology and metabolism 2019; 104 (6): 1871-1886. Doi: https://doi.org/10.1210/jc.2018-01869 [ Links ]
15. Liu Y, & Zhang W. Association between body mass index and endometriosis risk: a meta-analysis. Oncotarget 2017; 8 (29): 46928-46936. Doi: https://doi.org/10.18632/oncotarget.14916 [ Links ]
16. Cui N, Wang H, Wang W, Zhang J, Xu Y, Jiang L, Yang A, & Hao G. Impact of Body Mass Index on Outcomes of In Vitro Fertilization/Intracytoplasmic Sperm Injection Among Polycystic Ovarian Syndrome Patients. Cellular physiology and biochemistry: international journal of experimental cellular physiology, biochemistry, and pharmacology 2016; 39 (5): 1723-1734. Doi: https://doi.org/10.1159/000447873 [ Links ]
17. McCormick B, Thomas M, Maxwell R., Williams D, & Aubuchon M. Effects of polycystic ovarian syndrome on in vitro fertilization embryo transfer outcomes are influenced by body mass index. Fertility and Sterility 2008; 90 (6): 2304-2309. Doi: https://doi.org/10.1016/j.fertnstert.2007.10.077 [ Links ]
18. Marquard KL, Stephens SM, Jungheim ES, Ratts VS, Odem RR, Lanzendorf S, & Moley KH. Polycystic ovary syndrome and maternal obesity affect oocyte size in in vitro fertilization/intracytoplasmic sperm injection cycles. Fertility and sterility 2011; 95(6): 2146-2149.e1. Doi: https://doi.org/10.1016/j.fertnstert.2010.10.026 [ Links ]
19. Chiaffarino F, Parazzini F, Vecchia C, Chatenoud L, Di Cintio E, & Marsico S. Diet and uterine myomas. Obstet Gynecol 1999; 94 (3): 395-398. Doi: 10.1016/s0029-7844(99)00305-1 [ Links ]
20. Sparic P, Mirkovic L, Malvasi A, & Tinelli A. Epidemiology of Uterine Myomas: A Review. Fertility & Sterility 2016; 9 (4): 424-435. Doi: 10.22074/IJFS.2016.4599 [ Links ]
21. Lethaby AE, & Vollenhoven BJ. Fibroids (uterine myomatosis, leiomyomas). BMJ clinical evidence 2007: 0814. [ Links ]
22. Parker W. Etiology, symptomatology, and diagnosis of uterine myomas. Fertility & Sterility 2007; 87 (4): 725-736. Doi: https://doi.org/10.1016/j.fertnstert.2007.01.093 [ Links ]
23. Benksim A, Elkhoudri N, Ait Addi R, Baali A, & Cherkaoui M. Difference between Primary and Secondary Infertility in Morocco: Frequencies and Associated Factors. Royan Institute International Journal of Fertility and Sterility 2017; 12 (2): 141-146. Doi: 10.22074/ijfs.2018.5188 [ Links ]
24. Musoles F, Castillo JC, Raga F, Caballero O, Machado LE, Pérez-Panades J, Bonilla F, Dolz M. Valores de hormona antimülleriana (HAM) y recuento de folículos antrales (RFA) en casos con fallo reproductivo previo. Procesos de obstetricia y ginecología 2012; 55 (1): 8-14. Doi: https://doi.org/10.1016/j.pog.2011.08.012 [ Links ]
25. Yang W, Yang R, Lin M, Yang Y, Song X, Zhang J, et al. Body mass index and basal androstenedione are independent risk factors for miscarriage in polycystic ovary syndrome. Reprod Biol Endocrinol 2018; 16:119. Doi: https://doi.org/10.1186/s12958-018-0438-7 [ Links ]
26. Beydoun HA, Stadtmauer L, Beydoun MA, Russell H, Zhao Y, Oehninger S. Polycystic ovary syndrome, body mass index and outcomes of assisted reproductive technologies. Reproductive BioMedicine Online 2009; 18 (6): 856-863. Doi: 10.1016/s1472-6483(10)60037-5. [ Links ]
27. Orvieto R, Meltcer S, Nahum R, Rabinson J, Anteby EY, Ashkenazi J. The influence of body mass index on in vitro fertilization outcome. International Journal of Gynecology & Obstetrics 2009; 104 (1): 53-55. Doi: https://doi.org/10.1016/j.ijgo.2008.08.012 [ Links ]
28. Sarais V, Pagliardini L, Rebonato G, Papaleo E, Candiani M, Vigano P. A Comprehensive Analysis of Body Mass Index Effect on in Vitro Fertilization Outcomes. Nutrients 2016; 8: 109. Doi: https://doi.org/10.3390/nu8030109 [ Links ]
29. Loveland JB, McClamrock HD, Malinow AM, Sharara FI. Increased Body Mass Index Has a Deleterious Effect on In Vitro Fertilization Outcome. Journal of Assisted Reproduction and Genetics 2001; 18 (7): 382-386. Doi: https://doi.org/10.1023/A:1016622506479 [ Links ]
30. Munares-García O, Gómez-Guizado G, Barboza-Del Carpio J, Sánchez-Abanto J. Limitaciones del análisis secundario de bases de datos - Réplica [carta]. Rev Peru Med Exp Salud Publica 2013; 30 (1):152-3. [ Links ]
Received: January 26, 2023; Accepted: April 17, 2023











 texto en
texto en