Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.22 no.72 Murcia Out. 2023 Epub 04-Dez-2023
https://dx.doi.org/10.6018/eglobal.561651
Originals
Case management: cost-effectiveness analysis in continuity of patient care of the Complex Chronic Patients Unit
1Hospital Clínico Universitario Virgen de la Arrixaca. Murcia. España
Objective:
Evaluate the relationship between the costs associated with the number and days of admission before and after inclusion in the Complex Chronic Patients Unit (CCP).
Methods:
A descriptive cost-effectiveness analysis was performed, with calculation of arithmetic averages and standard deviations; in addition to using the t-Student for paired samples, with the SPSS v20.0 software, for a significance level alpha <0.05. The results of the computation were obtained from the Coding Unit of the patients recruited by the case manager nurse, who survived one year of follow-up by the CCP Unit.
Results:
A total of 132 CCP were recruited, with a total of 563 previous admissions, which were reduced to 204 post inclusion. The average number of admissions of the previous year was 4.27 (SD: 3.35), and it was reduced to 1.55 (SD: 1.74). On the other hand, the number of days of total hospital stay was reduced from 3,835 to 1,897 days, which is equivalent to a difference in estimated cost of 11,165,164.36 euros. The average number of days of admission before was 29.05, and it was reduced to 14.37 days, finding a statistical significance (p< 0.001) between days of admission before and after.
Conclusions:
Inclusion in the CCP Unit guarantees, through the leadership of the case manager nurse, a cost-effective improvement without added expenses, by optimizing already existing interlevel care resources, through the identification of CCP and their priority needs, discharge planning with reports individualized and guaranteeing contact.
Key words: Case management; Cost efficiency analysis; Holistic nursing; Continuity of patient care; Chronic disease
INTRODUCTION
Chronic diseases are a real problem in Spain, where 49.3% of men and 59.1% of women aged 15 and over say they have some perceived chronic disease or health problem, percentages that are increasing as the age of the respondents increases, according to the National Health Survey in Spain 2020 (1). This, together with a life expectancy at birth in Spain, which in 2020 was estimated at 82.3 years, 80 years for men and 85 years for women, make chronicity still today a great challenge for our health system (2).
Undoubtedly, the change in our demographic pattern is undeniable, as well as in the epidemiological profile of the diseases of our population, where it is in the internal medicine service, since it mainly cares for hospitalized elderly people, where more emphasis should be placed on the need of a comprehensive, multidimensional evaluation and also contemplating the need for multidisciplinary development when carrying out care plans during hospitalization, due to the impact they can have on the prevention of mortality, disability, and institutionalization at discharge (3 ). Highlighting at this point, the role of the nurse with training interventions for CCP during hospitalizations in internal medicine has also been evidenced, which has managed to date its efficiency in reducing even short-term readmissions (4). Or reduction, even mortality, in post-discharge interventions in patients with heart failure or COPD (5) where in all of them, care continuity interventions are the key when it comes to preventing short-term hospital readmission in CCP (6).
Faced with these common challenges, different proposals have emerged in recent years, from the Chronicity Strategy presented by the Ministry of Health itself (7), where some autonomous communities have been adding alternative approaches to comprehensive care focused, not so much on the diseases, but in people. A clear example of them can be seen in a recent systematic review that includes several studies where tele-nursing is evidenced as an alternative for follow-up with two-way continuity plans to promote the nurse-patient relationship with the aim of teaching the management of their illnesses, with the patient as the true protagonist of the action (8). And it is that, if the pandemic has been of any use, it is to reconsider certain healthcare aspects of interesting reflection since non-face care has allowed monitoring of patients with chronic processes with great guarantee, but we must not forget the essentials of face-to-face care, as well as the need for organizational changes in favor of an integrated health organization, highlighting the need for adequate socio-health and community coordination (9).
This problem is also perceived by the users of the health system, who when asked about it, do not reach even half of the population to think that the coordination between the different levels of care is good, and although the overall assessment of primary care is estimated at 7.3 out of 10, in hospitals they receive an assessment of less than 7.1 points, an overall assessment of the public health system in Spain is about 6.7 points (1).
