Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Pharmacy Practice (Granada)
versión On-line ISSN 1886-3655versión impresa ISSN 1885-642X
Pharmacy Pract (Granada) vol.5 no.3 Redondela jul./sep. 2007
| Original Research |
Assessment of prescription profile of pregnant women visiting antenatal clinics
Uchenna I. EZE, Adego E. EFERAKEYA, Azuka C. OPARAH, Ehijie F. ENATO.
| ABSTRACT Managing medical complications in pregnancy is a challenge to clinicians. Key words: Teratogens. Pregnancy. Maternal Exposure. Nigeria. | RESUMEN Manejar las complicaciones médicas en el embarazo es un reto para los clínicos. Palabras clave: Teratógenos. Embarazo. Exposición Materna. Nigeria. |
Uchenna I. EZE. MPharm., Lecturer. Department of Clinical Pharmacy/Biopharmacy, Faculty of Pharmacy, Olabisi Onabanjo University Shagamu Campus, Shagamu (Nigeria).
Adego E. EFERAKEYA, MD, PhD. Professor, Department of Pharmacology &Toxicology, Faculty of Pharmacy, University of Benin, Benin City (Nigeria).
Azuka C. OPARAH. MPH, PhD. Lecturer, Department of Clinical Pharmacy & Pharmacy Practice, Faculty of Pharmacy, University of Benin, Benin City (Nigeria).
Ehijie F. ENATO. PhD, Lecturer. Department of Clinical Pharmacy & Pharmacy Practice, Faculty of Pharmacy, University of Benin, Benin City (Nigeria).
INTRODUCTION
Pregnancy is a time of profound physiological changes in a woman's body. These unique changes challenge clinicians managing disease states during pregnancy in the selection of medications best suited to treat their patients.1 Maternal drug use during pregnancy may pose a teratogenic risk to the foetus. However, the recommendation to avoid all drugs during early pregnancy is unrealistic and may be dangerous.2,3 Pregnancy should not deter clinicians from providing their patients with appropriate management of their medical conditions, hence, prescribing in pregnancy is an unusual risk benefit situation.4,5
In 1979, the United States Food and Drug Administration (FDA) introduced a system of rating pregnancy-risk associated with pharmacological agents. This system categorised all drugs approved after 1983 into one of five pregnancy risk categories (A, B, C, D, and X). It indicates the effect of the agent on the foetus based on available animal and human data and recommends the degree of precaution that should be undertaken with each drug. However, the risk factors assigned are sometimes difficult to interpret because they may not always reflect the latest findings.6
Information on the use of drugs during pregnancy is scarce and rather anecdoctal.7 Despite the absence of adequate studies on the safety and effectiveness of prescription drugs for pregnant women, evidence available shows that physicians prescribe, and pregnant women take a surprisingly large number of drugs. An international investigation sponsored by WHO showed that pregnant women ingest an average of three prescription medications during pregnancy (range 1 – 15). Furthermore, 86% of the women had taken at least one prescription medication during their pregnancies.8
There have been drug use studies in Nigeria. Odusanya et al.9 did a retrospective prescribing audit at primary health care facilities and reported an average of 7.27 and 4.99 number of medicines in Mushin and Ikeja Lagos Nigeria, respectively. Gharoro and Igbafe10 showed that out of the 1200 pregnant women in their study, self-medication occurred in 26.8%. Folic acid was used by 76.08% of the women, antimalarials 19.45%, however studies on prescribing in pregnancy are quite few in Nigeria hence this study was done to add to the baseline of research of this sort. The objectives of this investigation were to determine the disease pattern and assess the prescription profile for pregnant women in Benin City, Nigeria. This study also assessed the types and extent of prescribing of medicines according to risk to the foetus.
METHODS
A retrospective prescription survey was conducted among 1,200 outpatient pregnant women attending three antenatal clinics (ANCs) in Benin City, Nigeria. The investigation was performed within February to October 2000. One of the facilities was a 560-bed university teaching hospital. The other two were secondary health care facilities having 500 and 120 beds, respectively. Prescribed medicines in the hospitals are dispensed in the hospital pharmacies when available; otherwise patients are referred to the communities for refills.
