My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
On-line version ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 n.3 May. 2007
Sinus histiocytosis with massive lymphadenopathy. Is the lymph node enlargement always massive?
Ritesh Sachdev1, Namrata Setia1, Shyama Jain2
(1) Residents. (2) Professor. Department of Pathology, Maulana Azad Medical College, New Delhi. India
ABSTRACT
Sinus histiocytosis with massive lymphadenopathy (SHML) is a benign proliferating histiocytic disorder, predominantly of lymph nodes with extra-nodal involvement in some cases. It is a self-limiting disease and has a good prognosis; however some patients need steroid therapy. Therein lays a need to differentiate it from other lympho proliferative disorders of poorer prognosis. Clinically, it is suspected only when there is a significant lymph node enlargement in younger age group as the term signifies. Recently, we came across a case where a middle-aged female presented with a subtle swelling in submental region, clinically suspected of reactive or tubercular etiology. However on fine needle aspiration cytology, the smears showed many histiocytes, some of them showing lymphocytes and plasma cells in their cytoplasm, a morphological feature called as emperipolesis classically seen in SHML. The present case is reported because of unusual clinical presentation and possibly the need for a revision of existing terminology.
Key words: Rosai-Dorfman disease, sinus histiocytosis, lymphadenopathy.
Introduction
Sinus histiocytosis with massive lymphadenopathy (SHML), also known as Rosai-Dorfman disease (RDD), is a rare entity of lymph nodes and was first described by Rosai and Dorfman in 1969. (1) The disease affects predominantly the younger age group. The common presentations include massive lymphadenopathy in the head and neck region, which is typically bilateral, nontender and self-limiting. It is a benign proliferative histiocytic disorder morphologically characterized by emperipolesis. (1) Extra-nodal involvement is not rare (43%); (2) sites include skin, nasal cavity, para nasal sinuses, eyelids, orbit, bone and central nervous system. (3)
We report an interesting case of a middle-aged woman who presented with minimal submental swelling and was clinically suggestive of reactive lymphoid hyperplasia (RLH) or tuberculous lymphadenopathy (TBL); however on fine needle aspiration cytology (FNAC) it was diagnosed as RDD.
Case Report
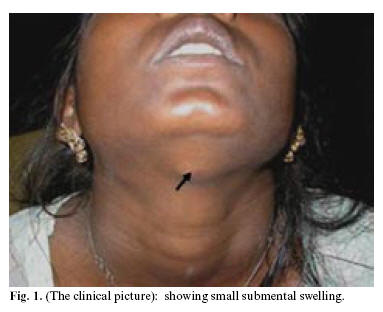
A 48-year female presented with history of low-grade fever off and on, malaise, cough, anorexia and lassitude since one year. There was no history of contact or family history of tuberculosis. On clinical examination, there was a small sub mental lymph node measuring 1x 0.8 cms in size (figure 1); for which she was given a course of antibiotics but showed no response to treatment.
The laboratory investigations showed anemia with hemoglobin of 10 gm/dl, the ESR (erythrocyte sedimentation rate) was raised to 40 mm in first hour. FNAC was done thrice in a private laboratory; reported twice as RLH and the third FNAC suggested possibilities of lympho proliferative disorder (LPD).
The patient was later referred to our centre for FNAC from lymph node. The Giemsa stained smears showed a polymorphous picture with presence of predominantly histiocytes admixed with a variable population of lymphocytes, plasma cells, neutrophils and few eosinophils. The histiocytes had moderate to abundant cytoplasm, large vesicular nuclei and showed with phagocytosis (emperipolesis) of plasma cells and lymphocytes (figure 2). The cytological diagnosis was suggestive of RDD. On immunocytochemistry (IC), the histiocytes were positive for S-100, CD-68 and, were negative for CD-1a, thus confirming the diagnosis of RDD. The patient was put on steroid therapy; her fever subsided and the swelling almost disappeared. She is still on follow up.
Discussion
Rosai Dorfman disease is a rare, idiopathic histiocytosis. (1) The disorder is thought to occur as a result of immune dysregulation or response to a presumed infectious agent. The stimulation of monocytes/macrophages via Macrophage-Colony-Stimulating-Factor leads to immunosuppressive macrophages, which is a main pathogenesis of RDD. (4)
Clinically mean age of onset is second decade; other features include fever, non-tender bilateral cervical lymphadenopathy, leucocytosis, elevated ESR and polyclonal hypergammaglobulinemia. However, in contrast our patient was a middle-aged woman with a subtle sub mental lymphadenopathy; though she had fever and a high ESR.
