Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.22 no.71 Murcia Jul. 2023 Epub 13-Nov-2023
https://dx.doi.org/10.6018/eglobal.538111
Originals
Correlation between the care dependence scale of ICU patients and their epidemiological profile
1Graduated in Nursing from the State University of Ponta Grossa – Paraná – Brazil
2Nurse. Doctoral student in Pharmaceutical Sciences from the State University of Ponta Grossa – Paraná – Brazil. Assistant Professor of the Nursing Department of the State University of Ponta Grossa – Paraná – Brazil
3Nurse. Doctor of Science from the School of Nursing of the University of São Paulo – São Paulo - Brazil. Adjunct Professor of the Nursing Department of the State University of Ponta Grossa – Paraná – Brazil
4Pharmacist. PhD in Chemistry from the Federal University of Paraná – Brazil. Associate Professor of the Department of Pharmaceutical Sciences of the State University of Ponta Grossa – Paraná – Brazil
Introduction:
The Intensive Care Unit (ICU) is an environment where critical patients must be treated by a multidisciplinary team. What becomes extremely important to recognize the clinical epidemiological profile to evaluate individually.
Objective:
To analyze the epidemiological profile of patients admitted to an ICU of a University Hospital and its relationship with the Fugulin scale.
Method:
This is a retrospective, descriptive study with a quantitative approach, which carried out an analysis of the epidemiological profile, outcomes and variables associated with morbidity and mortality, through reports of patients hospitalized from March to August 2020.
Results:
It was observed that most of these hospitalized patients were male, referred by the Emergency Medical Care Service, were diagnosed more frequently: acute respiratory failure, sepsis and acute renal failure, with a prevalent outcome in deaths, having been observed correlation of the Fugulin scale with the mortality and severity scores of these patients.
Conclusion:
In view of the complexity in the care of critically ill patients, the study demonstrates that the Fugulin scale can be an alternative in clinical practice, relating the need for care with severity and mortality to patients in an ICU.
Key words: Intensive care units; Organ Dysfunction Scores; Health Profile; Nursing; Critical Care
INTRODUCTION
The Intensive Care Unit (ICU) is a place where critical patients who need to be cared by a multidisciplinary team remain in treatment. In this context, the early recognition of the clinical-epidemiological profile is extremely important so that they can be evaluated individually, aiming at detecting or preventing changes presented in the ICU, as well as identifying the factors that are related to their health status(1).
Regarding to this profile, the vast majority of patients are elderly affected by clinical complications(2). Other characteristics can lead to ICU admission, such as intercurrences during hospitalization, such as admission diagnosis, gender, age, length of stay, morbidity rate, among others(3). These data will help the professional to establish health promotion strategies, minimizing other problems for the next individuals and contributing to the assistance(3).
Thus, in addition to outlining health promotion strategies, critically ill patients need individualized care, as they usually end up triggering prolonged hospitalization (more than 72 hours), which can interfere with their autonomy, generating an unfavorable prognosis or even death(4). So, it is important to evaluate the morbidity and mortality prediction of these patients, relating it to the worsening of hospitalization, resistant microorganisms, insertion of invasive devices, length of stay and use of antibiotics that are related to their care(5).
In this sense, it is essential that nurses use management tools for care planning(6), including the Fugulin scale, which assesses the degree of dependence of patients in the ICU(7). The scale groups categories according to the degree of complexity of care, and it is through this category score that the need for care can be classified according to the priority of the clinical condition(8).
Other tools can be used, such as mortality prognosis, such as the Acute Physiology and Chronic Health Evaluation (Apache IV), which evaluates the level of severity of diseases, using physiological data and stratifying patients into high, medium and low risk for prediction. of mortality(9) and by the Sequential Organ Failure Assessment (SOFA), which indicates the degree of organ dysfunction and morbidity of patients, with special attention to septic conditions(10). It is known that the use of these tools can help in the stratification of certain patients for clinical evaluation, treatment quality and survival results, as well as in the transfer to services of greater or lesser complexity(10).
