Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.6 nov./dic. 2006
Mandibular odontogenic myxoma. Reconstructive considerations by means of the vascularized fibular free flap
Mixoma odontogénico mandibular. Consideraciones reconstructivas mediante el empleo del colgajo libre vascularizado de peroné
Raúl González García, Francisco J. Rodríguez Campo, Luis Naval Gías, Mario F. Muñoz Guerra,
Jesús Sastre Pérez, Francisco J. Díaz González
Department of Oral and Maxillofacial Surgery. University Hospital La Princesa, Madrid, Spain
ABSTRACT
The odontogenic myxoma is a rare entity located in mandible and upper maxilla. Due to its local aggressiveness, wide surgical excision is mandatory. Several surgical techniques have been described for the reconstruction of segmental mandibular defects. In comparison with other free flaps, the vascularized free fibular flap (VFFF) supports the longest amount of bone and, due to the nature of the vascular supply a complete freedom in location of the osteotomy is present. A precise mandibular arc can be performed following bone resection. We suggest the performance of the "in situ" VFFF technique in order to recreate mandibular contour by means of several osteotomies, while the pedicle is still attached to the leg. Substantial decrease in surgical time is obtained. With the "double-barrel" technique and subsequent osseointegrated implants, good results are obtained in the reconstruction of dentate patients without maxillary atrophy. We present two new cases of large odontogenic mandibular myxoma. Wide surgical excision by means of hemimandibulectomies and subsequent reconstruction with VFFF were performed.
Key words: Odontogenic myxoma, vascularized fibular free flap, mandibular reconstruction.
RESUMEN
El mixoma odontogénico constituye una entidad rara de localización posterior en mandíbula y maxilar superior. Debido a su agresividad local, se hace necesaria la resección quirúrgica con márgenes amplios. Se han descrito diversas técnicas quirúrgicas para la reconstrucción de defectos mandibulares segmentarios. El colgajo microvascularizado de peroné, en comparación con otros colgajos óseos, aporta la mayor longitud de hueso y, debido a la naturaleza de su aporte vascular, confiere una completa libertad en la selección del lugar de osteotomía, con la posibilidad de recrear un arco mandibular preciso, tras la resección ósea. Sugerimos la realización de la técnica de preformado in situ del peroné, mediante la cual se replica el contorno mandibular por medio de osteotomías mientras el pedículo vascular del injerto sigue unido a la pierna. Se consigue, de este modo, disminuir substancialmente el tiempo de isquemia del colgajo. La realización de la técnica en "doble barra" y la colocación posterior de implantes osteointegrados constituye un método óptimo en la reconstrucción de pacientes dentados sin atrofia maxilar. Presentamos dos nuevos casos de mixoma odontogénico mandibular de grandes dimensiones, que fueron tratados mediante excisión quirúrgica con márgenes por medio de sendas hemimandibulectomías y reconstrucción por medio de un injerto libre vascularizado de peroné.
Palabras clave: Mixoma odontogénico, colgajo libre microvascularizado de peroné, reconstrucción mandibular.
Introduction
With the popularization of microvascular reconstruction techniques, osseous free flaps and other procedures such as distraction osteogenesis have become techniques of great value in the reconstruction of segmental mandibular defects following oncological resective surgery (1,2). Several advantages have been proposed for the VFFF in comparison with other bone free flaps used in mandibular reconstruction. These advantages are a two-team approach, longer bone and freedom in the choice of the manbibular osteotomy site, due to its periostal irrigation.
However, due to the limited fibular diameter in relation to dentate patients without maxillary atrophy, vertical distance to the occlusal plane can be significant following placement of implants.
Bähr et al (3) referred the use of two juxtaposed fibular segments for the creation of a double barrel. Later, Guerra et al (4) described the "partial double-barrel" technique for simultaneous reconstruction of the mandibular ramus and body in large mandibular segmental defects. These large defects are not exclusive of surgeries for malignant tumors, but also for locally aggressive benign tumors such as the mandibular odontogenic myxoma, and can be present following ablative surgery for these benign tumors. We report two new cases of large mandibular odontogenic myxomas and subsequent reconstruction by means of the "in situ" VFFF and the "double barrel" technique, respectively.
