Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versão On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.3 Mai./Jun. 2006
Stafne bone cavity: a retrospective study of 11 cases
Cavidad de Stafne: Estudio retrospectivo de 11 casos
Carmen Quesada Gómez 1, Eduard Valmaseda Castellón 2,Leonardo Berini Aytés 3, Cosme Gay Escoda 4
(1) Odontóloga. Residente del Máster de Cirugía e
Implantología Bucal. Facultad de Odontología de la Universidad de Barcelona
(2) Doctor en Odontología. Profesor Asociado de Cirugía
Bucal. Profesor del Máster de Cirugía Bucal e Implantología Bucofacial.
Facultad
de Odontología de la Universidad de Barcelona
(3) Doctor en Medicina. Estomatólogo. Especialista en Cirugía
Maxilofacial. Profesor Titular de Patología Quirúrgica Bucal y Maxilofacial.
Profesor del Máster de Cirugía Bucal e Implantología Bucofacial. Facultad de
Odontología de la Universidad de Barcelona
(4) Doctor en Medicina. Estomatólogo. Especialista en Cirugía
Maxilofacial. Catedrático de Patología Quirúrgica Bucal y Maxilofacial.
Director
del Máster de Cirugía Bucal e Implantología Bucofacial. Facultad de Odontología
de la Universidad de Barcelona.
Servicio de Cirugía Bucal, Implantología
Bucofacial y Cirugía Maxilofacial del Centro Médico Teknon. Barcelona
ABSTRACT
Objective: to describe the clinical and radiological
characteristics of patients with Stafne bone cavity.
Study design:
a retrospective, observational study of 11
cases of Stafne bone cavity. After finding an imagine compatible with Stafne
bone cavity in the Orthopantomograph® of 11 patients, a sialography
of the mandibular gland was made in 3 cases, computerized tomography (CT) in 6
cases, and in 4 cases surgical intervention to confirm the diagnosis.
Results: the average age was 51.5 years, predominantly
males. The entity was diagnosed incidentally during a routine radiology in all
cases. The sialography revealed glandular tissue within the defect, and the CT
demonstrated the conservation of the lingual cortical and the peripheral origin
of the lesion. Glandular tissue was found within the lesions of two of the
patients who underwent surgery, and in the other two the cavity was empty. No
progressive changes were found in any of the 11 cases.
Conclusions: Stafne bone cavity was an incidental finding,
presenting no evolutionary changes, and as such conservatory therapy based on
periodic controls was indicated. Currently, complementary techniques such as CT
are sufficient to establish a certain diagnosis.
Key words: Stafne bone cavity, mandibular bone depression, lingual mandibular bone defect.
RESUMEN
Objetivo: Describir las características clínicas y
radiológicas de pacientes con cavidad de Stafne.
Diseño del estudio: Estudio retrospectivo observacional
de 11 casos de cavidad de Stafne. Tras hallar en la ortopantomografía de 11
pacientes una imagen compatible con cavidad de Stafne, se solicitaron
sialografía de la glándula submaxilar en 3 casos, tomografía computadorizada (TC)
en 6 pacientes y se realizó una intervención quirúrgica en 4 casos para obtener
un diagnóstico de certeza.
Resultados: La edad media fue de 51.5 años y el sexo
masculino fue predominante. Esta entidad fue diagnosticada siempre de forma
casual tras una exploración radiológica de rutina. Las sialografías permitieron
observar tejido glandular dentro del defecto y con la TC se visualizó la
conservación de la cortical lingual y el origen periférico de la lesión. Dos
pacientes intervenidos quirúrgicamente tenían tejido glandular en el interior de
la lesión y 2 tenían la cavidad vacía. No se observaron cambios evolutivos en
ninguno de los 11 casos.
Conclusiones: La cavidad de Stafne fue un hallazgo
radiológico casual que no presentó cambios evolutivos estando así indicada una
opción terapéutica conservadora basada en controles periódicos. Actualmente, las
pruebas complementarias como la TC son suficientes para establecer un
diagnóstico de certeza.
Palabras clave: Cavidad de Stafne, depresión ósea mandibular, defecto óseo mandibular lingual.