It is in this line of work, where in an internal medicine service of a tertiary hospital and of regional reference, the creation of a CCP Unit was therefore considered opportune. With a hospital case management model known as "extramural" (10) and with the incorporation of a CCP case management nurse (CMN), whose leadership model would be the transformational one to empower and motivate the professionals involved in each management of cases (11). After recruiting patients who meet the criteria, the CMN performs an assessment through a motivational interview, prepares an individualized care continuity plan, focused on multidisciplinary care, and where it will have to coordinate the care of a limited group of high-risk patients of readmission, and consequently are the ones with the highest consumption of hospital expenditure.
As previously mentioned, the extramural management model chosen extends care across a continuum of settings and time, independent of the patient's location. In this intervention, each and every one of the different professionals necessary in the care of the specific case is involve, in a complex and shared care, which promote responses proportional to the real needs, at all times, to the patients and their families/carers. In this way it is possible to avoid unnecessary transfers in patients that we consider to be complex due to their pathologies, bedridden or frail; bringing hospital resources closer to home, when necessary. For this reason, this population is also considered more vulnerable, since its numerous transitions between care levels is related to a greater risk of suffering adverse effects and errors (12), due to the change of health personnel and the complexity of their approach, deficit in updated and complete clinical reports, lack of therapeutic reconciliation or lack of establishing clear continuity of care plans for all professionals who have to approach the patient, among other reasons that could cause avoidable income.
OBJECTIVE
Evaluate the relationship between the costs associated with the number and days of admission before and after inclusion in the CCP Unit.
METHODS
Study design
This is a descriptive, before-after study, with calculation of averages and standard deviations (SD). In this study, a cost-effectiveness analysis of the patients identified and recruited throughout the year 2020 was carried out, and who survived for one year under follow-up by the unit, throughout 2021 (from January to December). The admission data for the previous year to the inclusion date were collected from the hospital Coding Unit, to meet the inclusion criteria of 3 admissions in the last year, at least one in charge of internal medicine, and thus compare with the data After one year of follow-up by the CCP Unit, patients surviving one year after hospital discharge.
The CCP Unit is included within the Internal Medicine Service with an internist and a reference case management nurse. This service has three medical hospitalization units, in addition to internal coordination with the home hospitalization units, the short-stay unit, and the palliative support unit. But the needs of the CCP require, in addition to the interventions of multiple other specialists and professionals located in the hospital, cooperation with the reference primary care team in the health area. That is, the different levels of care, through which CCP may need to be attended according to their needs, at all times.
Population, sample and sampling
The target population was all the patients who met the identification criteria in the electronic medical record of hospitalization, SELENE program as CCP, whose criteria are these 6 exposed below:
Patients residing in the area where the procedure was implemented.
Over 18 years of age.
Patients who are not reported in SELENE as deceased.
That they do not have the CCP alert.
That they have presented two or more hospital admissions during the last year, being at least one in Internal Medicine (including Infectious Diseases Unit and Short Stay Unit) and the other also in Internal Medicine (with its sections included) or in certain medical specialties.
That they have presented two or more pathologies defined by the Charlson Index(13), as main or secondary diagnosis in a specific group of diagnoses.
After this pre-selection, from which a list of patients identified with the CCP label of those admitted throughout the hospital was drawn up on a daily basis, a subsequent selection was made to capture the CCP admitted exclusively to the Internal Medicine Service.
For this study, the patients on the list were also given the following criteria, before being definitively included: they meet at least 2 criteria for polypathology according to Ollero (14), a Profund index between 7-10 points (15) (a score that entails an intermediate-high risk of probability of dying 12 months after hospital discharge), not being actively monitored by other units or institutionalized, and giving verbal consent to want to participate in the monitoring of the CCP Unit. On the contrary, the reasons for exclusion were that during the time of the study the CCP died, left the health area, the CCP wanted to leave the program or required referral to another unit for further follow-up.
So, throughout the year 2020, the case manager nurse selected patients for inclusion, prior to their verbal consent to be part of the follow-up by the CCP Unit, the recruitment was carried out through nursing assessment by functional health patterns of Marjory Gordon (16) with a motivational interview (17). An individualized continuity of care plan was prepared for each case included at discharge, with structured telephone follow-up in coordination with their reference primary care teams.
