Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.6 nov./dic. 2006
Influence of cavity type and size of composite restorations on cuspal flexure
Santiago González López1, Maria Victoria Sanz Chinesta2, Laura Ceballos García3,
Francisco de Haro Gasquet4, Maria Paloma González Rodríguez4
(1) PhD, Profesor Titular de Patología y Terapéutica dental. Facultad de Odontología, Universidad de Granada
(2) Licenciada en Odontologia
(3) PhD, Profesora Contratada Doctor, Facultad de Ciencias de la Salud, Universidad Rey Juan Carlos, Alcorcón, Madrid
(4) PhD, Profesor Asociado de Patología y Terapéutica dental. Facultad de Odontología, Universidad de Granada
ABSTRACT
Objectives: The present study examines the influence of cavity type, and size of composite restorations on cuspal flexure due to polymerization shrinkage.
Methods: Thirty healthy premolars were selected and divided into two experimental groups. Group 1: Mesial, mesio-distal, and MOD cavities were successively prepared in each tooth by means of the SONICSYS approx system (KaVo®) using a nº 2 (small) diamond tip. Group 2: The same cavity preparation sequence was followed but a nº 3 (medium) tip was used.
Cavity preparations were performed and afterwards restored using the same adhesive system and resin composite. Cuspal displacement was measured 15 min after completion of each type of restoration.
Results: Under the experimental conditions used, polymerization shrinkage of composite restorations resulted in an inward deflection of the cusps in all the situations evaluated. The Friedman global test found significant differences according to the cavity type and size (p<0.05). The Wilcoxon test revealed that deflection was significantly affected by the amount of dental tissue lost, since practically no movement was observed in the case of mesial cavities but extensive displacements were recorded for MOD restorations (p<0.05). However, no influence of bucco-lingual width on cuspal flexure was detected by the Students t test (p>0.05).
Conclusions: The present study demonstrates that significantly higher cuspal deflection is observed in MOD restorations, showing that the degree of dental removal influences the cuspal flexure from polymerization shrinkage of composite restorations.
Key words: Cuspal flexure, cuspal deflection, cusp movement, polymerization shrinkage, cavity type.
Introduction
Current light-cured composite resins offer excellent aesthetics, improved mechanical properties and good bonding to tooth structure, when placed in combination with adhesive systems, accounting for their wide use in contemporary restorative dentistry. However, all resin-based materials undergo contraction inherent to the polymerization reaction, which ranges from 2.7% to 7.1% (1,2).
This shrinkage subjects the tooth structure to mechanical stresses may cause enamel fracture, cracked cusps, cuspal movement, and opening of the restoration margins, which may result in microleakage and postoperative pain (3-6).
The polymerization shrinkage of composites in a cavity generates stress that can be transmitted via the adhesive interface to adjacent dental tissues (3,7), producing dental deformation. According to Versluis et al. (8), tooth deformation offers the closest relationship to shrinkage stresses and can be quantified, whilst many of the other clinical symptoms are substantially subjective. This deformation is often determined by measuring the flexure of cusps (3, 7, 9, 10). Linear displacement of the cusps was previously reported using other devices such as Linear Variable Differential Transformers (LVDTs) and Direct Current Differential Transformers (DCDTs) (11), which are reported to be highly sensitive to the vertical angle of inclination (12). Cuspal deflection has also been measured with a digital micrometer (13) and by using strain gauges to measure strains generated in the deformed cusp (12, 14-16).
Reports on the degree of cuspal deflection range from 6 to 47 µm,(3, 7-10, 17) depending on the size of the restoration (9), cavity design (10), stiffness and flow of composite, bonding system applied, placement technique, light curing lamp intensity, and curing mode (6).
Cusps of teeth with large cavity preparations have been reported to exhibit greater deflection than those of teeth with small cavities (9). Loss of strategic dental structures, namely the marginal ridges, and the increased width of the isthmus region, reduce tooth stiffness and increase cusp flexibility (11, 14-17). Furthermore, a larger volume of composite may result in greater shrinkage forces (7-9). It has also been proposed that repeated functional loading causes fatiguing of the restored tooth and ultimately results in failure (18).
The present study was designed to determine the effects of three cavity designs of small or medium size on the magnitude of cuspal deflection caused by polymerization shrinkage of composite restorations. The null hypothesis was that there is no difference in cuspal deflection among mesial, mesio-distal, and MOD cavity preparations of small and medium size.
Materials and methods
Thirty intact non-carious human maxillary first premolars extracted for orthodontic reasons were used in the present study. The teeth were cleaned and stored in buffered saline plus 0.5% thymol at 4º C until use. Teeth were free of cracks or other defects after visual and stereomicroscopic examination and had regular occlusal anatomy and similar crown sizes.