Permission was sought from the authorities of the hospitals before commencement of the study. Medical case files of the pregnant women were retrieved and reviewed, and relevant information documented in a specific data collection format designed for the study. Data were gathered on age, gravidity, medical conditions, and medicines prescribed.
A World Health Organisation's (WHO) recommended method11 was used to measure some specific factors in prescribing for these women.
This method has been adopted in other studies.8,12 The average number of medicines per encounter was calculated by dividing the total number of drugs by the number of encounters. Percentage encounter with generic name, percentage encounter with antibiotics, and percentage of encounter with injections were determined by dividing the number of occurrence by the total number of event, respectively, and multiplying by 100. Data on the United States Food and Drug Administration classification of medicines according to risk to the foetus were obtained based on information provided in the physician's drug handbook.13
RESULTS
Four hundred medical case files were audited in each hospital giving a total of 1200 medical case files for the entire study. Demographics obtained showed that the average age was 25.16 (SD=3.62). Of the ANCs attendees were primigravidae 426 (35.5%), secundigravidae 260 (21.7%), and multigravidae 500 (41.6%), while in 14 cases (1.1%) the gravidity was not indicated.
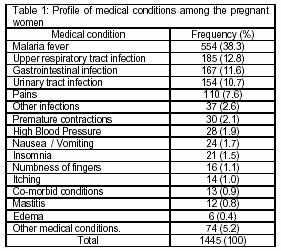
Table 1 shows the pattern of medical conditions occurring among the women in the 3 health facilities. Malaria fever occurred most frequently followed by upper respiratory tract infections and gastrointestinal disturbances.
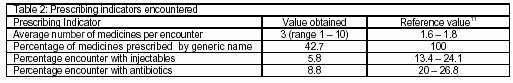
A total of 1897 prescriptions were obtained from the 1200 medical case files. The average number of drugs per encounter was found to be 3.0 (range 1 – 10). Eighty-two different medicines were encountered and a total of 5708 medicines were prescribed for the entire period. Table 2 shows the WHO prescribing indicators that were evaluated.
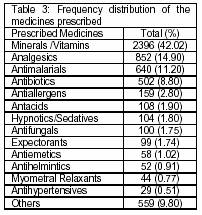
The distribution of medicines prescribed to these pregnant women is as shown in Table 3. Minerals and vitamins were the most frequently prescribed medicines. Folic acid 671 (35.4%) was the most frequently prescribed drug in the three health facilities. Other minerals and vitamins prescribed included ferrous sulphate 645 (34%), vitamin C 152 (8.0%) and calcium lactate 19 (1.0%). Paracetamol 749 (87.9%) was the most frequently prescribed analgesic; other analgesics included methamizole 66 (7.8%), acetylsalicylic acid 27 (3.2%), piroxicam 4 (0.5%), pentazocin 2 (0.3%), dihydrocodeine 2 (0.3%), and ibuprofen 2 (0.3%).
Antimalarials were the third most occurring medicines with an average of 640 (11.2%) for the three health facilities when compared with other groups of medicines. Chloroquine 350 (54.7%) was the most frequently prescribed antimalarial drugs for the 3 health facilities. Other antimalarials written included sulphadoxine/pyrimethamine130 (20.3%), pyrimethamine 64 (10%), quinine 76 (11.9%), amodiaquine 48 (7.5%), proguanil 4 (0.6%), sulphamethopyrazine/pyrimethamine 2 (0.3%). Twenty different types of antibiotics were encountered in the study. Penicillins 279 (55.6%) were the most frequently used antibiotics for the antenatal clinics. Other antibacterial agents included metronidazole 59 (11.8%), macrolides 53 (10.6%), cotrimoxazole 37 (7.4%), phythalylsulphathiazole 27 (5.4%) 4-quinolones 12 (2.4%), nitrofurantion 12 (2.4%), aminoglycosides (9(1.8%), and tetracycline 1 (0.2%).
Other groups of medicines encountered included antihypertensives: methyldopa, 24 (82.8% of all antihypertensives prescribed), nifedipine 4 (13.8%) and hydrallazine 1 (3.5%), Hypnotics and sedatives encountered included diazepam 87 (83.7%), bromazepam 12 (11.5%), nitrazepam 5 (4.8%), antifungals (clotrimazole containing agents 65 (65%), tioconazole containing agents 24 (24%), nystatin containing agents 8 (8%) miconazole containing agents 3 (3%). Salbutamol 44 (0.77%) was also prescribed.