Faced to these aspects and noting the scarcity of studies on the use of scores to support the need for nursing care for these patients, the following question was asked: Is it important to know the epidemiological profile of patients admitted to the ICU and to evaluate the severity and mortality related to with the dependency of patients in an ICU? This study aimed at relating the epidemiological profile of patients admitted to the ICU with their degree of dependence in a University Hospital in southern Brazil.
METHOD
This is an epidemiological, cross-sectional study that analyzed the epidemiological profile, outcomes and variables associated to morbidity and mortality of patients admitted to an Adult ICU placed in the Eastern Macro-region of the State of Paraná - Brazil. This Study Hospital is strategically placed in the Campos Gerais region, which has around 700,000 inhabitants, and provides medium and high complexity care. The hospital has approximately 153 beds, 20 of which are exclusively for the general ICU, with exclusive care from the Unified Health System (SUS).
As inclusion criteria, ita was used: hospitalization time greater than 96 hours (to evaluate the scores and observe the evolution of the severity and mortality of the patient during the hospitalization period) and age greater than 18 years. The following were excluded: cases of COVID-19 (the institution has a specific ICU to COVID-19, as well as the greater severity of patients and the greater number of professionals), patients readmitted to the ICU and medical records with incomplete data.
Data were selected through the institution's electronic medical record, with the collection of hospitalized patients from March to August 2020. Data collection took place from October 2020 to the end of January 2021. The following data were collected: clinical and sociodemographic characteristics and information from the patient's evaluation and the care provided.
A total of 407 medical records of patients admitted to the Adult ICU during the study period were selected for the investigation, and according to the criteria described, 300 patients were excluded from the sample due to hospitalization time of less than 96 hours or age of less than eighteen years or diagnosed with Covid-19, totaling a final sample of 107 patients.
Data were tabulated in a spreadsheet and later analyzed in statistical software. The Fugulin scale was considered as a dependent variable and sociodemographic and clinical characteristics and evaluation scores as independent variables. After evaluating normality, the ANOVA test was used for categorical independent variables and the Kruskal-Wallis test for non-parametric samples. To evaluate the correlation between the Fugulin Scale variation and the other continuous variables, the Spearman test was applied.
The research was approved by the Ethics Committee for Research with Human Beings, with a Certificate of Presentation for Ethical Assessment in Brazil (CAEE) under number 33662920.2.0000.0105.
RESULTS
Table 1 presents the patients' clinical and sociodemographic characteristics and their relationship to the Fugulin scale performed in the first 24 hours of hospitalization, with an overall mean of 35.09. Among the evaluated variables, the entry point variable (SAMU and others) stands out, in addition to hospitalization due to a diagnosis of acute respiratory failure (ARF), sepsis and acute renal failure (ARF) as criteria for the need for greater attention to highly complex patients.
Table 1. Clinical and Sociodemographic Characteristics in relation to the Fugulin scale in a University Hospital. Ponta grossa. Paraná. Brazil, 2021.

Source: The authors, 2021.
In the complications evaluation that occurred during hospitalization, it was observed that the outcome of death and/or transfer, use of antibiotics, presence of pressure ulcer (PPL) and/or sepsis were factors that influenced the variation in the Fugulin scale (Table 2 ).
Table 2. Intercurrences during hospitalization in relation to the Fugulin scale in a University Hospital. Ponta grossa. Paraná. Brazil, 2021.