Procedure
The objective of the CCP Unit is to guarantee the continuity of care in patients with a high level of interlevel transitions through the Figure of the CMN. Said nurse with advanced skills in the management of CCP allows self-care needs to be detected on admission related to the nursing diagnosis called (00078) Ineffective health management. An individualized care plan that allows work on hospital discharge planning, optimizing resources, involving both professionals and users, in decision-making with a view to subsequent telephone follow-up. In the work of transitions, it is essential to have a joint approach with your reference team in primary care, to work in a shared care of interlevel assistance in a patient of complexity and high risk of readmission, where the proactive monitoring of the CMN of CCP It is essential to detect possible doubts or the beginning of decompensation after hospital discharge, and serve as support to their reference professionals through a structured call format, with a data collection form, from vital signs, such as signs and symptoms in relation to their chronic pathologies, which allow a recorded follow-up of their evolution at home, and very helpful in decision making.
Visits to face-to-face consultations are only made when necessary, such as at the beginning of acute decompensation, or referrals to the hospital if readmission is required. In all cases, the reference person is always the CMN of CCP to guarantee continuity of care in all processes for which both patients, family members and/or caregivers, as well as their reference professionals have their contact telephone number at Monday to Friday, from 8:00 a.m. to 3:00 p.m.
In this line, an efficient response in real time to the CCP is essential in passive care, where two decompensation circuits are established: minor, which can be resolved by telephone with doubts in treatments and indications related to the hospital discharge process or involvement of their multiple pathologies or polypharmacy, and that must be resolved with specialists located in the hospital or specialty center. These situations may lead to rescheduling appointments and/or pending tests or generating new ones due to the current need of the CCP. It is important, at this point, to highlight the frequent needs for resources and necessary involvement on the part of many other professionals, and from whom we need responses with a certain amount of time for timely decision-making, which does not pose a risk to the CCP, without being a dilated response in the usual times for patients who are not considered complex. And the other circuit, related to moderate-severe decompensation, which involves the referral of the patient back to the hospital, which can be assessed either in a face-to-face in the CCP consultation, or directly in Emergency, where admission will be expedited from the Admission Desk for continuous follow-up by their reference professionals, always coordinated by the CMN of CCP, as reference personnel and guarantee of continuity of care.
Patients who suffer decompensation outside of the timeTable of the CMN of CCP are referred to the Emergency, which will later be recaptured through the list of CCP admitted to the hospital, to continue and always guarantee interlevel care monitoring, regardless of the process or reason for exacerbation that happened to the CCP. During their stay in the hospital again, the CMN of CCP will get in touch with the patient, family members and/or caregivers, as well as with their reference professionals in primary care, whose feedback allows for improved coordination and contribution in decision-making in CCP and when rethinking the continuity of care plan again.
Analysis of data
In this study, the cost-effectiveness between the difference in costs and the difference in income was calculated before and after the inclusion of the CCP in the follow-up by the Unit. For this, the difference in the number of admissions and number of days of admission for CCP included, before and after inclusion in the follow-up, was considered. For the cost calculation, it was considered that one day of stay in a medical hospitalization unit (non-surgical) supposes a cost of 601.22 Euros/day, according to the data provided by BORM (18).
In addition, in the study of the data, the t-Student test was used for paired samples, with the SPSS Software v.20.0, for a significance level alpha < 0.05, calculating differences related to a 95% confidence interval (CI).
RESULTS
In total, 132 PCC were counted, who met the criteria determined for this study, after inclusion and follow-up by the CCP Unit, and who survived one year after the moment of hospital discharge to inclusion. The average age of the sample was 81.9 years (minimum age 61 years and maximum 96 years). In relation to the sex of the sample, the cases of women showed a slight increase, with a total of 76 women (57.6%), compared to a total of 56 men (42.4%).
Of the 132 CCP, it must be added that the reasons for readmission, at the time the patients were recruited by the CCP Unit, were mostly due to heart failure, 57 cases (43.18%), where 46.55% of the The sample had previously been admitted for heart failure, corresponding to Ollero's Category A (14). These data were added to those of respiratory infections, some 17 cases (12.87%) and very closely urinary tract infections in 16 of the cases (12.12%), among the most frequent.
In relation to the assessment of the CMN of CCP, it stood out that 40.15% of the sample did not meet the adherence criteria with the indicated treatment and, in addition, 59.84% presented a NYHA greater than III. It should be added that 100% of the sample presented the NANDA Nursing Diagnosis (00078) Ineffective health management as the main one, and mostly related to the complexity of the health system and excessive demands.