Each tooth was mounted vertically in a plastic ring with acrylic resin (Ortocryl EQ, Dentautum, Germany), leaving 2 mm of the root surface exposed to mimic the support of alveolar bone in a healthy tooth. Samples were connected to a simulated pulpal pressure system using a previously described method (19), maintaining the tooth under pressure and humidity conditions throughout the preparation and measurement period. Adhesive techniques were then used to fix a 1.5 mm diameter glass ball to each cuspal vertex as reference points for intercuspal distance measurements.
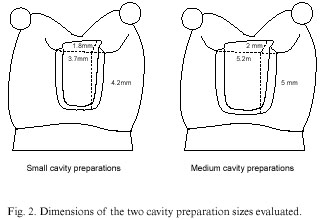
The teeth were randomly divided into two experimental groups (n=15). In the first group, mesial, mesio-distal, and MOD cavities were successively prepared by means of the SONICSYS approx system (KaVo, Biberach, Germany) using a nº 2 (small) diamond tip. In the other group, the same cavity preparation sequence was performed but a nº 3 (medium) tip was used. Cavity preparation types are shown in Figure 1.
In MOD cavity preparations, both proximal boxes were connected with an occlusal extension of approximately one-third of the bucco-lingual width of the tooth and 2 mm in depth. The cavity dimensions are shown in Figure 2.
After preparation of each cavity type, the distance between reference balls was measured using a precision micrometer (Mitutoyo, 293-561, Japan) and recorded as the initial distance.
In both experimental groups, mesial cavities were filled and the intercuspal distance was measured 15 min later. Afterwards, mesial composite restorations were removed from each specimen and distal cavities were prepared. After restoration of both cavities, the intercuspal distance was again recorded 15 min after composite polymerization. Finally, both composite restorations were removed and a MOD cavity was performed and filled, followed by measurement of the cuspal displacement 15 min after completion of the restoration
In all cases, the matrix band was placed without using a retainer in order to avoid any tension on the cusps. All cavities were treated with 37% phosphoric acid for 15 s, and the Syntac Single adhesive system (Ivoclar, Schaan, Liechtenstein) was then applied following the manufacturers recommendations. The same resin composite, Tetric Ceram (Ivoclar, Schaan, Liechtenstein), was used to restore all samples. Cavities were filled with horizontal layers in two increments, the first to one-half the cavity height and the second completing the restoration. In MOD restorations, the first increment filled the lower half of the proximal boxes and the second layer completely filled both boxes and the occlusal preparation. Each increment was light-cured for 40 seconds with the light source (Optilux 401, Demetron Research Corp, Danbury, Conn), which was tested with a radiometer (Cure Rite, Efos Inc, Mississawga; Canada) for a light output = 450 mW/cm2 before each application. The occlusal aspect of the restorations was carved before polymerization to approximate the normal occlusal anatomy of a maxillary premolar tooth.
All measurements were performed by the same operator and ten consecutive measurements were recorded for each specimen and experimental situation and the mean was used for the subsequent statistical analysis.
The Friedman global test was used for the global comparison among the three cavity types (M, MD and MOD) for each cavity size (small and medium). After finding significant differences among the three cavity designs, paired comparisons were made with the Wilcoxon test. Comparison of the cuspal movements recorded in either small or medium cavities was performed by Students t test. Statistical significance was set in advance at the 0.05 confidence level. All data were analyzed by means of SPSS 11.0 for Windows software (SPSS Inc., Chicago, IL, USA).
Results
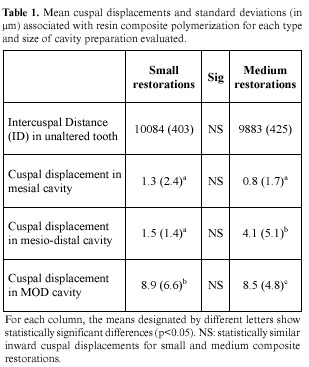
The values of cuspal deflection obtained for each cavity type and size are shown in Table 1. Type of cavity significantly influenced cuspal deflection. In small cavity preparations, MOD restoration was related to a significantly greater reduction in intercuspal distance compared with mesial or mesio-distal restorations, whereas no difference in distance reduction was observed between the restoration of mesial and mesio-distal cavities. In medium restorations, MOD restoration was again associated with a greater reduction in intercuspal distance and there was also a significantly greater reduction in mesio-distal versus mesial cavities.
No influence of cavity size on the inward movement of the cusps was detected, and the small and medium resin composite restorations showed a similar behavior.
Discussion
Polymerization shrinkage of composite restorations resulted in an inward deflection of the cusps for all the experimental groups evaluated, in agreement with previous reports (3, 6, 7, 9). Nevertheless, values of displacements in the present study were lower than other reported values (9, 17), probably because of differences in experimental design. In order to maximize cuspal movement due to polymerization shrinkage of resin composite, large MOD restorations are usually prepared (6, 7, 9). However, the objective of the present study was to evaluate the contribution of different dental structures to tooth stiffness, so that more conservative cavities were prepared, producing less tooth structure removing.