Majority of the medicines encountered were given orally 5268 (92.3%), others were by injectable route 336 (5.9%), per vaginal 99 (1.7%), instilling into the ears 2 (0.04%), eyes 1 (0.02%), anally 2(0.04%).
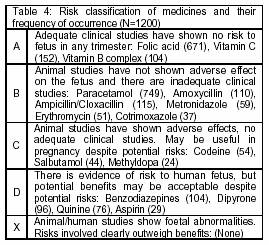
A classification of medicines according to risk to the foetus indicated that of all the medicines prescribed, 2743 (48.1%) were in category A, 1465 (25.7%) category B, 984 (17.2%) category C and 286 (5.0%) in category D. Table 4 shows drugs and their frequency of occurrence in this study.
DISCUSSION
The average maternal age obtained in this study was similar to that obtained in a similar study in Nepal.7 Primigravid women formed the majority of women attending the antenatal clinics. The pattern of medical conditions obtained in this study varied with those reported in Nepal study7 where problem oriented drug use was mainly due to gastrointestinal tract problems (nausea and vomiting, dyspepsia), and vaginal spotting/ bleeding.
Malaria fever was the most prevalent medical condition occurring among the pregnant women in the antenatal clinics of the three health facilities. Malaria in pregnancy is a major public health problem in Nigeria, as well as other malaria endemic countries.14 Previous reports indicated that pregnant women attending ANCs perceived malaria as a common health problem.15,16 Malaria in pregnancy results in maternal anemia, intrauterine growth retardation, fetal low birth weight and neonatal mortality.14
The average number of drugs prescribed per encounter in the antenatal clinics differs from the standard set by WHO.11 However, similar values have been obtained in studies by Das et al.7 and Krause et al.17 The maximum number of drugs prescribed was 10. The high number may have resulted from prescribing routine drugs along with other medicines. The implication is that the patient may have more medicines than she can cope with in terms of cost and adherence. The high number may also increase the risk of adverse drug interactions. The total number of medicines obtained was more than that obtained by Gracia et al.18 but less than that obtained by Mengue et al.19 Most of the medicines were prescribed in brand names irrespective of the type, and this pattern is common in the country. The low value obtained on generic prescribing indicates that irrational prescribing occurred.
However value obtained by Das et al.7 was even lower. This means that prescribers here were not complying fully with WHO recommendation that drugs should be prescribed using their international nonproprietary names. The use of brand names may lead to increased cost of drugs for these women. Factors that may be responsible for this trend include the influence of drug promotional activities, pressures of pharmaceutical detail men, lack of continuing education on the principles of rational prescribing and non-familiarity with generic names among the prescribers.
The occurrence of injectables was low in this study, which is commendable since the use of injectables may introduce a high concentration of drug to the plasma, which could lead to toxicity in the pregnant women exposed. The percentage encounter of antibiotics was lower than that prescribed by WHO and this is encouraging.
The level of antimalarial prescription was low compared to the fact that malaria is endemic in this area. Such low level was also obtained in a previous study.10 This may have implication on the effectiveness malarial intervention chemoprophylaxis programme.10 Prevention and treatment of malaria are essential components of antenatal care in endemic areas, but requires special considerations during pregnancy.14 Inadequate consumption of antimalarial drugs by patients may be a major contributing factor to the diminishing efficacy of the commonly available antimalarial drugs and development of drug resistant strains of the P. falciparum malarial parasites in our community.14
The occurrence of contraindicated medicines was low. Proper prescribing demands that such contraindications do not occur but the use of such medicines may be considered in cases where benefits outweigh the risk.20 Majority of the drugs prescribed were in category A of the FDA's classification of medicines according to risk to the foetus, followed by those in category B. However drugs in C and D were also obtained. This may have been in cases where benefits outweigh the risk. Similar results have been obtained in another study.19
CONCLUSION
Malaria fever occurred most frequently followed by upper respiratory tract infections and gastrointestinal disturbances among the pregnant women. Minerals, vitamins and to a less extent antimalarials topped the list of the prescribed medicines. The average number of prescriptions per encounter was much higher than WHO standard, indicating occurrence of polypharmacy. The occurrence of contraindicated medicines was desirably low.