Clinical cases
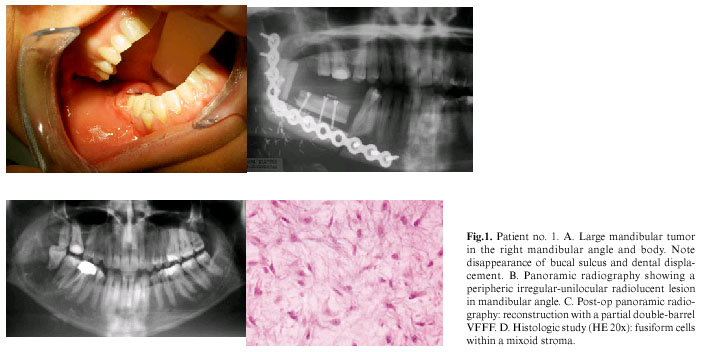
Clinical Case 1
A 34-year old woman was referred to our Department presenting a right expansive mandibular mass for 10 months. The patient referred continuous pain in right hemimandibular region, with extension to the right ear. Neither limitation of mouth opening nor inferior labial paresthesia was referred by the patient. Physical examination revealed a 2.5 to 3-cm mass in the right mandibular angle with displacement of the external mandibular cortex. Intraoral examination showed a poor limited firm mass with expansion of both mandibular walls and loss of integrity of the inner mandibular cortex. Expanded surrounding soft tissue and displacement of right molars were also noted. The panoramic radiograph showed an osteolitic poor-defined unilocular radiolucent lesion in the right mandibular angle and retromolar trigone. The canal of the inferior alveolar nerve was preserved. Facial computerized tomogram (CT) showed a 25-mm expanded osteolitic lesion in the right mandibular angle with destruction of both mandibular walls, homogeneous hypodensity with peripheral septi and an aggressive radiological pattern. Diagnostic biopsy showed the presence of fusiform cells in a mixoid estroma, compatible with odontogenic myxoma.
Wide surgical excision of the lesion was subsequently performed by means of a combined intraoral and extraoral approach.
Segmental mandibulectomy from premolar region to ipsilateral mandibular ramus and coronoid process was performed. Primary mandibular reconstruction by means of the double-barrel VFFF was performed. Arterial anastomosis between the peroneal artery and the right upper thyroid artery was performed. Venous anastomosis between the concomitant peroneal vein and the right truncus tirolinguofacialis was also performed. The histological study showed a 4-cm pale fascicled lesion with surgical free margins. Microscopically a fusiform or spindle cell proliferation with vesicled nucleus was observed in a highly Alcian blue-stained homogeneous mucoid estroma. Small osteoid nests partially mineralized were also observed. Postoperative period healed uneventfully.
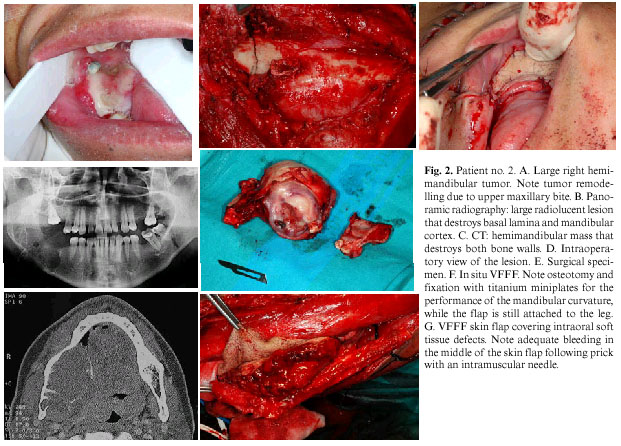
Clinical Case 2
A 33-year old man was referred from another center with a large 6-month right hemimandibular mass that had experimented progressive growing. The patient referred previous molar exodontia in the 4th quadrant without local severe pain. Physical examination showed a 5-6 cm bone tumor with affectation of both mandibular walls extending form the second premolar to the middle of the right mandibular ramus, with affectation of the ipsilateral medial pterigoid muscle.
A CT showing a 5.5 x 4.8 x 3 cm mandibular tumoral lesion was performed. Internal mandibular wall was destroyed and displacement of muscles and structures of the base of the tongue with affectation of most of the right mandibular body and ramus and preservation of the condyle was demonstrated. The biopsy showed a mixoid lesion with reactive linfo-plasmocitic inflammatory component. It was positive for vimentine, CD 138, kappa, lambda and partially positive for actin. Immunohistochemistry showed negativity for S-100, CD 31 and CD 68. Diagnosis was odontogenic mandibular myxoma.
Wide surgical excision with a combined intraoral and extraoral approach was performed. Segmental mandibulectomy from the contralateral canine region to the ipsilateral coronoid process was perfomed. Condyle was preserved. Primary reconstruction my means of VFFF was achieved. The flap was harvested and performed in situ. The new mandible was performed "in situ" and shaped over the original mandible. After it, vascular anastomoses between peroneal and facial arteries and peroneal vein and tyrolinguofacialis truncus were performed. Histologic study showed mandibular odontogenic myxoma with no involved margins. Immediate follow-up developed no complications (fig.2).