The relative effects of cavity size and sequential cavity restoration were determined by linear displacement of the cusps in a non-destructive testing procedure (20). Composite restorations were inserted, removed, and replaced by more extensive designs. This sequence simulates the clinical situation, where the most common treatment is the replacement of previous failed restorations (21, 22). This approach allowed each tooth to be used as its own control (15), minimizing the effect of variations in morphology or stiffness among teeth, which have been reported to increase after cavity preparation (12). Accordingly, only a small sample size is required to achieve statistical significance, improving the efficiency of the experimental design and statistical analysis (11, 15, 20).
The results are given in the table in absolute values of cuspal displacement as they are easier to grasp in this manner and the dispersion was minimal. The type of cavity preparation significantly influenced the extent of cuspal flexure (10, 15). Movement of the cusps when mesial cavity preparations were restored was minimal, practically non-existent (1 µm). The presence of the distal marginal ridge and the preservation of the occlusal enamel and dentin connecting the cusps may have prevented greater cusp displacement (15, 23). Thus, the elimination and subsequent restoration of the distal marginal ridge increased cuspal deflection only in larger restorations (4.1 µm). Nevertheless, the reductions in cuspal distance recorded were very small and may not be clinically relevant.
Significantly higher cuspal deflection was observed in MOD restorations (9 µm). The degree of cuspal flexure is known to be directly related to loss of dental structure. Larger cavity preparations cause a reduction in tooth stiffness (10, 11, 24, 25) and require more composite resin when restored, producing greater contraction forces (9).
In the present study, the cuspal displacements recorded for small and medium restorations were statistically similar. This finding contrasts with other studies (7, 9) that reported a greater cuspal deflection in teeth with large cavities than in those with small cavities. One possible reason is that, in those studies, there was a marked size difference between the small and large cavities. Moreover, the preservation of other strategic structures, such as the remaining dentin above the pulp chamber and the distal marginal ridge, seems to play a more important role in avoiding tooth weakening (23).
The inward deflection of the cusps is an expression of the polymerization kinetics and may be affected by many factors. It has been reported that cusps recover their original position after inward deflection because of shrinkage of composite restorations and that this recovery is strongly influenced by tooth hydration conditions and cavity size (9). To minimize these effects, intercuspal distances were measured 15 min after polymerization, because the majority of cusp movement is reported to occur within this time period (9, 24) and the teeth were fully hydrated. These study conditions may have influenced the low values of cuspal movement observed. Other factors that may affect cuspal deflection are the composite system and corresponding bonding system (6). The chemical curing of composites takes longer, showing lower resulting stress versus light-curing (26). Only one type of system was evaluated in the present study, and other systems, including different light curing sources or filling techniques, may produce different effects on cuspal movement (6, 8). The layering of resin composite has been proposed to reduce the composite mass to be polymerized and the resulting shrinkage stress (27), although Versluis et al. (28) reported that incremental techniques may produce higher stresses at the restorative interface in comparison with bulk filling. On the other hand, other in vitro studies reported no clear differences between these approaches (13, 29).
The present study demonstrates that the degree of dental removal influences the cuspal flexure from polymerization shrinkage of composite restorations. Cuspal movement indicates residual stresses in the tooth structure (8), which may cause failure during composite curing or act as a preloading, facilitating tooth fracture under occlusal loads (7, 18, 30). Conservative cavity designs are recommended for resin composites in order to reduce these stresses, avoiding classic designs for amalgam.