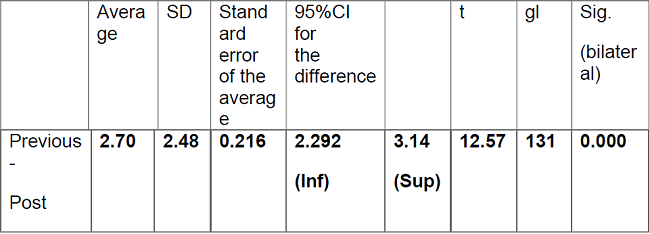
And lastly, with respect to the analysis of the data recorded in coding on the number of previous admissions of the patients included in the follow-up, it can be seen that they add up to a total of 563 admissions, compared to a reduction per year of 204 total admissions. In the following Table 1 we see the total average data between the number of admissions the year prior to inclusion, and the admissions after inclusion and follow-up by the CCP Unit.
As noteworthy data from the analysis, an average of admissions was obtained before 4.27 (SD: 2.35) admissions/year to an average reduction of 1.55 (SD: 1.74) admissions/year. Regarding the related differences in the number of admissions, there is a 95% CI reduction: 2.29-3.17 number of admissions/year, with a statistically significant reduction with p< 0.000.
In the analysis of data provided by the Coding Unit, it is verified that in 48 of the cases (36.36%) they did not present any readmission in the year of follow-up by the Unit, while in 12 of the cases (9.09%) presented a higher number of admissions than in the previous year to their recruitment by the CCP Unit.
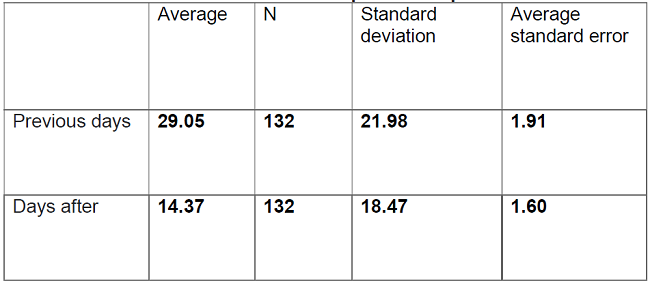
On the other hand, the number of days of total hospital stay of the sample was dated prior to inclusion at 3,835 days in a year, and after inclusion it was reduced to 1,897 days/year. Remaining in Table 2 reflected the reduction of average days compared to the previous year of being captured and followed by the CCP Unit.
From the management point of view, when dealing with the main objective proposed in said study to evaluate the cost-effectiveness of the unit's performance, it is important to emphasize that, considering that 1 day of stay in a medical (non-surgical) hospitalization unit supposes a cost of 601.22 Euros/day (18), the cost difference would average an estimated saving of 1,165,164.36 Euros/year.
Finally, a statistical significance (p< 0.001) was found between the days of admission before and after, after being included in the CCP Unit. Likewise, in terms of the differences related to the days of admission after less before, it presents a 95% CI reduction: 10.02-19.33 days.
DISCUSSION
In this study, a total of 132 PCCs were identified during one year. Said sample is slightly lower in a similar study of recruitment of primary care patients that achieved the follow-up of 149 patients (19). In addition, lower recruitment is reflected with respect to the recruitment by the unit itself a previous year, which was 207 CCP (20), since the unit must continue assuming the CCP captured until their referral, exit from the program or death, being the quota of patients limited to the load of the unit to assume follow-ups.
Concerning the characteristics of the sample, due to the age of the CCP, the average of the sample was 81.9 years (minimum age 61 years and maximum 96 years), higher than a similar study in which the average of the studied sample was from being 73.2 years old (21) and in another 75.4 years old (22), in all of them with lower ages or where the sex of the sample also presents very similar numbers of women (21,23). Regarding the characteristics of the CCP profile, we consider the change to an increasingly older population to be remarkable and undeniable, reflected in the average age of CCP captured in this second study compared to another analysis the previous year (20), possibly associated with being the population considered most frail (1, 2).
