Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.4 jul. 2006
Stafne bone cavity – Magnetic resonance imaging
Yoram Segev1, Max Puterman2, Lipa Bodner3
1Senior Staff, Department of Diagnostic Radiology
2Senior Lecturer , Department of Otolaryngology Head and Neack Surgery
3Associate Professor and Chairman, Department of Oral and Maxillofacial Surgery,
Soroka University Medical Center and Ben Gurion University of the Negev, Beer-Sheva , Israel
ABSTRACT
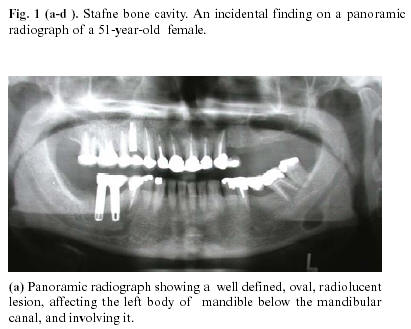
A case of Stafne bone cavity (SBC) affecting the body of the mandible of a 51-year-old female is reported. The imaging modalities included panoramic radiograph, computed tomography (CT) and magnetic resonance (MR) imaging.
Panoramic radiograph and CT were able to determine the outline of the cavity and its three dimentional shape, but failed to precisely diagnose the soft tissue content of the cavity. MR imaging demonstrated that the bony cavity is filled with soft tissue that is continuous and identical in signal with that of the submandibular salivary gland.
Based on the MR imaging a diagnosis of SBC was made and no further studies or surgical treatment were initated. MR imaging should be considered the diagnostic technique in cases where SBC is suspected. Recognition of the lesion should preclude any further treatment or surgical exploration.
Key words: Mandible, lingual bone cavity, Stafne bone cavity, CT, MR, imaging.
Introduction
Stafne bone cavity (SBC), also known as lingual mandibular bone defect , is a bony cavity of the mandible containing salivary gland. This cavity has a cystlike appearance on plain film radiographs. It was described for the first time by in 1942 by Stafne, who reported on 35 cases appearing as round or ovoid, well-defined, unilocular radiolucencies, located below the mandibular canal, between the first molar and the angle of the mandible. A SBC is usually an asymptomatic incidental radiologic findings, and mostly affect males in the their fifth to seventh decade of life. Surgical exploration has shown salivary gland tissue in the concavity , often in continuity with the submandibular gland (1,2). There has been some debate regarding the nature of the lesion,whether a congenital or a developmental in origin (3,4).
Although the radiologic features of SBC have been widely reported , these include mainly the plain film and CT appearance. The MR imaging has been reported only scarcely (5-7) . The purpose of the present report is to describe a case occuring in the body of mandible with focus on the role of MR imaging in establishment of the final diagnosis.
Report of Case
A 51-year-old female was referred by her dentist with an asymptomatic"lesion" in the mandible, discovered incidentally on a panoramic radiograph done for routine dental treatment. There was no previous trauma to the mandible or contributory medical history. Extraoral and intraoral examination revealed no remarkable findings.
There was no cervical lymphadenopathy and the laboratory data were unremarkable.
Panoramic radiograph revealed a unilocular, oval radiolucent lesion with well defined sclerotic borders, situated at the second and third molar region, below the mandibular canal. The cortical outline of the mandibular canal was clearly visible anterior and posterior to the lesion, with no sign of displacement. (Fig 1a). Axial CT scan of the mandible with bucco-lingual reconstruction program (DentaScan, General Electric, Milwaukee, USA), revealed discontinuity in the lingual cortex and some erosion in the buccal cortex (Fig 1b). The content of the lesion appeared to be a soft tissue mass.
MR imaging of the mandible disclosed that the bone cavity is filled with soft tissue that is continuous and identical in signal with that of the submandibular gland.This could be seen in all types of sequences and in various plains (Fig 1c, 1d). A diagnosis of SBC was made and no further investigations or therapy were initiated.
Discussion
The SBC was first discribed by Stafne in 1942. Since then numerous cases of the entitiy have been reported (1,2,5,8-12). The exact pathogenesis is still obscure. Stafne suggested that the cavity could result from a failure of normal bone deposition in the region formely occupied by cartilage (1,8). However, the most widely accepted view is that the cavities develop as a result of a localized pressure atrophy of the lingual surface of the mandible from the adjacent salivary gland (9).
This theory is supported by findings of radiolicencies in association with both submandibular and sublingual salivary glands (10). Surgical series, following exploration of the mandibular bony defect, have noted salivary tissue within the bony defect, however, non salivary tissue, such as lymphatic tissue, muscle and blood vessels have also been reported . The non salivary gland tissue findings in the surgical reports may be explained by intermitted gland herniation, regression of the herniated gland or surgical disruption of the cavity content (13).Most reports on SBC, are case reports and have discussed their findings on intraoral dental films, plain films of the mandible or pamoramic radiographs. Although these imaging techniques may be sufficient for diagnosis in some cases, they may not be enough for a definitive diagnosis in many other cases, especially, where the lesion is atypical, such as lobulated , incomplete sclerotic margins, multiple, or unusual location(6,13).
