Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.7 nov. 2007
Effectiveness of low flow vascular lesions sclerosis with monoetanolamine: Report of six cases
Paulo Rogério Ferreti Bonan1, Leonardo de Paula Miranda2, Danilo Cangussu Mendes2, Alfredo Maurício Batista de Paula1, Sabina Pena Borges Pego3, Hercílio Martelli-Júnior2
(1) MSc,PhD, Stomatology
(2) Graduation Student
(3) DDS and MSc. Department of Dentistry, State University of Montes Claros, Unimontes, Minas Gerais, Brazil
ABSTRACT
Vascular malformations or even hemangiomas need therapeutic intervention if they start to cause clinical symptoms or personal discomfort. Different therapeutic modalities, including cryotherapy, corticosteroids, laser therapy, sclerotherapy, surgery, and/or embolization, can be performed successfully. Sclerotherapy with monoethanolamine is a relatively simple and effective method to treat low flow vascular lesions. We presented a report of six cases of vascular malformations treated with monoethanolamine. There were 3 male and 3 female patients, with an age range of 20 to 68 years. The patients were submitted to applications according to clinical response and/or tolerability. In all cases, low-flow vascular lesions were recorded and submitted to infiltration with 2.5% monoethanolamine, directly into the lesions. The volume applied was approximately the middle of affected area. Vascular lesions were characterized as low-flow due to absence of arterial pulsation and flat consistence. The sclerosis with 2.5% monoethanolamine resulted in complete or partial involution, without severe complications.
Key words: Vascular lesions, sclerotherapy, monoethanolamine, hemangioma.
Introduction
Vascular anomalies comprise a widely heterogeneous group of tumors and malformations. Vascular malformations generally present at birth, and usually persist throughout the lifetime. Most hemangiomas undergo a progressive involution during the first years of life (1,2). Vascular malformations or even hemangiomas require therapeutic intervention if they start to cause clinical symptoms or personal discomfort. Based on individual parameters (such as diameter, location and growth dynamics), different therapeutic modalities, including cryotherapy, corticosteroids, laser therapy, sclerotherapy, surgery, and/or embolization, can be performed successfully (2). Advances in laser surgery as well as sclerotherapy techniques have improved our ability to treat extensive lesions and these have also improved patients quality of life (3).
Sclerotherapy of vascular lesions is a relatively simple, effective, and inexpensive method that is a valuable and promising treatment (4). The sclerosing therapy may cause the complete regression of low flow vascular lesions. Even in the case of partial regression of the angioma, surgery of the remaining lesion has less bleeding (5). Monoethanolamine oleate (MO) is a sclerosing agent accepted for skin vascular lesions and esophageal varices (6-9). Nevertheless, few studies deal with MO efficacy in head and neck vascular malformations, and particularly for intra-oral lesions (10-11). The purpose of this article is to present the effectiveness of MO sclerosing in six patients with low flow vascular lesions of the oral mucosa.
Clinical cases
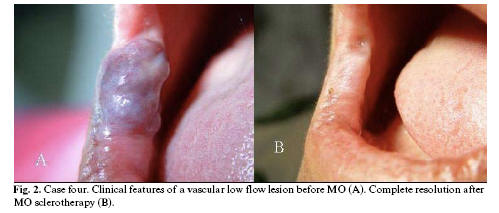
Table 1 shows the main demographic, clinical and therapeutic findings, as well as the side effects and patient´s complaints in this series. Six patients were randomly selected for this analysis. All of them were referred to the Oral Diagnosis Clinic, Unimontes, complaining of oral vascular lesions positive to diascopy. There were 3 male and 3 female patients, with an age range of 20 to 68 years. All were in good systemic health. In all cases, low-flow vascular lesions were recorded and submitted to infiltration with 2.5% MO, diluted in distillated water, directly into the lesions. The volume applied was approximately the middle of affected area. Vascular lesions were characterized as low-flow due to absence of arterial pulsation and flat consistence. Even after needle puncture, no hemorrhage was noted. The patients were submitted to applications according to clinical response and/or tolerability. All patients formally consent with the procedures and were informed about the possible complications after the procedure like edema and intense pain. For all cases, analgesics were prescribed. Clinical and histopathological pictures describing the effectiveness of sclerotherapy are shown in Figures 1-2-3.
Discussion
Vascular low flow lesions may present progressive increase with age, trauma and after partial surgical resection. Ectasic blood vessels and reddish-blue surface are characteristically found in these lesions (2). Solitary presentation or multiple patterns may occur being non-isolated lesions possibly associated with syndromes like Maffuci, Sturge-Weber, Beckwith-Wiedemann, Ascher and Cobb (1,12). Change on pressure is a common finding with return to the original color on withdrawal of pressure (13). We believe that our cases correspond to vascular low-flow malformations due to their reddish-purple aspect, consistence, response to diascopy and absence of vascular pulsation (2).
