Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.22 no.71 Murcia Jul. 2023 Epub 13-Nov-2023
https://dx.doi.org/10.6018/eglobal.545071
Originals
Effectiveness of a brief intervention on the resilience, mindfulness and empathy of nursing professionals
1Santa Lucía General Hospital, Cartagena, Murcia. Spain
2University of Murcia. Murcia. Spain
3Primary Care, Area 2. Murcian Health Service. Murcia. Spain
5FADE Foundation. Murcia. Spain
Objectives:
Assess the efficacy of a guided intervention based on stress reduction and compassion, related to resilience and compassion fatigue of healthcare professionals.
Methods:
Quasi-experimental study with a control and intervention groups, combining a multimodal intervention delivered in 3 sessions. Control group (n = 23), experimental group (n = 23). Data collection: 4 observations were made using the Brief Resilience Scale, Freiburg Mindfulness Inventory, Compassion Fatigue Inventory and data on the professional profile and personal life. In order to analyze the relationship between variables, a general linear model, the chi-square or Fisher test, and regression analysis were used.
Results:
No significant effect of the evaluated intervention was found on the score obtained in mindfulness, resilience or empathy. The control group obtained a higher score in mindfulness when related to the non-covid work unit and the absence of personal stressors F(1.21)=16.081 p=<0.01, ŋ2=0.434. The normal empathic profile without risk was significantly higher in non-covid units compared to covid units in the first evaluation (70% vs 30%, p=0.002). The profile of low resilience in auxiliary nurses was higher during the last evaluation (72.2% vs 27.8%, p=0.003), a moment in which a greater number of patients were hospitalized with covid.
Conclusions:
A higher influences on professionals psychological wellbeing was present with personal and job related factors (professional category, work place and healthcare pressure) than the intervention carried out.
Key words: Resilience, Psychological; Mindfulness; Compassion Fatigue; Psychotherapy; Stress, Psychological; Nursing
INTRODUCTION
The prevalence of anxiety and other disorders related to mental health in healthcare professionals during the Covid-19 pandemic is well documented. Different projects synthesize the results of more than 400 studies carried out during the 2020-2021 period, and estimate a combined prevalence of sleep-related disorders of 43% (95% CI: 36%-50%) (1), depression of the 27.05% (95% CI: 23.14%-31.36%) (2) and anxiety up to 43% in frontline healthcare workers (95% CI: 25%-62%) (3).
This obvious negative impact that the Covid pandemic has had on healthcare professionals shows an increased interest in identifying effective interventions that improve their psychological well-being. Some studies indicate that increasing health care professional's ability to face adverse situations, through mental flexibility, emotional regulation, adaptive capacity, internal locus of control, etc., could reduce their vulnerability to psychological harm. Strengthening these “resilient traits” can be achieved through very diverse interventions, including organizational changes, psychological support and/or guided or unguided self-help strategies (which in turn include a large number of variants: mindfulness, cognitive behavioral therapy, compassion etc). The duration and organization of said interventions is also diverse and ranges from those that require a single intervention to those that last for six months or longer (4,5).
The synthesis studies point out that the heterogeneity, the scarcity of experimental studies and the methodological deficiencies of those that have been carried out to date are the cause of the lack of firm evidence on the subject. So far, two systematic reviews conducted on frontline healthcare professionals during any infectious disease pandemic or epidemic, and on healthcare professions students reported no evidence, or "limited" and "unclear" evidence on this type of interventions(4,5).
The main objective of this study was to determine the efficacy of a guided intervention based on stress reduction and compassion, on resilience, empathy burnout and mindfulness of healthcare professionals.
METHOD
A quasi-experimental study with a control group, was carried out between July 2021 and February 2022, at the Santa Lucia General University Hospital in Cartagena.The sample size was calculated assuming an alpha risk of 0.05 and a beta risk of 0.2 in a bilateral contrast. The result was that 23 subjects were needed in the control group and 23 in the intervention group to detect a difference equal to or greater than 0.15 units. The common standard deviation was estimated to be 0.21 (6) , and a rate of loss during follow-up of 30%.