Regarding the results for the reason for readmission, 57 cases (43.18%) resulted in a higher frequency for heart failure and 46.55% of the sample had previously presented admission for heart failure. Percentages higher than those found in a similar study in chronic patients where the sample with heart failure was 27.8% (22), or compared to studies where planning the discharge of patients with a cardiology diagnosis was also the most frequent reason for admission (twenty-one). From the perspective of the CCP Unit, we point out heart failure as a frequent pathology in the internal medicine service, where the multidisciplinary approach, the involvement of the CCP and their caregivers, as well as guaranteeing continuity in follow-ups, we know have a direct influence on avoid relapses and avoidable admissions. On this subject, we see in Michalsen's study the need to delve into the causal factors that are prevenTable, specifically in readmissions due to decompensation in heart failure, more than half of which are considered prevenTable (19).
Regarding the assessment of the CMN of CCP, it was highlighted that 40.15% of the sample did not meet the adherence criteria with the indicated treatment, Figures that coincide with a study with similar characteristics, which reflect that 41.9 % of cases also presented lack of adherence to the medical regimen. In this study, it was associated as a causal factor for decompensation in heart failure, dating non-compliance with medications in 23.5% of patients. And, it is that same study, where the presence of dyspnea is highlighted, with levels higher than NYHA III in a high percentage of the sample, 88.1% (19), although in our study it was 59.84%, possibly due to heart failure was not exclusively the reason for CCP captured in our study.
In this study, the key is the assessment and planning of continuity of care at nursing discharge, since during the care the nurse is considered as the key Figure in the intervention during transitions. It is precisely this vision that is reflected in a similar way in another study, where the nurse is highlighted as the professional focused on promoting self-care, and the person responsible for guaranteeing the continuity of out-of-hospital care, and through health education during the stay on the ward (23). It is, therefore, this nursing intervention of identification and follow-up, the change to the usual way of acting, which makes it possible to avoid readmissions that may be avoidable in complex chronic patients from hospitalization.
It stands out among our results that 100% of the sample presented the Nursing Diagnosis (00078) Ineffective health management, and that it also perfectly contemplates all the work that addresses the CMN of CCP in transitions and specific follow-ups that are needed in case management of said CCP.
Regarding the results, after the analysis of the data registered in coding, on the number of previous admissions of the patients included in the follow-up, a total of 563 admissions were obtained. These results are higher compared to a reduction per year to 204 total admissions (therefore, 359 admissions were avoided). These are very high data compared to those reduced in a similar study (24) where it was reduced from 212 to 145 (67 admissions were avoided). This represents a reduction of 63.76% in our study, compared to a reduction of 31.60% in said reference study. In said study, the saving costs are calculated based on the number of days of admission, with a total saving between 70,847.3 Euros and 121,882.5 Euros, being in our study the total calculated based on the saving of days it represents a cost of one day of admission to the hospitalization unit estimated at 601.22 Euros/day as established in the BORM list(18). The results of our study estimate the difference in cost saved at approximately 1,165,164.36 euros in one year of follow-up by the case manager nurse, as the result of 1,938 days of stay avoided, due to the money involved each day of admission to the internal medicine department of the hospital.
Although there are few similar studies because they do not use the same methodology, these Figures can be verified with respect to another study of complex and advanced chronic patients, where avoided admissions were also calculated as a cost-effective measure (22). In this study, on the other hand, with regard to the reduction of days, it cannot be made comparable to our study, since it considers the expense by admission, and not by days of stay. However, it does help us to establish the need to implement a specific program as a way to manage the approach efficiently and safely, as well as the need to use the same identification tools, monitoring and measurement methodologies to be able to establish future relationships of the results.
The data shown in Table 1 shows the reduction in average income, which when compared with those produced by the same unit the previous year (20), we see less reduced number, since a year before a reduction of 3 was achieved, 44 to 0.57 after inclusion, and coinciding in the statistical significance of p< 0.000 between the days of admission before and after. On the other hand, it should also be noted regarding the comparison of both studies, where the differences related to days of admission after less before presented a 95% CI: 24.37 - 32.83 days with a p< 0.000 (20).
Despite reduction data, in number of admissions and days of general stays, it is highlighted in the results in some patients in whom it could not be reduced, but even saw increased expenses, in 9.09% of cases. This is due to the fact that we consider them to be ineviTable in CCP, and that it is also noTable in studies of the same study population (24). We must emphasize that the objective in monitoring a CCP Unit is to avoid the avoidable, and to support and attend to the ineviTable. That is why, in 48 of the cases (36.36%), they did not present any readmission in the year of follow-up by the Unit, but instead in the rest the readmissions were not avoidable, and even in 12 of the cases (9.09%) came to present a greater number of admissions than in the previous year to their recruitment by the CCP Unit. At this point we must keep in mind the complexity of CCP, since sometimes they are in the advanced phase of their pathologies, where the next referral to the palliative care unit should even be considered.