Introduction
In 1942, Stafne (1) described for the first time, 35 asymptomatic, radiolucent cavities, unilaterally located in the posterior region of the mandible, between the mandibular angle and the third molar, below the inferior dental canal and slightly above the basis mandibulae. Since then, and due to the multiple explanations offered as to its etiopathogenesis, this entity has been given numerous names, particularly, static bone cyst, lingual mandibular bone defect, Stafne bone cavity, idiopathic bone cavity and lingual mandibular bone depression. (2-7) Although 4 variants of this entity have been described, when the term Stafne bone cavity is found in the literature it usually refers to the posterior lingual variant. This is located between the mandibular angle and the first permanent molar, below the inferior dental canal. (2, 3, 5, 7) The anterior lingual variant, 7 times less frequent than the posterior, is usually located between the incisor and the premolar areas, above the insertion of the mylohyoid muscle. (3, 8-10) Variants with lingual or buccal location of the ascending ramus of the mandible are very infrequent findings. (3, 4, 11)
The posterior lingual variant has an incidence of between 0.10 and 0.48% when diagnosed radiologically, although in studies where mandibulars from cadavers are examined this value can reach 6.06%. (2, 3, 5, 7)
The age range is quite wide, although there is a clear predilection for males in the 5th or 6th decade. (3, 7, 12)
The objective of this study is to describe the clinical and radiological characteristics of cases of Stafne bone cavity.
Patients and methods
A retrospective study was made of 11 patients with Stafne bone cavity who attended the Vall d´Hebron General Hospital, Granollers General Hospital, Teknon Medical Center and the Master in Oral Surgery and Buccofacial Implantology of the University of Barcelona. In each case the orthopantomographic study (made for other reasons, or as part of the complementary studies of a first visit) revealed a rounded or ovoid radiolucent image, in the posterior area of the mandible, having no apparent relationship with the teeth, and either below or superimposed on the inferior dental canal. Once a provisional diagnosis of Stafne bone cavity had been established, complementary tests were requested in order to identify the lesion. A sialography of the submandibular gland was carried out on three patients, and in six cases a computerized tomography was performed, two of these with three-dimensional reconstruction. Four patients were surgically intervened, either fearing cancer or to verify diagnosis.
The following data were collected by the same professional: age, sex, reason for consultation, symptomatology, history of trauma, shape, size and radiological characteristics, variant, treatment and evolution.
The data was processed using the Statistical Package for Social Sciences version 9.0 (SPSS; Chicago, USA). The Kolmogorov-Smirnov test was used to determine the normal distribution for age.
Results
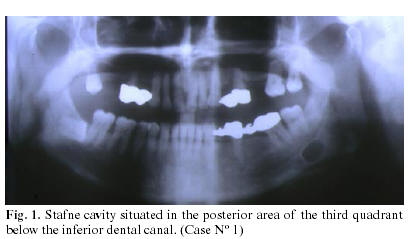
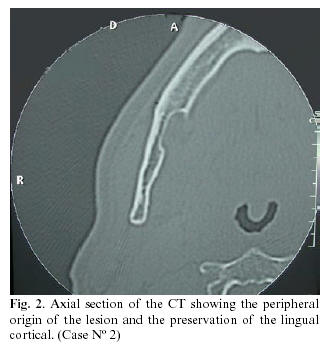
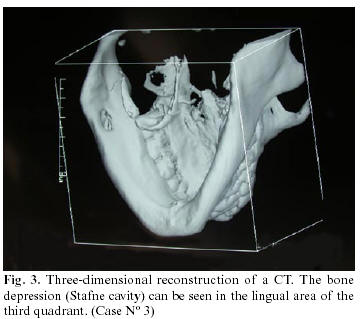
The average age of the patients was 51.5 years, range 29 to 74. There was a predominance of males (8:3), with no signs or symptoms in any of the cases, the entity being diagnosed incidentally by radiological examination in all cases. No history of trauma was established. The image obtained by Orthopantomograph® was round in 3 cases, and elliptical in eight. Regarding location, all cases were posterior lingual variants, 7 being located in the area of the mandibular ridge at the 2nd or 3rd molar level (figure 1), 2 situated in the mandibular angle and 2 in the mandibular ridge. The 3 sialographies of the submandibular gland revealed the presence of glandular tissue within the cavity. The CT demonstrated the conservation of the lingual cortical and the peripheral origin of the lesion (figure 2). The three-dimensional reconstruction produced for two patients clearly showed a cavity in the lingual cortical (figure 3). Treatment was conservative with periodic radiological control by orthopantomographic study in 7 cases, and surgical in 4 cases, glandular tissue being found within the cavity of two of these. No evolutionary changes were found in any of the subsequent radiographic controls of the 11 patients.