Discusion
Odontogenic myxoma is a non-encapsulated benign tumor of the jaws that rarely occurs. It derives from the dental mesenchyme or periodontal ligament. Previous studies refer the tip of the incidence in the third decade of the life, and the majority of the cases between 10 and 40 years-old (5). Our two cases surpass the third decade of life, but can be addressed within the range referred in the literature. Globally, it represents 3 to 6% of all odontogenic tumors. Although its most frequent location is the posterior mandible, other locations such as the incisive sector, upper maxilla and mandibular condyle must be considered (6). Present cases showed large lesions in the majority of the mandibular body, with extension to the ramus in the second case.
Clinically, myxoma has been described as a slow-growing asymptomatic mass. The presence of pain, paresthesia, ulceration and dental mobility has been referred in the literature (7,8). One of our patients referred pain with irradiation to the auricular region. Both of our patients showed a large mass as the main aspect in physical examination. In the X-ray examination, it may show uni- or multi- locular "soap-bubble" or "honey-panel" pattern, with cortical expansion and dental displacement (9). External and internal cortical displacement can be very evident, with bone destruction and soft tissue protrusion. Both of our cases showed this cortical expansion. The second case showed a fracture of the internal cortex with inclusion and displacement of bony fragments. No midline cross-over was observed in any case. Unilateral involvement was observed in all the cases, as it is reported in the literature (5). Biopsy is mandatory to obtain definitive diagnosis. Differential diagnosis must be established with other clinically similar entities, such as simple cyst, ameloblastoma, intraosseous haemangioma, giant cell granuloma, osseous aneurismatic cyst and metastasis (9). Characteristic radiological imaging "in sun rays" of mandibular sarcomas may be present in cases of myxoma with cortical perforation, as it was observed in the second case.
Histologically, fusiform or spindle cells along a mucoid estroma of condroitin sulphate and hialuronic acid was observed. For diagnosis, It is not necessary the presence of islands of odontogenic epithelium (10). The presence of distrophic calcification in the first case is very unusual and has been rarely reported in the literature (11). Immunohistochemically, it has been reported the presence of mesenchimal markers such as muscle-specific actine, vimentine and less frequently S-100 protein (6), which was absent in our second case.
Despite surgery has been established as the treatment of choice for these tumors, no unanimous consensus exists concerning the extension of surgery. Disparity in surgical criteria may be in relation to the tumor size. Thus, our group and other authors (12) advocate for a wide surgical excision to avoid the high local recurrence rate which is, according with some studios, up to 25% of the cases. This has been referred by Smith et al. (13) as a consequence of inadequate tumor excision. The possibility to perform primary reconstruction with optimal aesthetical and functional results encourages us to choose this option, moreover if we consider the local aggressiveness showed by this tumor. However, other authors (14) advocate for a conservative surgery based upon enucleation and curettage. Under our point of view this option should be only acceptable for small-sized myxomas.
With the advent of microvascular surgery, the use of the VFFF has become an optimum method in the reconstruction of mandibular post-ablative oncologic defects. In comparison with other osseous vascularized free flaps, the fibula supports the longest bone supply and allows for posterior optimum implant rehabilitation (2), with low donor site morbidity (15). In fact, this lower flap failure rate can be explained by the presence of a long vascular pedicle that avoids the necessity to interpose vein grafts between the donor vessel and the recipient vessel.
VFFF allows the reconstruction of large mandibular ramus and body defects, even in cases with bilateral involvement. In fact, a segment of bone up to 20-26 cm can be obtained. Rich periostal irrigation of the fibula supports the performance of multiple osteotomies that allow the design of a several-segmented barrel, in relation to a pre-designed model (generally a mandibular bridging plate). In fact, fibula tolerates osteotomies as small as 2 cm, wide enough to replicate the mandibular curvature. Together with its bone particularities, we consider very adequate the incorporation of a skin paddle in order to allow an easy control of flap viability and an easy restoration of associated soft tissue defects.
The "in situ" VFFF technique (16) is used in the context of a mandibular bridging plate designed according to patient mandibular curvature. This model is performed previous to mandibulectomy. Both fibular osteotomies are performed without dividing the vascular pedicle that supplies the flap.
Several osteotomies with preservation of the periostium can be done in order to adequate the fibula to the mandibular bridging plate. Posteriorly miniplates are used to fix the osteotomies. Finally, flap is transferred to the recipient site.
Several modifications have been referred in the literature in relation to VFFF (3,5). Due to its limited diameter in comparison to mandibular height, distance to the occlusal plane may be important, preventing for adequate implant rehabilitation. In order to obviate this problem, Bähr et al (3) described the use of both fibular segments one up into the other, in a "double-barrel" conformation. This technique provides more bone height and substantially reduces vertical distance to the occlusal plane. Thus, it constitutes an optimum method to compensate narrowness of the fibula in patients with non-atrophied mandibles. A modification of this technique was suggested by Muñoz-Guerra et al (2), by means of a "partial double-barrel" for the reconstruction of mandibular ramus and body. In a series of 42 patients with post-ablative mandibular defects that were reconstructed with VFFF, we refer 8 patients in whom a double-barrel VFFF was performed, five of them with posterior implant rehabilitation. Good aesthetic results and adequate implant rehabilitation were obtained.