Oral vascular lesions are of clinical importance to the dentist because they pose serious bleeding risk induced during normal procedures like orthodontics or oral surgery resulting in need of clinical treatment (14). Management of vascular lesions includes the injection of sclerosant substances, which is a safe and effective primary treatment (13). A study with Sudanese patients with esophageal varices demonstrated that MO was useful to reduce the bleeding consequent to portal hypertension (9). In one analysis done with 25 patients with craniofacial venous malformations, MO at 5% was applied inside the lesions and was effective for 14 of 16 patients who underwent sclerotherapy as the only treatment (11). Other report cited varicosities in the buccal mucosa treated with monoethanolamine oleate with resolution after three sessions (10). Even when the sclerotherapy with MO reduced the lesion only partially, it provided good preparation for further surgery of residual lesion (8). In our cases, the larger lesions were reduced and in one case, it could be removed surgically. In other case, preservation was indicated due to a diffuse residual lesion. In another study, 9 cases of pyogenic granuloma were treated by local injection of MO solution with excellent results. Scars were inconspicuous in all cases and complications occurred in only one patient who complained of pain due to an avoidable injection of excess solution. (7). In our cases, only slight edema and mild pain after the injections were referred in two cases. Other clinical trial confirmed the efficacy of MO application in lip hemangioma with complete resolution (13). The injection of MO should be slow and careful and the doses per application have been less than 2 mL with the minimum interval of 7 days between them (13). The usual concentration choice is 5 % been necessary to observe that reduced concentrations may be useful to control side effects like pain and inflammation (10, 13). In our cases we diluted to 2.5% in distilled water, and the patients did not complain about pain or discomfort after the injections and clinical result was satisfactory.
The mechanism of action of MO involves tissue necrosis, direct damage over the venous endothelium, induction of thrombus formation and balanced action over hemostasis (13,15). However, there are no studies which deal with histological alterations in oral vascular malformation caused by MO. In a study that analyzed the effect of MO at venous dog wall, it was observed that venous thrombosis with signs of organization. Reactive inflammatory process, sclerosant spillage and hyaline amorphous material deposition were shown in the adventitia layer (15). These data are according with our findings, corroborating the thrombosis induction inside the vessels, mild inflammatory infiltrate and hyalinization of adjacent connective tissue.
Conclusion
In summary, we presented six cases of low flow vascular lesions treated with 2.5% monoethanolamine oleate with good results, showing the histological confirmation of its efficacy and practically lack of severe clinical complications and complaints.
References
1. Romero AM, Echebarria A, Sierrasesumaga L. Vascular malformations as syndromic marker. An Sist Sanit Navar. 2004;27 Suppl 1:45-56. [ Links ]
2. Redondo P. Classification of vascular anomalies (tumours and malformations). Clinical characteristics and natural history. An Sist Sanit Navar. 2004;27 Suppl 1:9-25. [ Links ]
3. Werner JA, Dunne AA, Lippert BM, Folz BJ. Optimal treatment of vascular birthmarks. Am J Clin Dermatol. 2003;4(11):745-56. [ Links ]
4. Buckmiller LM. Update on hemangiomas and vascular malformations. Curr Opin Otolaryngol Head Neck Surg. 2004 Dec;12(6):476-87. [ Links ]
5. Winter H, Drager E, Sterry W. Sclerotherapy for treatment of hemangiomas. Dermatol Surg. 2000 Feb;26(2):105-8. [ Links ]
6. Seccia A, Salgarello M. Treatment of angiomas with sclerosing injection of hydroxypolyethoxydodecan. Angiology. 1991 Jan;42(1):23-9. [ Links ]
7. Matsumoto K, Nakanishi H, Seike T, Koizumi Y, Mihara K, Kubo Y. Treatment of pyogenic granuloma with a sclerosing agent. Dermatol Surg. 2001 Jun;27(6):521-3. [ Links ]
8. Matsumoto K, Nakanishi H, Koizumi Y, Seike T, Kanda I, Kubo Y. Sclerotherapy of hemangioma with late involution. Dermatol Surg. 2003 Jun;29(6):668-71; discussion 671. [ Links ]
9. Gasim B, Fedail SS, Musaad AM, Salih SM, Ibn-Ouf M. Endoscopic sclerotherapy for bleeding oesophageal varices: experience in Sudan. Trop Gastroenterol. 2002 Apr-Jun;23(2):107-9. [ Links ]
10. Gomes CC, Gomez RS, Do Carmo MA, Castro WH, Gala-Garcia A, Mesquita RA. Mucosal varicosities: case report treated with monoethanolamine oleate. Med Oral Patol Oral Cir Bucal. 2006 Jan 1;11(1):E44-6. [ Links ]
11. Choi YH, Han MH, O-Ki K, Cha SH, Chang KH. Craniofacial cavernous venous malformations: percutaneous sclerotherapy with use of ethanolamine oleate. J Vasc Interv Radiol. 2002 May;13(5):475-82. [ Links ]
12. Hanemann JA, Oliveira DT, Gomes MF, Dos Anjos MJ, Santana E. Congenital double lip associated to hemangiomas: report of a case. Med Oral. 2004 Mar-Apr;9(2):156-8, 155-6. [ Links ]
13. Ribas MO, Laranjeira J, Sousa MH. Hemangioma bucal: escleroterapia com oleato de etanolamina. Revisão da Literatura e apresentação de caso. Revista de Clínica e Pesquisa Odontológica 2004; 1:31-6. [ Links ]
14. Patel A, Davies SJ, Sandler PJ. The potentially fatal vascular anomaly and orthodontic treatment--a case report. Dent Update. 2004 May;31(4):230-2, 235-6. [ Links ]
15. Cruz Filho M, Maia CC, Abrahão S, Baptista Silva JCC, Gomes PO, Soufen MA, et al. Efeitos do oleato de etanolamina na parede venosa, de cães. Acta Cir Bras 2002;17:317-26. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Paulo Rogério Ferreti Bonan,
Av. Corinto Crisóstomo Freire, 600, apto 305,
Morada do Parque, Montes Claros,
Minas Gerais, Brazil, Cep: 39401-365,
E-mail: pbonan@yahoo.com
Received: 15-10-2006
Accepted: 1-10-2007