Source: The authors, 2021
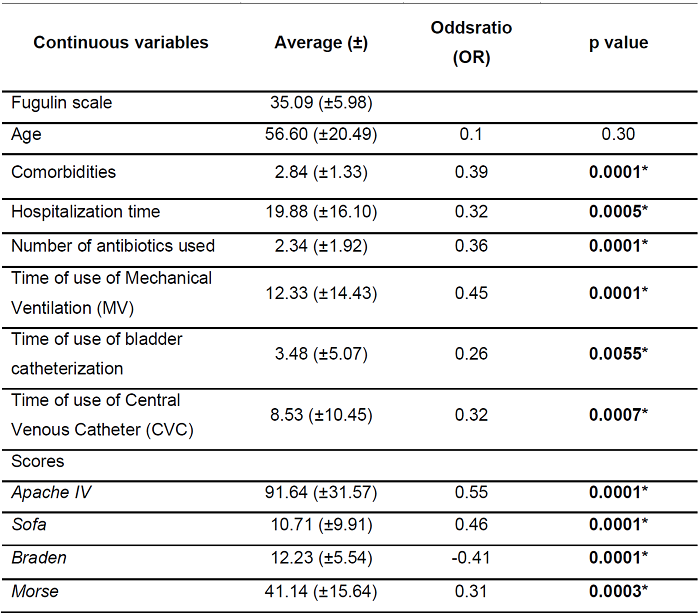
Seeking to analyze the possibility of correlation between the Fugulin need for attention score and the other continuous variables related to the patient's clinical condition, it is observed that some of the variables present inversely proportional changes, such as the Braden scale (signaled by negative Odsratio), where a lower value means a greater risk of PPL, unlike the other scores, where an increased value implies greater severity (Table 3).
DISCUSSION
The ICU remains one of the physical spaces of hospital institutions with the highest absolute and relative number of deaths in the world, even with the artifice of advanced technologies for patient care in bed, since this patient is subjected to prolonged hospitalizations and various invasive procedures. Many of the scores developed were used to evaluate the severity of illness in critically ill patients in order to guide therapeutic interventions(9).
Among the investigations related to characteristics similar to this study, it is noteworthy that ICU in Brazil and around the world, the average admission age is between 50 and 73 years, as described in other similar studies(10,11), corroborating with the age group found. Regarding to gender, there is no significant difference (p=0.76) in both genders, with 55.14% men (fugulin=35.35) and 44.86% women (fugulin=34.77)(12) which demonstrates a percentage of hospitalization between men (22.6%) and women (77.4%), concluding that regardless of gender, it does not interfere with the degree of dependence of the individual's care on the professional.
When evaluating the need for care with the main port of admission for these critically ill patients, it is observed that patients referred by SAMU have a significant difference with greater need for care (fugulin= 36.11 p= 0.01). On the other hand, patients referred from other institutions had less need for care with a significant difference (fugulin= 31.57 p= 0.02).
In this sense, it can be said that the complexity of care required by patients referred from hospital services is greater than that of patients referred from other institutions. A study pointed out that doors such as the Emergency Room and the Surgical Center(13) need more attention, corroborating this study.
In the present study, sepsis (Fugulin = 36.28 p = 0.01) was inferred as the main cause of admission, followed by ARF (Fugulin = 36.30 p = 0.04) and ARFI (Fugulin = 38.6 p= 0.009). Observing other results found(14), contrasting data can be observed, as the main causes with the highest prevalence were postoperative (32%), stroke (14%) and congestive heart failure (13%), followed by sepsis (10%), ARF (8%) and ARI (9%).
Hospitalization in the context of the pandemic could have changed the cause of hospitalizations due to the suspension of elective surgeries for a long time, as well as hospital referral for clinical care.
Along the same lines, when analyzing the number of hospitalization diagnoses and the significant correlation between the increase in the number of diagnoses and the Fugulin scale, it is suggested that patients have a greater need for care according to the increase in pathologies present during hospitalization, however, there are no data in the literature that compare these data.
Regarding to the length of stay in the ICU, the mean of this study was approximately 20 days, with a difference being observed in relation to the length of stay described in the literature (1.15), mean of 11 days and 13 days. In this study, there was a significant correlation between the days of hospitalization and the need for care (p= 0.0005), which suggests an increase in the demand for care as the length of stay of critically ill patients in the ICU increases.
Regarding to the outcome of these patients, the percentage results of this investigation were higher than those of another study(16). There is also a relationship between the outcome and higher Fugulin values at the time of death and transfer (p= 0.05).