Radical surgical resection of mandibular odontogenic myxoma with primary reconstruction must be the treatment of choice. The use of VFFF is an optimum method for mandibular reconstruction. We advocates for the use of the double-barrel technique in both its modalities, in order to obtain adequate mandibular height in patients without mandibular atrophy. In contrast with previous considerations (3) in relation to replication of mandibular contour when the fibula is still attached to the leg, we think that it can be performed successfully with a careful technique. This technique maintains flap irrigation for a longer period of time. We should expect better results in terms of flap survival. More controlled and randomized prospective studies are necessary to compare this technique with conventional performance of mandibular arc in the recipient site.
References
1. González-García R, Rubio-Bueno P, Naval-Gías L, Rodríguez-Campo FJ, Escorial-Hernández V, Martos PL, et al. Internal distraction osteogenesis for mandibular reconstruction. Clinical experience in ten cases. Plast Reconstr Surg [in press]. [ Links ]
2. Muñoz-Guerra MF, Naval-Gías L, Rodríguez-Campo FJ, Díaz-González FJ. Vascularized free fibular flap for mandibular reconstruction: a report of 26 cases. J Oral Maxillofac Surg 2001;59:140-4. [ Links ]
3. Bärh W, Stoll P, Wächter R. Use of the "double barrel" free vascularized fibula in mandibular reconstruction. J Oral Maxillofac Surg 1998;56:38-44. [ Links ]
4. Guerra MF, Gías LN, Campo FJ, Pérez JS, de Artiñano FO, González FJ. The partial double-barrel free vascularized fibular graft: a solution for long mandibular defects. Plast Reconstr Surg 2000;105:1902-3. [ Links ]
5. Simon EN, Merkx MA, Vuhahula E, Ngassapa D, Stoelinga PJ. Odontogenic myxoma: a clinicopathological study of 33 cases. Int J Oral Maxillofac Surg 2004;33:333-7. [ Links ]
6. Halfpenny W, Verey A, Bardsley V. Miyoma of the mandibular condyle. A case report and review of the literature. Oral Surg Oral Med Oral Pathol Endod 2000;90:348-53. [ Links ]
7. Kangur TT, Dahlin DC, Turlington EG. Myxomatous tumors of the jaws. J Oral Surg 1975;33:523-8. [ Links ]
8. Hernández Vallejo G, Cohn C, García Penín A, Martínez Lara S, Llanes Menéndez F, Montalvo Moreno JJ. Myxoma of the jaws. Report of three cases. Med Oral 2001;6:106-13. [ Links ]
9. Peltola J, Magnusson B, Happoren RP, Boman H. Odontogenic myxoma-a radiological study of 21 tumors. Br J Oral Maxillofac Surg 1994;32:298-302. [ Links ]
10. Kimura A, Hasegawa H, Satou K, Kitamura Y. Odontogenic myxoma showing epithelial islands with microcystic features. J Oral Maxillofac Surg 2001;59:126-8. [ Links ]
11. Bucci E, Lo Muzio L, Mignogna MD, De Rosa G. Odontogenic myxoma: report of a case with peculiar features. J Oral Maxillofac Surg 1991;49:91-4. [ Links ]
12. Adamo AK, Locricchio RC, Freedman P. Myxoma of the mandible treated by peripheral ostectomy and immediate reconstruction. J Oral Surg 1980;38:530-3. [ Links ]
13. Smith GA, Konrad HR, Canalis RF. Childhood mixomas of the head and neck. J Otolaryngol 1977;6:423-30. [ Links ]
14. Cuestas-Carnero R, Bachur RO, Gendelman H. Odontogenic myxoma: report of a case. J Oral Maxillofac Surg 1988;46:705-9. [ Links ]
15. Hidalgo DA, Rekow A. A review of 60 consecutive fibula free flap mandible reconstructions. Plast Reconstr Surg 1995;96:585-96. [ Links ]
16. González-García R, Muñoz-Guerra MF, Rodríguez-Campo FJ, Naval-Gías L. In-situ generated vascularized fibular free flap for the reconstruction of complete mandibular defects. Plast Reconstr Surg [in press]. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Raúl González García
Servicio de Cirugía Oral y Maxilofacial.
Hospital Universitario La Princesa.
Madrid, España
E-mail: raugg@mixmail.com
Received: 4-06-2005
Accepted: 1-08-2006