Convenience sampling was carried out among Nursing asistants/ Auxiliary Nurses and Nursing professionals from different units. The inclusion criteria were: uninterrupted employment contract from January 2020 to February 2022, and having signed a consent form.The participants were divided into two groups, a control group (CG) and an intervention group (IC). The control group selection was paired with the intervention group, according to variables that could exert a bias if not taken into account: age (± 3 years of difference between groups), work unit, professional category, and years of work experience (± 2 year difference between groups).
The intervention group received the following training: 3 classes lasting four hours each. The first two classes were given in mid-July 2021, and the third class in early November 2021. The training received was mainly made up of a practical component and included content from: the Mindfulness-Based Stress Reduction program (MBSR) and a program that incorporates practices for the cultivation of compassion, the Mindful-SelfCompassion (MSC) program (7).
To assess the impact of the training, 4 observations were made (15 days before the first intervention, 2 months before the third intervention, and another two observations 1 month and 3 months after the third intervention. (Figure 1). The following tools were used for data collection: Brief Resilience Scale (8), Freiburg Mindfulness Inventory (9) and the Compassion Fatigue Inventory (10). In addition, other data related to the work profile and personal life of the participants.
Variables analyzed in the study:
Dependent variables: level of mindfulness (measured according to the Freiburg Mindfulness Inventory), resilience (measured according to the Brief Resilience Scale) and empathy/compassion (measured according to the Compassion Fatigue Inventory). Independent variables: complete training (3 sessions) on stress reduction through Mindfulness techniques and cultivation of compassion, age, sex, professional category (Auxiliary Nurses or Nurse), years of work experience, unit in which they have worked during the pandemic (Covid or non-Covid unit), regular practice of activities that help manage stress (regular physical exercise, yoga, therapy, meditation practice...) and having suffered a stressful event in the last 6 months.
For data analysis, the JAMOVI statistical program was used. For descriptive statistics, qualitative data is expressed with frequencies and percentages, and quantitative data with averages and ± standard deviation. A general linear model was performed, using a factorial ANOVA with repeated measures as a test to analyze the interaction between categorical independent and quantitative dependent variables. Pearson's Chi-square test or Fisher's exact test was used to determine the association between categorical variables, and regression analysis to determine the relationship between quantitative independent variables and dependent variables. A value of p < 0.05 was established as the level of statistically difference.
The project obtained permission from the Research Ethics Committee of the 2nd and 8th Health Areas of the Murcian Health Service, and the consent of all participants was requested. Throughout the research process, the anonymity and confidentiality of the people involved in the research was ensured.
RESULTS
A total of 46 professionals participated in the study, there were no lost participants during follow-up, table 1.
Mindfulness
No significant effect of the evaluated intervention was found on the score obtained in full atención F (1.21)=0.389, p=0.539, ŋ2=0.389, although significant relationships were obtained when the group in which each participant had been assigned was related to the unit / ward and to the previous experience of a stressful event: F (1.21)=16.081 p=<0.01, ŋ2=0.434. Professionals belonging to the control group who worked in non-covid units and who had not previously suffered any stressful event obtained a higher score in mindfulness (M= 44.41, SD=1.85), than those of the intervention group (M=37, 16, SD=1.73), p=0.009. Mindfulness was not significantly related to any other variable.
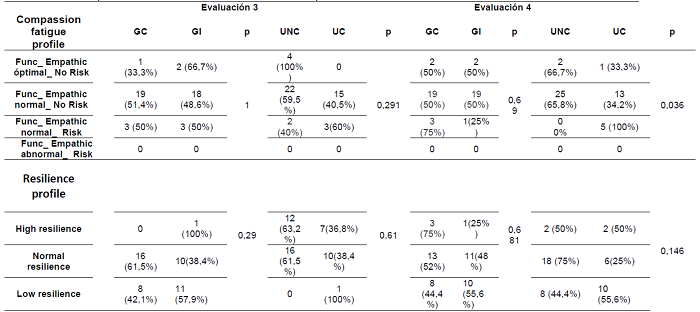
Empathy
To measure the variable exhaustion by empathy, the participants were classified into four profiles: optimal empathic functioning, normal empathic functioning, risky empathic functioning, and abnormal empathic functioning. The predominant empathic profile in the control and intervention group was normal without risk. No effect was found because of the intervention, nor of any other variable on the empathy exhaustion of the participants (Table 2), except that related to the which the participants worked at (Covid or non-Covid). The normal empathic profile without risk was significantly higher in non-covid units/wards compared to covid units/wards in the first evaluation (70% vs 30%, p=0.002) and in the fourth evaluation (65.8% vs 34.2% p= 0.036), (Table 2) (Table 3).
