Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Pharmacy Practice (Granada)
versión On-line ISSN 1886-3655versión impresa ISSN 1885-642X
Pharmacy Pract (Granada) vol.5 no.1 Redondela ene./mar. 2007
| Original Research |
Medication prescribing errors in a public teaching hospital in India: A prospective study
Sayali POTE, Pramil TIWARI, Sanjay D'CRUZ.
| ABSTRACT Background: To prevent medication errors in prescribing, one needs to know their types and relative occurrence. Such errors are a great cause of concern as they have the potential to cause patient harm. The aim of this study was to determine the nature and types of medication prescribing errors in an Indian setting. Key words: Medication Errors. Drug Interactions. Pharmacists. India. | RESUMEN Antecedentes: Para prevenir errores de prescripción, se necesita conocer sus tipos y la aparición relativa. Esos errores causan gran preocupación porque son causa posible de daño al paciente. El objetivo de este estudio fue determinar la naturaleza y tipos de errores de prescripción de medicación en un centro de India. Palabras clave: Errores de medicación. Interacciones medicamentosas. Farmacéuticos. India. |
Sayali POTE. M.Pharm, Department of Pharmacy Practice. National Institute of Pharmaceutical Education and Research, S. A. S. Nagar, Punjab (India).
Pramil TIWARI. Associate Professor, Department of Pharmacy Practice. National Institute of Pharmaceutical Education and Research, S. A. S. Nagar, Punjab (India)
Sanjay D'CRUZ. Reader, Department of Medicine, Government Medical College and Hospital, Chandigarh (India).
INTRODUCTION
Pharmaceutical care is the responsible provision of drug therapy for the purpose of achieving definite outcomes that improve patients' quality of life. Any suboptimum therapy leads to medication error.1 The adverse drug event (ADEs) and medication errors are most common types of injuries experienced by hospitalized patients. Such events may be related to professional practice, healthcare products, procedures and systems.2
Various studies have been carried out to find out the impact of medication errors; but, the issue received maximum attention in the immediate years after the Institute of Medicine report 1999 was published.3 The published data demonstrates that approximately 5-10% of all hospital admissions are drug related.4
Various factors identified for medication errors are illegible orders, non-availability of patient information, inadequate medical knowledge, increased patient load, failure to monitor drug concentration or drug therapy, and not accounting for changes in renal & cardiac functions.5 The sources of medication errors, therefore, are multidisciplinary and multifactorial. Some medication errors result in serious patient morbidity and mortality.7 Medication errors usually occur because of breakdown in the systems that have been developed for handling and processing drugs, from prescribing and ordering to distribution and administration.6 Finally, the medication errors compromise the confidence of patients' in health care system and lead to increased health-care cost.
A number of published reports have confirmed the adverse impact of these errors on patients' health and health care.8-10 Therefore, the medication errors should be minimized as far as possible and the nature should be identified so that effective systems can be implemented for prescribing, transcribing, dispensing and administering the medications. The aim of this study was to determine the nature and the types of medication errors in prescribing in an Indian setting.
METHODS
The medication errors were analyzed through a prospective observational study conducted in 3 medical wards of the public Teaching Hospital in India. The prescriptions were analyzed using the chart review method, which is well suited to identify the prescribing medication errors.11 The patients were randomly selected and the data for identification, medication details and relevant laboratory reports and progress reports were collected. The prescriptions with incomplete information for date of discharge, identification number were excluded from the study. The patient (or caregiver) was interviewed to gather information regarding the drug allergy and past medications taken. The drugs given on SOS basis were also taken into consideration. The patients were followed throughout the hospital stay to study the clinical significance of these medication errors and drug-drug interactions.
Each prescription was checked twice, once for identifying any medication error(s) and then for the possibility of a drug-drug interaction in the prescription. All the prescriptions were checked for errors by the Micromedex Drug-Reax database.12 The prescriptions were checked for incorrect dosing interval, dosing errors, incomplete prescription, incorrect drug, allergy, inappropriate duration of therapy or the route of administration, monitoring error and drug-drug interactions.