Discussion
The Stafne bone cavity is generally detected in patients in the 5th or 6th decade of life, although cases have been described in ages between 11 and 87 years. (3, 7, 12, 13) Our sample shows a predominance of patients diagnosed between 40 and 60 years of age. Another epidemiological aspect referred to by Philipsen et al. (3), is that this entity is much more frequent in males, with a male/female ratio of 6:1. In the present study, there was also a greater, but less evident, preference for males, (8:3).
Various theories exist which attempt to explain the etiopathology of the Stafne bone cavity. Currently the large majority of authors (2-7, 9), consider this entity to originate from the pressure exercised by glandular tissue on the lingual cortical of the mandible. The submandibular gland is directly related with the posterior variant, while the sublingual gland is related to the anterior variant, and the parotid gland with the two variants of the ascending ramus of the mandible. (3, 4).
Defenders of this etiology support their argument essentially on the results of sialographies and surgical findings. Our results appear to be in accordance with this theory, since glandular tissue was found within the defect of the 3 patients subjected to sialographies of the submandibular gland and in two of the patients intervened surgically. However, in two of the patients operated on the cavities were empty, which could be explained by the accidental displacement of tissue during surgical manipulation, or by the actual position of the patient during surgery. Other congenital or embryonal etiological factors have been described, especially deficient bone formation in the area previously occupied by Meckel cartilage. (1, 3, 6, 12) The facial artery could also be associated with these defects, given that an abnormal vascular pressure could originate necrosis and resorption of the adjacent bone. (1, 3, 6, 7, 12)
The diagnosis of this cavity is incidental, since patients do not usually present clinical symptoms. (2) In the Orthopantomograph®, the test which usually first identifies this entity, a radiolucent image with a well-defined sclerotic border is generally observed, situated at a posterior location of the mandible, below the inferior dental canal. (2, 12, 14, 15)
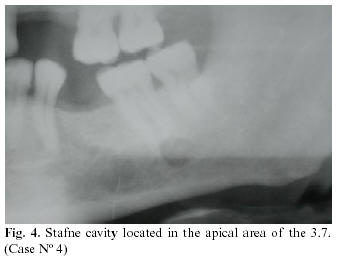
In such cases the diagnosis is easier. However, if the location of the cavity is atypical (figure 4), this complementary test does not provide a reliable diagnosis and other methods such as CT should be used. (2-7, 11 12, 14, 15) Likewise, although some authors (3, 5, 7, 14 15) do not view sialography as a very effective tool, other more classical studies (2, 4) consider it to be a useful method, since it can establish a relationship between the glandular tissue and the cavity. CT, currently considered as the complementary test of choice, has the great advantage of verifying the peripheral origin of the lesion and the conservation of the lingual cortical, which are essential characteristics for discounting other pathologies such as apical or residual cysts, fibrous dysplasia, traumatic osseous cyst, among others. (5-7, 12, 14, 16) Ariji et al. (6) add that CT permits, to a certain extent, the identification of the tissue found within the cavity. Magnetic resonance (MR), is a test also referred to in the literature (3, 7) being considered by Branstetter et al. (17) as essential. In our cases, both the 3 sialographies of the submandibular gland, in which glandular tissue was observed within the defect, and the CT, were sufficient to confirm the diagnosis. CT with three-dimensional reconstruction has, in recent years, been considered as a reasonably effective complementary test in this entity, as also shown in our series. (16)
The two main therapeutic options are based on either surgical intervention or a wait and see approach, the latter being preferred, always with periodic clinical and radiological controls. (2-7, 14) Currently, due to increased development in imaging techniques, and to the static and benign character of the entity, the use of periodic radiological controls is, without doubt, the most adequate. (2-7, 14) Likewise, various authors affirm that CT avoids unnecessary surgery. (3, 6) In our series, 4 patients were subjected to surgical examination, which can be explained by the fact that these patients were diagnosed before 1988, an age in which radiological tests were neither as accessible nor as effective. However, in atypical cases, or when doubts exist as to diagnosis, surgical intervention and a subsequent anatomopathological examination of the extirpated tissue may be indicated, since this is the only way in which to discount a neoplastic pathology with certainty. In fact, there is a case, published by Simpson (18), of a pleomorphic adenoma contained within a Stafne bone cavity.