The morphological features include a histiocytic proliferation with presence of large histiocytes showing fine vacuoles in the cytoplasm and large vesicular nuclei. The phagocytosis of lymphocytes and plasma cell (emperipolesis) is characteristic. (5) The background population predominantly consists of lymphocytes, plasma cells, neutrophils and few eosinophils. Although the cytomorphological features are well described, diagnostic difficulties may sometimes arise. The common differential diagnoses (D/D) include infectious lesions, reactive lymphoid hyperplasia with sinus histiocytosis (RLHSH), Langerhans cell histiocytosis (LCH), hemophagocytic syndrome and malignant lymphoma. (5-8) A detailed clinical history and careful morphological assessment usually prevents misdiagnosis. The most important D/D is RLHSH and LCH; the features favoring SHML are numerous histiocytes with prominent emperipolesis. On IC histiocytes in RLSH and SHML show strong positivity for S-100 and CD- 68; however in LCH the histiocytes also show positivity for CD1a. Further confirmation of LCH can be done by demonstrating Birbecks granules on electron microscopy.
The course of RDD is usually benign, indolent and self-limiting in most of the patients. Treatment does not appear to be necessary in the majority of patients since the disease does not usually threaten life or organ function. Surgery is generally limited to biopsy to confirm the diagnosis or, to relieve obstructive symptoms. Patients with progressive disease have been treated with corticosteroids, chemotherapy or radiotherapy with variable results. (9) Our patient received corticosteroids to which she responded well.
To conclude, this case should alert the clinician and cytopathologist to the possibility of occurrence of SHML in minimally enlarged lymph nodes. Careful interpretation of FNAC slides along with appropriate marker study would help in early diagnosis and timely management. An increased awareness of such a possibility by the clinician and the pathologist is desired. Moreover, it is suggested that the terminology of massive lymphadenopathy in SHML may be revised to Sinus Histiocytosis with lymphadenopathy (SHL) or use of RDD should be encouraged.
References
1. Rosai J, Dorfman R F. Sinus histiocytosis with massive lymphadenopathy: a newly recognized benign clinicopathologic entity. Arch Pathol 1969;87:63-70. [ Links ]
2. Wenig B M, Abbondanzo S L, Childers E L. Extranodal sinus histiocytosis with massive lymphadenopathy (Rosai Dorfman disease) of the head and neck. Hum Pathol 1993;24:483-92. [ Links ]
3. Foucar E, Rosai J, Dorfman R F. Sinus histiocytosis with massive lymphdenopathy (Rosai Dorfman disease): review of the entity. Semin Diagn Pathol 1990;7:19-73. [ Links ]
4. Middel P, Hemmerlein B, Fayyazi A, Kaboth U, Radzun H J. Sinus histiocytosis with massive lymphadenopathy: evidence for its relationship to macrophages and for a cytokine –related disorder. Histopathology 1999;35:525-33. [ Links ]
5. Stastny J F, Wilkerson M L, Hamati H F, Kornstein M J. Cytologic features of sinus histiocytosis with massive lymphadenopathy. A report of three cases. Acta Cytol 1997;41:871-6. [ Links ]
6. Minguez I, Minguez JM, Bonet J, Penarrocha M, Sanchis JM. Oral manifestations of chronic disseminated histiocytosis. A report of 10 cases. Med Oral 2004; 9:152-4, 149-52. [ Links ]
7. Hernandez-Juyol M, Boj-Quesada JR, Gallego Melcon S. Oral manifestations of Langerhans cell histiocytosis. Case study of a two-year-old boy. Med Oral 2003;8:19-25. [ Links ]
8. Pacino GA, Serrat A, Redondo LM, Verrier A. Langerhans cell histiocytosis: clinical diagnostic features and current concepts. Med Oral 1999;4:607-18. [ Links ]
9. Goodnight J W, Wang M B, Sercarz J A, Fu Y S. Extranodal Rosai- Dorfman disease of the head and neck. Laryngoscope 1996;106:253-6. [ Links ]
![]() Correspondence:
Correspondence:
Dr Shyama Jain
20/59, Lodhi Colony
New Delhi- 110003
India
E-mail: jainshyama@rediffmail.com
Received: 21-05-2006
Accepted: 24-09-2006