It is therefore considered important to highlight the efficiency of non-contact follow-ups, as well as follow-ups by nursing professionals as a reference in chronic patients and their caregivers, as highlighted in the Chronicity Approach Strategy (CAS) emphasizes in that it is the nurse, due to her clinical educational profile, who must play the role of coordinator in decision-making in continuity of care (7). And, without the slightest doubt, if chronicity is to be dealt with efficiently, it is necessary to consider improving coordination between care levels, with the incorporation of case management nurses which allows the hospital to give proportional responses to complex situations, and also save money for the healthcare system (7). We must also say that this study did not take into account the satisfaction and perceived quality of CCP and their caregivers, something that we consider to be the most noteworthy in case management and that should be considered in future lines of research within the CCP Unit, as well as well as the professionals involved in said procedures.
It should be noted that this study did not measure the number of interventions and visits in primary care either. Likewise, it has not been taken into account whether after the telephone management, performed from the hospital, has meant a significant increase in care for said primary care teams, as occurred in another study of integrated care for complex chronic patients (21). As well as we must consider that the CCP Unit seeks in its proactive follow-up, and also on demand, as far as possible the avoidance of unnecessary transfers to the hospital, and as far as possible the care of the patient at home in a manner proportional to the situation punctual CCP, which sometimes entails the involvement and referral of the case management to their reference team in primary care or home hospitalization units.
Finally, we must add as one of the main limitations of this study that it has been precisely the difficulty of the care and approach to the complexity of the patients that has been a real work challenge when evaluating the effectiveness of the program. This limitation is also mentioned in another study that emphasizes the importance of taking into account social factors or measures of personal autonomy as limitations in the study (21).
CONCLUSIONS
The guarantee of continuity of care at discharge, through case management, led by a nurse with advanced skills in complex chronic patients, represents a cost-effective improvement without added expenses, improving decision-making circuits, optimizing existing resources care interlevels, which by identifying CCP and their priority needs provides responses in proportion, as well as motivating and involving all the reference professionals, when their intervention is required.
Acknowledgment
We thank each and every one of the professionals of Health Area I of the Region of Murcia for their collaboration, involvement and work in coordinating the CCP, without whom this work would be impossible.
REFERENCES
1. Ministerio de Sanidad. Gobierno de España. Informe anual del sistema nacional de salud 2020-2021. (citado el 29 nov 2022) 2022. Disponible em: https://www.sanidad.gob.es/estadEstudios/estadisticas/sisInfSanSNS/TablasEstadisticas/InfAnualSNS2020_21/INFORME_ANUAL_2020_21.pdf. [ Links ]
2. Instituto Nacional de Estadística (INE). Encuesta Europea de Salud en España (EESE) 2020. (citada 29 nov 2022) Disponible en: https://www.sanidad.gob.es/estadEstudios/estadisticas/EncuestaEuropea/EncuestaEuropea2020/EESE2020_inf_evol_princip_result.pdf [ Links ]