The differential diagnosis of SBC includes benign and malignant jaw lesions such as: odontogenic cystic lesion, nonossifying fibroma, fibrous displasia, vascular malformation, focal osteoporotic bone marrow defect, brown tumor of hyperparathyroidism, ameloblastoma, basal cell nevus syndrom, giant cell tumor or a metastasis from a primary malignant tumor . Therefore, in some cases more confirmatory diagnostic tools are mandatory. Sialography is able to depict salivary tissue in the bony cavity and has been used to confirm the diagnosis (14). However, there were case reports of surgically proved SBC with negative results in sialography (15).
Some CT evaluations of SBC were able to show salivary tissue within the bone defect (14,16, 17).
The fact that CT is more specific to bone lesions of the jaws and much less so to soft tissue have led some outhors to advocate MR imaging as the primary diagnostic technique (5-7). Some authors however, have advocated MR imaging only after they had exposed their patients to unnecessary surgical exploration (5,6). The main advantage of MR imaging is its superior soft tissue characterization and discrimination. The superior soft tissue contrast of MR imaging should be adequate to make the diagnosis of SBC, even without any intravenous contrast material. Its major disadvantage is the high cost and the distortion artifacts produced by dental material. Branstetter et al (7) were the first to establish a diagnosis of SBC merely on MR imaging with no further treatment. Our case is apparantly the second one. In the present case MR imaging was performed only after panoramic radiograph and Dental CT scan were unable to establish a precise diagnosis, regarding the content of the bony cavity. MR imaging , by demonstrating that the cavity is occupued by extension of the submandibular gland , established a definitive and solid diagnosis of SBC. In agreement with Branstetter et al (7), MR imaging should be considered a primary diagnostic technique in cases where SBC is suspected.
Recognition of the lesion should preclude any treatment or surgical exploration.
References
1. Stafne EC. Bone cavities situated near the angle of mandible. J Am Dent Assoc 1942;29:1969-72. [ Links ]
2. Tolman DE, Stafne EC. Developmental bone defects of the mandible .Oral Surg Oral Med Oral Pathol 1967;24:488-90. [ Links ]
3. Lello GE, Makek M. Stafnes mandibular lingual cortical defect. Discussion of aetiology. J Maxillofac Surg 1985;13:172-6. [ Links ]
4. Reuter I. An unusual case of Stafne bone cavity with extra-osseous course of the mandibular neurovascular bundle. Dentomaxillofac Radiol 1998;27:189-91. [ Links ]
5. Grellner TJ, Frost DE, Brannon RB. Lingual mandibular bone defect ; report of three cases. J Oral Maxillofac Surg 1990;48:288-96. [ Links ]
6. Barak S, Katz J, Mintz S. Anterior lingual mandibular salivary gland defect: a dilemma in diagnosis. Br J Oral Maxillofac Surg 1993;31:318-20. [ Links ]
7. Branstetter BF, Weisman JL, Kaplan SB. Imaging of a Stafne bone cavity: what MR adds and why a new name is needed. Am J Neuroradiol 1999;20:587-9. [ Links ]
8. Killey HC, Kay LW, Seward GR. Benign cystic lesions of the jaws, their diagnosis and treatment. London, Churchil Livingstone; 1977. p. 146-9 [ Links ]
9. Boyle CA, Horner K, Coulthard P, Fleming GI. Multiple stafne bone cavities: a diagnostic dilema.Dent Update 2000;27:494-7. [ Links ]
10. de Courten A, Kuffer R, Samson J, Lombardi T. Anterior lingual mandibular salivary gland defect (Stafne defect) presenting as a residual cyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:460-4. [ Links ]
11. Poveda R. Stafnes cavity. Med Oral 2004;9:271. [ Links ]
12. Belmonte- Caro R, Velez- Gutierrez MJ, Garcia De La Vega- Sosa FJ, Garcia- Perla- Garcia A, Infante- Cossio PA, Diaz- Fernandez JM, et al. A Stafnes cavity with unuaual location in the mandibular anterior area. Med Oral 2005;10:173-9. [ Links ]
13. Tsui SH, Chan FF. Lingual mandibular bone defect: case report and review of the literature. Aust Dent J 1994;39:368-71. [ Links ]
14. Tonigana K, Kuga Y, Kubota K, Ohba T. Stafnes bone cavity in the anterior mandible . Dentomaxillofac Radiol 1990;19;28-30. [ Links ]
15. Oikarinen VJ, Wolf J, Julku M. A sterosialographic study of developmental mandibular bone defects(Stafnes idiopathic bone cavities). Int J Oral Surg 1975;4:51-4. [ Links ]
16. Ariji E, Fugiwara N, Tabata O,Nakayama E, Kanda S, Shiratsuchi Y et al. Stafnes bone cavity ; classification based on outlune and content determined by computer tomography. Oral Surg Oral Med Oral Pathol 1993;76:375-80. [ Links ]
17. Slasky BS, Bar-Ziv J. Lingual mandibular bony defects: CT in the buccolingual plane. J Comput Assist Tomogr 1996;20:439-43. [ Links ]
![]() Correspondence:
Correspondence:
Prof. Lipa Bodner,
Department of OMF Surgery,
Soroka University Medical Center,
P.O. Box 151,
Beer-Sheva 84101, Israel.
Fax: 972-8-6403651
E-mail: lbodner@bgu.ac.il
Received: 23-12-2005
Accepted: 29-03-2006