All the data was represented as average (SEM) and percentages. Appropriate statistical tests were used.
RESULTS
These results are based upon data collected from 304 patients (Of 312, 8 were excluded). Out of 304 patients, 204 (67%) were male patients. The age profile showed that only 25 patients were below the age of 18 years; 198 patients (65.2%) were between 18-60 years and 81 patients were over 60 years of age.
A total of 2052 medications were prescribed to 304 patients; and, the average number of medications per patient was found to be 6.57 (0.18). The analysis of these averages vis-à-vis age groups showed an extremely significant statistical difference between the groups 18-60 years vs. over 60 years. The average number of medicines for these groups were 6.20 (0.21) and 8.20(0.39), respectively.
The number of patients with a single diagnosis was 133; 95 presented two diagnoses and 76 patients had more than 2 diagnoses. Therefore, the average diagnosis per patient was 1.88 (0.06).
Of the 304 cases, approximately 34% cases had at least one medication error. The total number of errors identified was found to be 157. The medication errors were classified according to the types of errors, their severity and the medication class(es) involved. Out of the 157 errors observed, the drug-drug interactions (DDIs) were noted in 68.2% of the patients making it the top most medication error. This was followed by incorrect dosing interval in 12.1% cases, overdosing in 7%, incomplete prescription in 5%, underdosing and monitoring error in 2.6%, incorrect medication and allergy occurred in 1.3% of cases. The detailed distribution of the medication errors is shown in table 1.
Of the total 157 errors identified, only 40 were severe, 97 were moderate and the remaining 20 were minor. Hence, the largest contributor (61.8%) was the moderate errors.
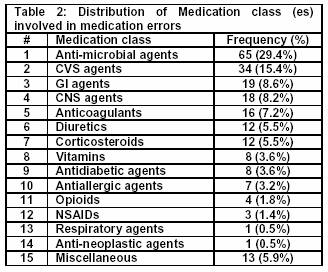
The study of involvement of a particular medication class to the medication errors showed that the anti-microbial agents contributing maximum (29.4%), which was followed by cardiovascular agents (contributing 15.4%). In the third rank were the GI agents (contributed 8.6%) followed very closely by the CNS agents contributing 8.2% (Table 2). It is evident that the total number of times a medication class was involved in the errors (221) was higher than the total number of errors identified (157). This implies that in one error, two or more medications might be involved - belonging to either the same or different class.
The analysis of medication errors in each age group demonstrated that the prescriptions of patients over 60 years of age had the largest proportion (69.1%) of medication errors. It is very clear from the table 3 that as the age increases, the number of medication errors also increase; very likely because of co morbidities and a higher number of medicines being used. The linear correlation coefficient was computed in number of medications prescribed and percentage of errors in the same class. The value of correlation coefficient was 0.84, which confirms that polypharmacy increases the incidence of medication errors.
DISCUSSION
A total of 304 cases have been analyzed. Out of these 304 patients 32.9% were females and 67.1% were males. The patients of all ages have been included in the study. Nearly two-thirds of the patients were adults.
A number of researchers have shown that the DDIs and dosing errors occur more often in healthcare settings; the current results match this pattern of errors.13-17 In this study, the drug-drug interactions were found to account for over two-third (68.2%) of the total errors, which was followed by incorrect dosing interval & overdosing. The most common drug involved in DDIs was Aspirin (18 occurrences), which interacts with heparin, low molecular weight heparin, clopidogrel and streptokinase prescribed to the patients of this study. This was followed by amikacin (9 occurrences) which had the potential to interact with ceftriaxone, frusemide, cloxacillin, ceftazidime and vancomycin prescribed; insulin (7 occurrences) with metoprolol, atenolol, carvedilol and levofloxacin.