3. Vallejo Maroto I, Cubo Romano P, Mafé Nogueroles M.C., Matesanz-Fernández M, Pérez-Belmonte L.M, Said Criado I, Gómez-Huelgas R, Díez Manglano J. Recomendaciones sobre la valoración integral y multidimensional del anciano hospitalizado. Posicionamiento de la Sociedad Española de Medicina Interna. Revista Clínica Española. Vol. 221. 2021 Jun-Julio; 6: 347-358. doi: 10.1016/j.rce.2020.10.003. [ Links ]
4. Blanco-López RM, Fole-Santalla MD, Rio-Enríquez M, Quiroga-Mariño MJ, Barcón-Pajón M, Casariego-Vales E; en representación del Grupo de Estudio de Formación por Enfermería. Effectiveness of a nursing training intervention in complex chronic patients. Enferm Clin (Engl Ed). 2020 Sep-Oct;30(5):302-308. English, Spanish. doi: 10.1016/j.enfcli.2019.08.008. Epub 2019 Nov 6. PMID: 31706728. [ Links ]
5. Bamforth RJ, Chhibba R, Ferguson TW, Sabourin J, Pieroni D, Askin N, Tangri N, Komenda P, Rigatto C. Strategies to prevent hospital readmission and death in patients with chronic heart failure, chronic obstructive pulmonary disease, and chronic kidney disease: A systematic review and meta-analysis. PLoS One. 2021 Apr 22;16(4):e0249542. doi: 10.1371/journal.pone.0249542. PMID: 33886582; PMCID: PMC8062060. [ Links ]
6. Facchinetti G, D'Angelo D, Piredda M, Petitti T, Matarese M, Oliveti A, De Marinis MG. Continuity of care interventions for preventing hospital readmission of older people with chronic diseases: A meta-analysis. Int J Nurs Stud. 2020 Jan;101:103396. doi: 10.1016/j.ijnurstu.2019.103396. Epub 2019 Aug 15. PMID: 31698168. [ Links ]
7. Ministerio de Sanidad Servicios Sociales e Igualdad, Ministerio de Sanidad-Servicios Sociales e Igualdad. Estrategia para el abordaje de la cronicidad en el Sistema Nacional de Salud. 2012; 80. https://www.sanidad.gob.es/organizacion/sns/planCalidadSNS/pdf/ESTRATEGIA_ABORDAJE_CRONICIDAD.pdf [ Links ]
8. Alcazar B, Ambrosio L. Tele-enfermería en pacientes crónicos: revisión sistemática [Tele-nursing in patients with chronic illness: a systematic review]. An Sist Sanit Navar. 2019 Aug 23;42(2):187-197. Spanish. doi: 10.23938/ASSN.0645. PMID: 31270511. [ Links ]
9. Lesende IM. Lecciones aprendidas durante la pandemia COVID-19 sobre el seguimiento de pacientes crónicos [Lessons learned during the COVID-19 pandemic on the follow-up of chronically ill patients]. Aten Primaria. 2021 Oct;53(8):102180. Spanish. doi: 10.1016/j.aprim.2021.102180. PMID: 34593101; PMCID: PMC8482472. [ Links ]
10. Morales JM. Gestión de casos y cronicidad compleja: conceptos, modelos, evidencias e 65 incertidumbres. Enferm Clin. [Internet] 2014; 24(1):23-34. [citado 6 Nov 2022]. Disponible en: https://www.elsevier.es/esrevista-enfermeria-clinica-35-articulogestion-casos-cronicidad-complejaconceptos-S1130862113001563 [ Links ]
11. Collins E, Owen P, Digan J, Dunn F. Applying transformational leadership in nursing practice. Nurs Stand. 2020 Apr 29;35(5):59-66. doi: 10.7748/ns.2019.e11408. Epub 2019 Dec 16. PMID: 31840443. [ Links ]
12. Plan de Calidad para el Sistema Nacional de Salud. http://www.msssi.gob.es/ca/organizacion/sns/planCalidadSNS/). [ Links ]
13. Brusselaers N, Lagergren J. The Charlson Comorbidity Index in Registry-based Research. Methods Inf Med. 2017;56(5):401-406. doi: 10.3414/ME17-01-0051. Epub 2018 Jan 24. PMID: 29582935. [ Links ]
14. Barrio-Cortes J, Del Cura-González I, Martínez-Martín M, López-Rodríguez C, Jaime-Sisó MÁ, Suárez-Fernández C. Grupos de morbilidad ajustados: características y comorbilidades de los pacientes crónicos según nivel de riesgo en Atención Primaria [Adjusted morbidity groups: Characteristics and comorbidities in patients with chronic conditions according to their risk level in Primary Care]. Aten Primaria. 2020 Feb;52(2):86-95. Spanish. doi: 10.1016/j.aprim.2018.12.007. Epub 2019 May 29. PMID: 31153669; PMCID: PMC7025976. [ Links ]