References
1. Feilzer AJ, de Gee AJ, Davidson CL. Curing contraction composites and glass- ionomer cements. J Prosthet Dent 1988;59:297-300. [ Links ]
2. Hervas-García A, Martínez-Lozano MA, Cabanes-Vila J, Barjau-Escribano A, Fos-Galve P. Composite resins. A review of the materials and clinical indications. Med Oral Patol Oral Cir Buc 2006;11:E215-20. [ Links ]
3. Alomari QD, Reinhardt JW, Boyer DB. Effect of liners on cusp deflection and gap formation in composite restorations. Oper Dent 2001;26;406- 11. [ Links ]
4. Bausch JR, de Lange K, Davidson CL, Peters A, de Gee AJ. Clinical significance of polymerization shrinkage of composite resins. J Prosthet Dent 1982;48:59-67. [ Links ]
5. Eick JD, Welch FH. Polymerization shrinkage of posterior composite resins and its possible influence on postoperative sensitivity. Quintessence Int 1986;17:103-11. [ Links ]
6. Abbas G, Fleming GJ, Harrington E, Shortall ACC, Burke FJT. Cuspal movement and microleakage in premolar teeth restored with a packable composite cured in bulk or increments. J Dent 2003;31:437-44. [ Links ]
7. Meredith N, Setchell DJ. In vitro measurement of cuspal strain and displacement in composite restored teeth. J Dent 1997;25:331-7. [ Links ]
8. Versluis A, Tantbirojn D, Pintado MR, DeLong R, Douglas WH. Residual shrinkage stress distributions in molars after composite restoration. Dent Mater 2004;20:554-64. [ Links ]
9. Suliman AA, Boyer DB, Lakes RS. Cusp movement in premolars resulting from composite polymerization shrinkage. Dent Mater 1993;9:6-10. [ Links ]
10. Pearson GJ, Hegarty SM. Cusp movement of molar teeth with composite filling materials in conventional and modified MOD cavities. Br Dent J 1989;166:162-5. [ Links ]
11. Panitvisai P, Messner HH. Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod 1995;21:57-61. [ Links ]
12. Jantarat J, Panitvisai P, Palamara JEA, Messer HH. Comparison of methods for measuring cuspal deformation in teeth. J Dent 2001;29:75-82. [ Links ]
13. González- López S, Lucena- Martín C, de Haro- Gasquet F, Vilchez- Díaz MA, de Haro- Muñoz C. Influence of different composite restoration techniques on cuspal deflection: an in vitro study. Oper Dent 2004;29:656-60. [ Links ]
14. Morin DL, Douglas WH, Cross M, DeLong R. Biophysical stress analysis of restored teeth: experimental strain measurement. Dent Mater 1988;4:41-8. [ Links ]
15. Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod 1989;15:512-6. [ Links ]
16. Sakaguchi RL, Brusr EW, Cross M, DeLong R, Douglas WH. Independent movement of cusps during occlusal loading. Dent Mater 1991;7:186-90. [ Links ]
17. Causton BE, Miller B, Sefton J. The deformation of cusps by bonded posterior composite restorations: an in vitro study. Br Dent J 1985;159:397-400. [ Links ]
18. Ausiello P, Apicella A, Davidson CL, Rengo S. 3D-finite element analyses of cusp movements in a human upper premolar, restored with adhesive resin-based composite. J Biomechanics 2001;34:1269-77. [ Links ]
19. Lucena-Martín C, González- Rodríguez MP, Ferrer-Luque CM, Robles-Gijón V, Navajas JM. Study of the shear bond strength of five one-component adhesives under simulated pulpal pressure. Oper Dent 1999;24:73-80. [ Links ]
20. Linn J, Messer H. Effect of restorative procedures on the strength of endodontically treated molars. J Endod 1994;20:479-85. [ Links ]
21. Forss H, Widstrom E. Reasons for restorative therapy and the longevity of restorations in adults. Acta Odont Scand 2004;62:82-6. [ Links ]
22. Mondelli J, Steagall L, Ishikiriama A, Navarro M, Soares FB. Fracture strength of human teeth with cavity preparations. J Prosthet Dent 1980;43:419-22. [ Links ]
23. Mjor IA, Shen C, Eliasson ST, Richter S. Placement and replacement of restorations in general dental practice in Iceland. Oper Dent 2002;27:117-23. [ Links ]
24. McCullock, Smith BGN. In vitro studies of cuspal movement produced by adhesive restorative materials. Br Dent J 1986;161:405-9. [ Links ]
25. Blaser BK, Lund MR, Cochran MA, Potter RH. Effects of designs of class 2 preparations on resistance of teeth to fracture. Oper Dent 1983;8:6-10. [ Links ]
26. Kuiks RH, Fennis WMM, Kreulen CM, Barink M, Verdonschol N. Does layering minimize shrinkage stresses in composite restorations?. J Dent Res 2003;82:967-71. [ Links ]
27. Neiva IF, de Andrada MA, Baratieri LN, Monteiro Jr. S, Ritter AV. An in vitro study of the effect of restorative technique on marginal leakage in posterior composites. Oper Dent 1998;23:282-9. [ Links ]
28. Versluis A, Tantbirojn D, Douglas WH. Do dental composites always shrink toward the light?. J Dent Res 1998;77:1435-45. [ Links ]
29. Loguercio AD, Reis A, Ballester RY. Polymerization shrinkage: effects of constraint and filling technique in composite restorations. Dent Mater 2004;20:236-43. [ Links ]
30. González- López S, Vilchez Díaz MA, de Haro- Gasquet F, Ceballos L. de Haro- Muñoz C. Cuspal flexure of teeth with composite restorations subjected to occlusal loading. J Adh Dent. In press. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Santiago González- López.
Facultad de Odontología, Universidad de Granada
Campus Universitario de la Cartuja s/n,
18071 Granada, España.
E-mail: sglopez@ugr.es
Received: 29-01-2006
Accepted: 3-06-2006