The influence of the use of antibiotics on the need for nursing care can be evaluated, with a significant correlation between these (p=0.01), but no studies were found in the literature that addressed this association between the use of antibiotics, demonstrating only the correlation between the classes of antibiotics and the severity of the patients, generating an alert for future evaluations with this perspective of polypharmacy in terms of antibiotic therapy.
When evaluating the use of invasive devices during the ICU stay, it was observed that the days of use of MV (12.22±14.43), permanent bladder catheterization (3.48±5.07) and CVC (8. 53±10.45) correlate with an increase in the Fugulin value (p<0.05), indicating that the days of use of these devices increase the need for care and, consequently, the severity and prognosis of these patients.
A similar study(17) evaluated 277 patients, and the researchers warned about the excessive use of these devices in the ICU environment and the association of the use of devices interferes with the demand for care and infers an increase in Fugulin values, when correlated.
Comparing the Fugulin values with the Morse scale, a correlation is demonstrated between the risk of falls and the need for care, indicating the importance of having a daily monitoring of the risk of falls in patients. In a study(18), this evaluation confirmed the high risk of falls for critically ill patients, with a probable association with the neurological condition and decreased walking. Therefore, the nursing professional has a fundamental role in preventing this event at the bedside, with continuous observation, help with walking and basic care, as well as raising protection rails and guidelines, thus justifying the increase in the demand for care according to the progressive risk of falls.
By evaluating the patients in relation to the Braden scale in this study (12.23 ± 5.54), it was possible to classify them as at high risk for PI. An author(19) observed that patients in intensive care are at high risk of developing PI during their stay in the ICU, which corroborates the average found in this study, which was moderate to severe risk (12). Regarding to the association to the average Fugulin value, there is a significant correlation (ODS= -0.41 and p<0.05), where it is observed that the lowest Braden values (indicating a higher risk of PI) are associated to higher values of Fugulin (greater need for care), confirming the importance and need for continuous and individualized care from the nursing team to these patients in order to prevent and treat PI.
Analyzing this characteristic of high dependence on care by the nursing team for critically ill patients admitted to the ICU, it can be stated that the patients included in this study have a high severity score in the SOFA Score (10.71±9.91), in comparison to another study(20) which highlights the SOFA score of 6.55 (±0.61) points with 117 patients admitted to the ICU. These higher values in the patients evaluated in this study may be related to the characteristics of patients hospitalized with clinical diagnoses, mostly due to the suspension of surgical procedures in the studied ICU caused by the advent of the COVID-19 Pandemic. There is also a strong correlation between the Fugulin scores and the SOFA score (p<0.05), warning that the need for intensive care should be directed towards the most severe patients.
From this same evaluation perspective, when evaluating the APACHE IV for ICU patients (91.64 ± 31.57), higher values than those reported in the literature are observed, as described in a study carried out in a Brazilian state(21) with an average of 75.70 in the APACHE IV and another study carried out in Guatemala(22) obtained an average of 78.27. Therefore, it is suggested that this high predictive profile of mortality may be associated to the profile of the patients studied due to the existence of a global pandemic.
It is also observed that the APACHE IV is correlated with the need for care (Fugulin) (p<0.05), inferring that patients with a higher risk of predictive mortality require a greater demand for intensive care by the nursing team.
Thus, it is noteworthy that this research correlated the assessment of the need for care with mortality and severity, as well as the use of devices and antibiotics, reinforcing and justifying that the use of the Fugulin scale is an essential instrument in clinical practice, subsidizing the nurses diagnose and manage care according to needs, as well as point out to the team, through the Fugulin scale, the most severe patients and mortality prediction.
However, a limitation of this research was the study sample, the evaluation during the pandemic with changes in the profile of hospitalized patients, as well as the scarcity of preliminary studies with a perspective of correlation. Therefore, there is a need for new multicenter studies and with other populations of critically ill patients to support these data and strengthen, for the nursing team, the importance of applying the Fugulin scale in the assessment and management of care based on the needs of the individual/patient.