ACKNOWLEDGEMENT
The authors of this study would like to acknowledge Holly Hoffman-Roberts, Pharm.D. and Brian K. Irons, Pharm.D.,
CONFLICT OF INTEREST
None declared.
| References |
1. Cheney BE. Management of common primary care problems during pregnancy. Program and abstracts of the 5th Annual Conference of the National Association of Nurses Practitioners in women's health. September 27-29, 2002 Scottsdale Arizona. [ Links ]
2. Vallance P. Drugs and the foetus. BMJ 1996;312:1053-4. [ Links ]
3. Banhidy F, Lowry BR, Czeizel AE. Risk and benefit of drug use during pregnancy. Int J Med Sci. 2005;2(3):100-6. [ Links ]
4. Webster WS, Freeman JA. Prescription drugs and pregnancy. Expert Opin Pharmacother 2003; 4(6): 949-61. [ Links ]
5. Revan VB, Sun ET, Morris MC. Management of asthma in pregnancy. Female Patient 2002:27;18-28. [ Links ]
6. Young VSL.Teratogenicity and Drugs in the breast milk. In: Koda kimble, MA. et al. eds. Applied Therapeutics: The Clinical Use of Drugs 7th edition USA Lippincott Williams & Wilkins; 2001. [ Links ]
7. Das B, Sarkar C, Datta A, Bohra S. A study of drug use during pregnancy in a Teaching Hospital in Western Nepal. Pharmacoepidemiol Drug Saf 2003; 12(3):221-5. [ Links ]
8. Collabourative Group on Drug Use in Pregnancy. An international survey on drug utilization. Int J Risk Safety Med 1991; 1:1. [ Links ]
9. Odusanya OO, Oyediran MA. Rational drug use at primary health care centers in Lagos, Nigeria. Nig Qt J Hosp Med 2000;10:4-7. [ Links ]
10. Gharoro EP, Igbafe AA. Pattern of drug use amongst antenatal patients in Benin City, Nigeria. Med Sci Monit, 2000; 6 (1);84-87. [ Links ]
11. How to investigate drug use in health facilities: selected drug use indicators. Action Programme on Essential Drugs. (WHO/DAP/(93.1) Geneva, World Health Organization, 1985. [ Links ]
12. Carmo TA, Nitrini SM. Prescricoes de medicamentos para gestantes: um estudo farmacoepidemiologico. Cad Saude Publica 2004;20(4):1004-13. [ Links ]
13. Kelly WJ. Physician's drug hand book 10th edition, Philadelphia: Lippincott Williams & Wilkins; 2003. [ Links ]
14. World Health Organization (WHO/AFRO). A strategic framework for malaria prevention and control during pregnancy in the African region. World Health Organization Regional Office for Africa, Brazzaville – AFR/MAL/04.01; 2004. [ Links ]
15. Enato EF, Okhamafe AO, Okpere EE. A survey of knowledge, attitude and practice of malaria management among pregnant women from two health care facilities in Nigeria. Acta Obstet Gynecol Scand. 2007;86:33-6. [ Links ]
16. Enato EF, Okhamafe AO, Okpere EE, Oseji FI. Prevalence of malaria during pregnancy and antimalarial intervention in an urban secondary health care facility in Southern Nigeria. Med Prin Pract 2007;16:240-3. [ Links ]
17. Krause G, Borchert M, Benzler J, Heinmuller R, Kaba I, Savadogo M, Siho N, Diesfeld HJ. Research report. Rationality of drug prescriptions in rural health centers in Burkina Faso. Health Policy Plan 1999;14:291-8. [ Links ]
18. Gracia I, Beyens MN, Gauchoux R, Guy C, Ollagnier M. Drug Prescription for pregnant women in the Department of the Loire. Therapie. 2000; 55(5):605-11. [ Links ]
19. Mengue SS, Schenkel EP, Duncan BB, Schmidt MI. Uso de medicamentos por gestantes em seis cidades brasileiras. Rev Saude Publica 2001; 35(5) :415-20. [ Links ]
20. Beyens MN, Guy C, Ratrema M, Ollagnier M. Prescription of drugs to pregnant women in France. The HIMAGE study. Therapie 2003; 558(6): 505-11. [ Links ]