![]() Correspondence:
Correspondence:
Dr. Cosme Gay Escoda
Centro Médico Teknon
C/ Vilana 12
08022 - Barcelona
E-mail: cgay@ub.edu
Received: 30-09-2004
Accepted: 25-03-2005
References
1. Stafne E. Bone cavities situated near the angle of the mandible. J Am Dent Assoc 1942;29:1969-72. [ Links ]
2. Grau J, Gay Escoda C, Hernández F. Cavidad de Stafne. Revisión a propósito de 6 casos. Av Odontoestomatol 1991;7:83-7. [ Links ]
3. Philipsen H, Takata T, Reichart P, Sato S, Suei Y. Lingual and buccal mandibular bone depressiones: A review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofac Radiol 2002;31:281-90. [ Links ]
4. Barker G. A radiolucency of the ascending ramus of the mandible associated with investid parotid salivary gland material and analogous with a Stafne bone cavity. Br J Oral Maxillofac Surg 1988;26:81-4. [ Links ]
5. Slasky B, Bar-Ziv J. Lingual mandibular bony defects: CT in the buccolingual plane. J Comput Assit Tomogr 1996;20:438-43. [ Links ]
6. Ariji E, Fujiwara N, Tabata O, Nakayama E, Kanda S, Shiratsuchi Y, et al. Stafnes bone cavity: Classification based on outline and content determined by computer tomography. Oral Surg Oral Med Oral Pathol 1993;76:375-80. [ Links ]
7. Grellner T, Frost D, Brannon R. Lingual mandibular bone defect: Report of three cases. J Oral Maxillofac Surg 1990;48:288-96. [ Links ]
8. Phillips A, Yates C. Case report: Anterior lingual mandibular cortical bone concavity. Dent Update 2004;31:175-6. [ Links ]
9. de Courten A, Kuffer R, Samson J, Lombardi T. Anterior lingual mandibular salivary gland defect (Stafne defect) presenting as a residual cyst. Oral Surg Oral Med oral Pathol Oral Radiol Endod 2002;94:460-4. [ Links ]
10. Katz J, Chaushu G, Rotstein I. Stafnes bone cavity in the anterior mandible: A posible diagnostic challenge. J Endod 2001;27:304-7. [ Links ]
11. Campos P, Panella J, Crusoé-Rebello I, Azevedo R, Pena N, Cunha T. Mandibular ramus-related Stafnes bone cavity. Dentomaxillofac Radiol 2004;33:63-6. [ Links ]
12. Barrer G. Xeroradiography in relation to a Stafne bone cavity. Br J Oral Maxillofac Surg 1988; 26:32-5. [ Links ]
13. Wolf J, Mattila K, Ankkuriniemi O. Development of a Stafne mandibular bone cavity. Report of a case. Oral Surg Oral Med Oral Pathol 1986;61:519-21. [ Links ]
14. Reuter I. An unusual case of Stafne bone cavity with extra-osseous course of the mandibular neurovascular bundle. Dentomaxillofac Radiol 1998;27:189-91. [ Links ]
15. Prapanpoch S, Langlais R. Lingual cortical defect of the mandible: An unusual presentation and tomographic diagnosis. Dentomaxillofac Radiol 1994; 23:234-7. [ Links ]
16. Lubieniecka E, Subirán B, Fernández L. Depresión ósea mandibular. Estudio realizado mediante tomografía computada con un software dental. Archivos de Odontoestomatolología 2003;19:616-22. [ Links ]
17. Branstetter B, Weissman J, Kaplan S. Imaging of a stafne bone cavity: What MR adds and why a new name is needed. AJNR Am J Neuroradiol 1999;20:587-9. [ Links ]
18. Simpson W. A Stafnes mandibular defect containing a pleomorphic adenoma. J Oral Surg 1965;23:553-6. [ Links ]











 texto em
texto em