CONCLUSION
It was concluded that the epidemiological profile of patients admitted to the Intensive Care Unit of the hospital under study was mostly male, white and admitted via SAMU. It was observed that the vast majority used antibiotics and invasive devices and the main outcome was death. Regarding to the evaluation of the Fugulin Scale, values with significant differences were observed when comparing them to patients referred via SAMU or other towns, as well as hospitalized due to ARF, Sepsis or ARI.
Intercurrences during hospitalization that had significant differences in relation to the value of Fugulin were the outcome, use of antibiotics, PI and sepsis.
When evaluating the correlation of the Fugulin Scale with the data obtained in this study, the relationship between the SOFA and APACHE IV scores, as well as the days of use of the devices, is highlighted. It is possible to conclude that, although the studies have some limitations, the model showed good results in relation to predictions, with significant and reliable values in all versions, proving to be a promising alternative in the clinical practice of the entire multidisciplinary team, especially for nurses, who use the Fugulin scale to guide their care, resources and attention to patients admitted to intensive care.
REFERENCIAS
1. Albuquerque JM, Silva RFA, Souza RFF. Epidemiological Profile and Monitoring After Discharge of Patients Hospitalized At an Intensive Care Unit. Cogitare Enferm [Internet]. 2017;22(3):1-9. Available from: http://revistas.ufpr.br/cogitare/article/view/50609/pdf [ Links ]
2. Associação de Medicina Intensiva Brasileira (AMIB). AMIB apresenta dados atualizados sobre leitos de UTI no Brasil. Assoc Med Intensiva Bras. 2020;2507(February):1-9. [ Links ]
3. I AHR, Bettina M, Bub C, I OFP, Ii GZ, Jesús M De, et al. Epidemiological characteristics and causes of deaths in hospitalized patients under intensive care. 210 Rev Bras Enferm. 2016;69(2):210-4. [ Links ]
4. Joice Barbosa Vilas Boas da Silva, Larissa Chaves Pedreira, Jessica Lane Pereira Santos, Cláudia Silva Marinho Antunes Barros, Rose Ana Rios David. Clinical profile of long-living elderly at an intensive care unit Corresponding author. Acta Paul Enferm. 2018;31(1):39-45. [ Links ]
5. Inês Aguiar-Ricardo, Hélia Mateus J, João Gonçalves-Pereira. Hidden hospital mortality in patients with sepsis discharged from the intensive care unit. Rev Bras Ter Intensiva. 2019;31(2):122-8. [ Links ]
6. Andrielly Silva Rufino, Bruna Maria Malagoli Rocha, João Pedro Resende Castro, Juliana da Silva Garcia Nascimento MB da S. Clasificación de los pacientes según el grado de dependencia de enfermería del equipo. Rev Enferm Atenção Saúde [Online] Ago/Dez. 2015;4(2):5-19. [ Links ]
7. Perroca MG, Gaidzinski RR. Patient classification system: construction and validation of an instrument. Vol. 32, Revista da Escola de Enfermagem da U S P. 1998. p. 153-68. [ Links ]
8. Ilana Elen Andrade Mariano Nobre, Lívia Moreira Barros, Maria Laura Silva Gomes, Leonardo Alexandrino da Silva, Isabel Cristina da Silva Lima JÁC. Fugulin patient classification system: medical clinic assistance profile. J Nurs UFPE line. 2017;11(4):1736-42. [ Links ]
9. Keegan MT, Soares M. What every intensivist should know about prognostic scoring systems and risk-adjusted mortality. Rev Bras Ter Intensiva. 2016;28(3):264-9. [ Links ]