Inappropriate dosing frequency was the second largest type of medication error noted; the drugs involved most often were pantoprazole and ranitidine. Overdosing was found to be higher amongst anti-microbial agents and cardiovascular agents. In addition to these three types of medication errors, underdosing, allergy, inappropriate choice of drug and incomplete prescription were also found to contribute to the errors. Allergy with cefuroxime & phenytoin has occurred in one patient each. Many prescriptions did not contain information such as diagnosis or weight of patient (in renal failure), though these were not counted as errors. However, the prescriptions in which dose or frequency or route of administration was not stated were counted as errors. They contributed 5% of the total medication errors. For example, the dose of vitamin K and some antimicrobial agents' was not specifically mentioned in the prescriptions. The analysis of medication errors based upon severity shows that the moderate medication errors were most frequent, which was followed by the severe ones.
The studies analyzing the risk factors for the medication errors have shown that the age and number of medications administered were the main risk factors for medication errors.17 The results of this study are in concurrence with this.
CONCLUSION
This study had presented a pattern of findings of medication prescribing errors in a public teaching hospital in India. The present results point to the establishment of a medication error reporting system at each hospital and to share the data with other hospitals/healthcare settings. The role of a clinical pharmacist in this situation appears to be a strong intervention; and, the clinical pharmacist, initially, could only confine to identification of the medication errors.
| References |
1. Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm 1990;47:533-43. [ Links ]
2. Phillips J, Beam S, Brinker A, Holquist C, Honig P, Laureen YL, Pamer C. Retrospective analysis of mortalities associated with medication errors. Am J Health Syst Pharm 2001;58:1835-40. [ Links ]
3. Kohn LT, Corrigan GM, Donaldson MS. To err is human: building a safer health system. Institute of medicine. Washington DC: National Academy Press;1999. [ Links ]
4. Zed PJ. Drug-related visits to the emergency department. J Pharm Pract 2005;18(5):329-35. [ Links ]
5. American society of hospital pharmacists. ASHP guidelines for preventing medication errors in hospitals. Am J Hosp Pharm 1993;50:305-14. [ Links ]
6. National Coordinating Council for Medication Error Reporting and Prevention. About medication Errors [Homepage on the internet]. [Updated on 2001; cited on 7th April 2006]. Available from: http//www.nccmerp.org/aboutMedErrors.html [ Links ]
7. Benjamin CG, Jeffrey MR, Robert G, David WB. What do we know about medication errors in inpatient psychiatry? Psychiatr serv 2003;29(8):391-400. [ Links ]
8. Lapointe NM, Jollis JG. Medication Errors in hospitalized cardiovascular patients. Arch Intern Med 2003;163:1461-6. [ Links ]
9. Jenkison ML. Prescribing errors. Lancet 2002;360:256-9. [ Links ]
10. Hennessy S, Bilkar WB, Zhou L, Weber AL, Bresinger C, Wang Y, Strom BL. Retrospective drug utilization review, medication errors, and clinical outcomes. JAMA 2003;290:1494-9. [ Links ]
11. Flynn EA, Barker KN, Pepper GA, Bates DW, Mikel RL. Comparison of methods for detecting medication errors in 36 hospitals and skilled nursing facilities. Am J Health Syst Pharm 2002;59:436-69. [ Links ]
12. DRUG-REAX (Micromedex), version 2005: Thomson MICROMEDEX; Greenwood Village, Colorado, USA. [ Links ]
13. Runciman WB, Roughhead EE, Semple SJ, Adams RJ. Adverse drug events and medication errors in Australia. Int J Qual Health Care 2003;1(15 suppl):149-59. [ Links ]
14. Patel NC, Crismon ML, Rush AJ, Francea A. Practitioners versus medication-expert opinion on psychiatric pharmacotherapy of mentally retarded patients with mental disorders. Am J Health Syst Pharm 2001;58:1824-9. [ Links ]
15. Carter BL, Lund BC, Hayase N, Chrischilles E. The extent of potential antihypertensive drug interactions in Medicaid population. Am J Hypertens 2002;15:953-7. [ Links ]
16. Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ 2005;173(5):510-15. [ Links ]
17. Evans RS, Lloyd JF, Nebeker JR, Samore MH. Risk factors for adverse drug events: A 10-year analysis. Ann Pharmacother 2005 Jul-Aug;39(7-8):1161-8. [ Links ]