15. Moretti D, Buncuga MG, Laudanno CD, Quiñones ND, Scolari Pasinato CM, Rossi FE. Índice PROFUND y mortalidad intrahospitalaria en pacientes pluripatológicos. Análisis post-hoc [PROFUND index and intrahospital mortality in plurypathological patients. A post-hoc analysis]. Medicina (B Aires). 2021;81(3):329-336. Spanish. PMID: 34137691. [ Links ]
16. Arroyo-Lucas S, Vásquez-Cruz R, Martínez-Becerril M, Nájera-Ortiz MP. Patrones funcionales: una experiencia en el camino de la construcción de conocimiento. Rev Mex Enf. 2018;6-97-102. [ Links ]
17. Moral RR, Torres LA, Ortega LP, Larumbe MC, Villalobos AR, García JA, Rejano JM; Collaborative Group ATEM-AP Study. Effectiveness of motivational interviewing to improve therapeutic adherence in patients over 65 years old with chronic diseases: A cluster randomized clinical trial in primary care. Patient Educ Couns. 2015 Aug;98(8):977-83. doi: 10.1016/j.pec.2015.03.008. Epub 2015 Mar 18. PMID: 25858633. [ Links ]
18. Orden de 29 de mayo de 2020 de la Consejería de Presidencia y Hacienda, por la que se publican las tarifas de las tasas y precios públicos aplicables en el año 2020. Boletín Oficial de la Región de Murcia, Número 133, (11 de Junio de 2020). [ Links ]
19. Coderch J, Pérez-Berruezo X, Sánchez-Pérez I, Sánchez E, Ibern P, Pérez M, Carreras M, Inoriza JM. Evaluación de la efectividad de un programa de atención integrada y proactiva a pacientes crónicos complejos [Assessment of the effectiveness of a proactive and integrated healthcare programme for chronic complex patients]. Gac Sanit. 2018 Jan-Feb;32(1):18-26. Spanish. doi: 10.1016/j.gaceta.2016.07.014. Epub 2016 Oct 24. PMID: 27789050. [ Links ]
20. Roldán-Valcárcel MD, Beteta Fernández D, Iniesta Alcázar J, Lucas Gómez JM, Navarro Egea AP, Pérez Luján R. Eficiencia de la Enfermera Gestora de casos liderando una Unidad de Pacientes Crónicos Complejos. 22cnh Congreso Nacional de Hospitales y Gestión Sanitaria, Málaga, 2021. https://www.google.com/search?q=libro+de+ponencias+22-congreso-nacional-de-hospitales-y-gestion-sanitaria/&rlz=1C5CHFA_enES930ES930&sxsrf=ALiCzsZuzf7STtJJ_eZJHXkvi-Tk2n6uqw:1669725598090&source=lnms&tbm=isch&sa=X&ved=2ahUKEwja15XJtNP7AhXBzqQKHZY7CQQ4ChD8BSgCegQIHhAE&biw=1401&bih=1226&dpr=1 [ Links ]
21. Barrio Cortes J, Suárez Fernández C, Bandeira de Oliveira M, Beca Martínez MT, Lozano Hernández C, Del Cura-González I. Utilización de los servicios de salud de Atención Primaria en los pacientes crónicos según nivel de riesgo [Health services utilization in Primary Care in patients with chronic conditions according to risk levels]. Rev Esp Salud Publica. 2019 Sep 6;93:e201909082. Spanish. PMID: 31488808. [ Links ]
22. Michalsen A, König G, Thimme W. PrevenTable causative factors leading to hospital admission with decompensated heart failure. Heart. 1998 Nov; 80(5): 437-41. doi: 10.1136/hrt.80.5.437. PMID: 9930040; PMCID: PMC1728853. [ Links ]
23. Cano Arana A, Martín Arribas MC, Martínez Piédrola M, García Tallés C, Hernández Pascual M, Roldán Fernández A; investigator team. Eficacia de la planificación del alta de enfermería para disminuir los reingresos en mayores de 65 años [Efficacy of nursing planning after hospital discharge of patients over 65 to reduce their readmission]. Aten Primaria. 2008 Jun;40(6):291-5. Spanish. doi: 10.1157/13123681. PMID: 18588800; PMCID: PMC7713473. [ Links ]
24. Allepuz Palau A, Piñeiro Méndez P, Molina Hinojosa JC, Jou Ferre V, Gabarró Julià L. Evaluación económica de un programa de coordinación entre niveles para el manejo de pacientes crónicos complejos [Economic evaluation of a program of coordination between levels for complex chronic patient' management]. Aten Primaria. 2015 Mar;47(3):134-40. Spanish. doi: 10.1016/j.aprim.2014.05.002. Epub 2014 Jun 19. PMID: 24953172; PMCID: PMC6983786. [ Links ]
Received: March 20, 2022; Accepted: May 16, 2023











 texto em
texto em