10. Denti IA, Julcimara AP, Biasi LS, Manfredini CS. Prognosis of disease severity in patients hospitalized in intensive care units. Perspectiva [Internet]. 2015;145(3):29-39. Available from: http://www.uricer.edu.br/site/pdfs/perspectiva/145_479.pdf [ Links ]
11. Alves GA de A, Martinez BP, Lunardi AC, Alves GA de A, Martinez BP, Lunardi AC. Assessment of the measurement properties of the Brazilian versions of the Functional Status Score for the ICU and the Functional Independence Measure in critically ill patients in the intensive care unit. Rev Bras Ter Intensiva [Internet]. 2019 [cited 2022 May 25];31(4):521-8. Available from: http://www.gnresearch.org/doi/10.5935/0103-507X.20190065 [ Links ]
12. Nogueira P, Hissa G, Rocha M, Hissa N, Ramos De Araújo PS, Original A. Comparative analysis between two scores in predicting mortality in intensive care unit. Rev Bras Clin Med. 2013;11(1):6-21. [ Links ]
13. De Assis LGR, Nery Neto CDS, Santos GS, Dos Santos AW, Silva CHS, Barros JF, et al. Evaluación de la mortalidade en una Unidad de Cuidados Intensivos en Sergipe, según la puntuación fisiológica aguda simplificada (SAPS 3). Rev Epidemiol e Control Infecção. 2020;10(1):1-7. [ Links ]
14. Nascimento MS de M, Nunes EM, Medeiros RC, Souza WIM, Sousa Filho LF, Alves ESRC. Epidemiological Profile Of Patients In Intensive Care Unit Adult Of A Local Hospital In The State Of Paraiba Maria. Temas em Saúde. 2018;18(1):247-65. [ Links ]
15. Guia CM, Biondi RS, Sotero S, Lima A de A, De Almeida KJQ, Amorim FF. Epidemiological profile and predictors of mortality in an intensive care unit in a general hospital in Distrito Federal. Comun em Ciências da Saúde. 2018;26(01/02). [ Links ]
16. Yasmim Y, Anjos F, Vasconcelos N, Marques G, et al. Escores prognósticos à admissão e desfechos de pacientes em unidade de terapia intensiva Prognostic scores for admission and outcomes of patients in a intensive care unit Pontuaciones prognósticas en la admisión y salidas de pacientes en una unidad de. Rev Eletrônica Acervo Saúde. 2019;12(11):1-9. [ Links ]
17. Bergamim Hespanhol LA, Cartonilho de Souza Ramos S, Ribeiro Júnior OC, Silva de AraújoTatiane T, Martins AB, Hespanhol LAB, et al. Infección relacionada con la Asistencia a la Salud en Unidad de Cuidados Intensivos Adulto. Enfermería Glob [Internet]. 2018 Dec 20 [cited 2022 May 25];18(1):215-54. Available from: https://revistas.um.es/eglobal/article/view/eglobal.18.1.296481 [ Links ]
18. Specht AM, Sousa GP de, Beghetto MG. Incidence of falls in a cohort of critical adults: a cause for concerns? Rev Gauch Enferm. 2020;41(spe):e20190167. [ Links ]
19. Carolina Otto, Beatriz Schumacher, Luiz Paulo De Lemos Wiese, Carlos Ferro RAR. Factores De Riesgo Para El Desarrollo De Lesiones Por Presión En Pacientes Críticos. Enferm Foco. 2019;10(1):7-11. [ Links ]
20. Costa RA da. Mortality of patients admitted by sepse in a general icu of a tertiary hospital. Arq Catarinenses Med. 2018;47(4):15-28. [ Links ]
21. de Carvalho GA, Rezende AAB, Reis GR, Gardenghi G. Use of the apache IV score as a predictor of mortality and length of stay in an intensive care unit. Rev Pesqui em Fisioter. 2020;10(1):9-15. [ Links ]
22. Godínez Ortiz LE, Ranero Meneses JL. Predictores de mortalidad en pacientes críticamente enfermos: Correlación de la Escala APACHE II y APACHE IV. Rev med interna Guatem [Internet]. 2017;21(1):7-12. Available from: https://docs.bvsalud.org/biblioref/2019/06/994975/01.pdf [ Links ]
Received: September 05, 2022; Accepted: January 19, 2023











 texto em
texto em