Table 2: Empathic and resilience profile by evaluation moment, group and work unit/ward (Evaluation 1, Evaluation 2).

*Note:CG: Control group, IG: Intervention group, NCU/W: Non-covid unit/ward, CU/W: Covid unit/ward, p: p value.
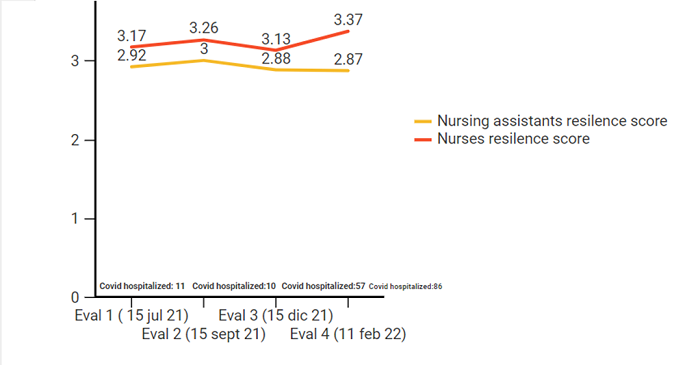
Resilience
Participants were classified into three profiles based on resilience (high, normal, and low). A normal resilience profile was identified in most of the professionals. No effect of the intervention was found in the evaluation of resilience, this was only related to the professional category. Auxiliary nurses, compared to Nursing professionals, obtained a low resilience profile in a higher percentage during the last evaluation (72.2% vs 27.8%, p=0.003), at moment that coincided with a greater number of patients hospitalized for covid (Figure 2).
DISCUSSION
The design of the evaluated activity took into account the available evidence and the methodology to be used. The content was based on a combination of different theoretical bases, since date provided from a review on the subject literature suggest better results then a single based intervention. A face-to-face approach, presented in groups, were also two characteristics of the intervention that, according to the latest available evidence, implied an advantage (5).
Regarding the duration of the intervention, different trials have shown efficacy in short or low-intensity interventions. Sood et al in 2011, using two 90-minute sessions, followed by another 30-60-minute session (which was optional), based on the SMART Stress Management and Resiliency Training (SMART) program, obtained significant results for the intervention group in resilience MD=-1.04, 95% CI=-0.28 -1.815, (5,11). Varker et al, in 2012, after carrying out a 4-hour activity, which included combined resilience training, estimated an improvement in some symptoms associated with depression and anxiety (F(3, 75) = 2.89, p < .05) (12).
Chesak et al, in 2015, after two sessions of 90 and 60 minutes that included content related to stress, calculated significant results for the resilience intervention group MD = 0.68, 95% CI= 0.04 , 1.32 5, (5,13).However, in synthesis studies, the efficacy of short-term interventions was lower when compared to long-term ones.
In the review by Kunzler et al, only high-intensity interventions, > 12 hours or > 12 sessions, demonstrated improvements in the resilience of healthcare professionals. Subgroup analysis of 11 studies showed that resilience increased significantly in high-intensity activities (MD=-0.46, 95% CI=-0.26 -0.67), compared to moderate-intensity activities (MD= -0.05, 95% CI=-0.02, 0.09), and with those of low intensity (MD=-0.53, 95% CI=-0.14, 1.2).
Despite the available evidence, long-term activities are difficult to include in the training programs in health centers and can lead to rejection and abandonment by professionals. This reason and the existence of trials that show an effect in favor of low intensity interventions (≤ five hours or ≤ three sessions) (11, 12 and 13), encouraged us to test a low intensity format.
The limitations of the study, non-randomized design, small sample size, and use of a low-moderate intensity intervention may have been some of the reasons for the ineffectiveness of the activity analyzed.
The results show us that shaping “ways of thinking”, attitudes and behavior requires continuity. Combined interventions, delivered in small groups, directly in the work place and fragmented (more than 12 sessions, but brief) could be adapted to the needs of the organization, so evaluating their effectiveness may be a hypothesis to be tested in another study.
REFERENCIAS
1. Santabárbara J, Bueno-Notivol J, Lipnicki DM, Olaya B, Pérez-Moreno M, Gracia-García P, et al. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: A rapid systematic review (on published articles in Medline) with meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 20 de abril de 2021;107:110244. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9188432/pdf/main.pdf [ Links ]
2. Sousa GM de, Tavares VD de O, de Meiroz Grilo MLP, Coelho MLG, Lima-Araújo GL de, Schuch FB, et al. Mental Health in COVID-19 Pandemic: A Meta-Review of Prevalence Meta-Analyses. Frontiers in Psychology [Internet]. 2021 [citado 14 de agosto de 2022];12. Disponible en: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.703838 [ Links ]
3. Al Maqbali M, Al Sinani M, Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. J Psychosom Res. febrero de 2021;141:110343. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7831768/pdf/main.pdf [ Links ]
4. Pollock A, Campbell P, Cheyne J, Cowie J, Davis B, McCallum J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. 5 de noviembre de 2020;11:CD013779. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7831768/pdf/main.pdf [ Links ]
5. Kunzler AM, Helmreich I, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst Rev. 5 de julio de 2020;7:CD012527. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8121081/pdf/CD012527.pdf [ Links ]
6. Blanco-Daza M, de la Vieja-Soriano M, Macip-Belmonte S, Tercero-Cano M del C. Trastorno de estrés postraumático en enfermeras durante la pandemia de COVID-19. Enferm Clin. 2022;32(2):92-102. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8677464/pdf/main.pdf [ Links ]
7. Aranda Auserón G, Elcuaz Viscarret MR, Fuertes Goñi C, Güeto Rubio V, Pascual Pascual P, Sainz de Murieta García de Galdeano E. Evaluación de la efectividad de un programa de mindfulness y autocompasión para reducir el estrés y prevenir el burnout en profesionales sanitarios de atención primaria. Atención Primaria. 2018;50(3):141-50. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6836985/pdf/main.pdf [ Links ]
8. Rodríguez-Rey R, Alonso-Tapia J, Hernansaiz-Garrido H. Reliability and validity of the Brief Resilience Scale (BRS) Spanish Version. Psychol Assess. mayo de 2016;28(5):e101-10. Disponible en: https://psycnet.apa.org/record/2015-48451-001 [ Links ]
9. Ruiz-Ruano-García AM, Sáez-García M, Moya-Faz FJ, López-Puga J, Ruiz-Ruano-García AM, Sáez-García M, et al. Propiedades psicométricas de la versión corta del Inventario Friburgo de Mindfulness. Terapia psicológica. abril de 2022;40(1):71-92. Disponible en: https://www.scielo.cl/scielo.php?pid=S0718-48082022000100071&script=sci_arttext&tlng=es [ Links ]
10. Maín, V., Rondón, J., Tauber, L., Viñuela, M., y Zamponi, J. (2009). ESAPE: escala para evaluar el Sindrome de Desgaste por Empatía. Argentina: Universidad Católica de Santa Fe. Disponible en: http://desgastexempatia.blogspot.com [ Links ]
11. Chesak SS, Bhagra A, Schroeder DR, Foy DA, Cutshall SM, Sood A. Enhancing resilience among new nurses: feasibility and eIicacy of a pilot intervention. Ochsner Journal 2015;15(1):38-44. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4365845/pdf/i1524-5012-15-1-38.pdf [ Links ]
12. Varker T, Devilly GJ. An analogue trial of inoculation/resiliencetraining for emergency services personnel: proof of concept.Journal of Anxiety Disorders 2012;26(6):696-701. Disponible en: https://pubmed.ncbi.nlm.nih.gov/22464031/ [ Links ]
13. Sood A, Prasad K, Schroeder D, Varkey P. Stress managementand resilience training among Department of Medicine faculty:a pilot randomized clinical trial. Journal of General InternalMedicine 2011;26(8):858-61. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3138987/ [ Links ]
Received: October 31, 2022; Accepted: January 19, 2023











 texto em
texto em