Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Pharmacy Practice (Granada)
versión On-line ISSN 1886-3655versión impresa ISSN 1885-642X
Pharmacy Pract (Granada) vol.9 no.4 Redondela oct./dic. 2011
ORIGINAL RESEARCH
Prescription of psychoactive drugs in patients attended by the SUS at Manhuaçu - MG (Brazil)
Prescripción de medicamentos psicoactivos en pacientes atendidos por el SUS en Manhuaçu - MG (Brasil)
Gonçalves D.P.1, Silva I.V.2, Rangel L.B.3, Rezende L.C.4
1. PharmD, Department of Pharmacy, Municipal Secretary of Health. Manhuaçu, MG (Brazil).
2. PharmD. PhD. Assistant Professor. Biotechnology Post-Graduation Program, Department of Morphology, Federal University of Espírito Santo. Vitória, ES (Brazil).
3. PharmD. PhD. Associate Professor. Biotechnology Post-Graduation Program, Department of Pharmaceutical Sciences, Federal University of Espírito Santo. Vitória, ES (Brazil).
4. PharmD. Biotechnology Post-Graduation Program, Federal University of Espírito Santo. Vitória, ES (Brazil).
Funding: CNPq - Universal no019/2004, Universal no02/2006, and Ação Transversal no07/2010. DECIT/SUS/CNPq - PPSUS/2005 and PPSUS/2007. FAPES - Universal/2005 and Student scholarship announcement no001/2009. FACITEC/ES - Universal/2007.
ABSTRACT
Objectives: In this study we present the development of a database of psychoactive drugs dispensed to patients attended by the Brazilian Public Health System (SUS) in the city of Manhuaçu, Minas Gerais and the pattern of drug prescription in this city.
Methods: 827 patients under psychoactive treatment and attended by SUS were surveyed and information such as gender, degree of education, age, marital status were collected. The collected data were analyzed in order to outline patients' profile and the dispensing and information was used to the access the pattern of psychoactive drug use in the city.
Results: Women accounted for 67.2% of the population and age seemed to influence positively the use of psychoactive drugs. Benzodiazepines and antidepressants were among the most prescribed drugs especially after 20 years of age, while in the younger population the antipsychotics and antiepileptics were the mainly prescribed drugs. Antiepileptics/mood stabilizers seemed to be prescribed mainly to single men and women.
Conclusion: Personal data concerning gender, age and marital status are related with psychoactive drug dispensing. The collected data will serve as a support for the performance of pharmacists responsible for dispensing psychoactive drugs in the municipality.
Key words: Psychotropic Drugs. Drug Utilization. Age Factors. Brazil.
RESUMEN
Objetivos: En este estudio presentamos el desarrollo de una base de datos de medicamentos psicoactivos dispensados a pacientes atendidos por el Sistema Público de Salud brasileño (SUS) en la ciudad de Manhuaçu, Minas Gerais y el patrón de prescripción en esta ciudad.
Métodos: Se investigó a 827 pacientes bajo tratamiento con psicoactivos y atendidos por el SUS y se recogió información como género, nivel de educación, edad, estado civil. Los datos recogidos se analizaron para dibujar el perfil de los pacientes y la dispensación y la información se utilizó para crear el patrón de uso de psicoactivos en la ciudad.
Resultados: Las mujeres sumaron el 67,2% de la población y la edad parecía influenciar positivamente el uso de medicamentos psicoactivos. Las benzodiazepinas y los antidepresivos estaban entre los medicamentos más prescritos, especialmente después de los 20 años, mientras que en la población más joven los antipsicóticos y los antiepilépticos fueron los medicamentos más prescritos. Los antiepilépticos y los estabilizadores del ánimo parecían ser prescritos principalmente a hombres y mujeres solteros.
Conclusión: Los datos personales como género, edad y estado civil están relacionados con la dispensación de medicamentos psicoactivos. Los datos recogidos servirán como apoyo para la actuación de los farmacéuticos responsables de la dispensación de psicoactivos en el municipio.
Palabras clave: Psicotrópicos. Utilización de Medicamentos. Factores de Edad. Brasil.
Introduction
Drugs that act on the central nervous system, designated as psychoactive drugs, are among the earliest pharmacological compounds developed and still among the most widely used worldwide. Moreover, the use of psychoactive drugs has increased in recent decades in many western countries1,2, and even, in some Asiatic countries.3,4 This tendency has been attributed to the increased frequency of psychiatric disorders within the population, the introduction of new psychoactive drugs in the pharmaceutical market, and the novel therapeutic indications of old psychoactive drugs.
According to Sinitox (Toxicological and Pharmaceutical National Information System, Brazil), there have been over 112 thousand poisonings registered in Brazil in the year of 2007, of which 30.31% were caused by medications, the main cause of intoxications.5 Poisoning by psychoactive drugs is especially worrisome, since it can often result in patient's death, accidentally or intentionally.
In this context, the pharmacist-patient relationship is crucial, and pharmacists must act in the documentation of medication history.6 Pharmaceutical care has the objectives to focus on the patient during the therapeutic intervention, and to promote the rational use of drugs. For that matter, the pharmacist might evaluate the use of drugs and the patients' profile, generating databases that would ultimately enable the guidance and the dissemination of information about drugs, as well as the promotion of continuing education of health professionals, patients and the community.
Many studies concerning psychoactive drugs prescription and dispensation are available in the literature, and this article contributes to this subject by showing the patterns observed in the city of Manhuaçu, Minas Gerais, Brazil. The central focus of the present work was to generate a database based on information provided by patients using psychoactive drugs, attended by the Brazilian Public Health System (SUS) in the city of Manhuaçu, Minas Gerais, Brazil, and to correlate the collected data with the profile of psychoactive drugs use.
Methods
AIn the period of one month, from April to May 2009, 827 patients under psychoactive treatment and attended by SUS were surveyed in the city of Manhuaçu, Minas Gerais, Brazil. The interviews were conducted in a single location during drug dispensation by the pharmacist. Only drugs listed by the Brazilian Standardized Municipal Essential Medicines (REMUME) were provided to the patients included in this study. The instrument used in the interview was a questionnaire with five questions regarding patients' information, such as gender, degree of education, age, marital status, and psychoactive drugs dispensed. This questionnaire was presented and approved by the Municipal Secretary of Health of Manhuaçu. An original database was generated with the information provided by the patients. The five variables included in the model studied were then coded, based on preliminary analysis: a) gender (male, female), b) age (0-10 years, 11-20 years, 21-30 years, 31-40 years, 41-50 years, more than 50 years), c) education degree (illiterate, primary school, high school, incomplete high school education, graduation degree), d) marital status (single, married, divorced, widowed), e) used psychoactive drug.
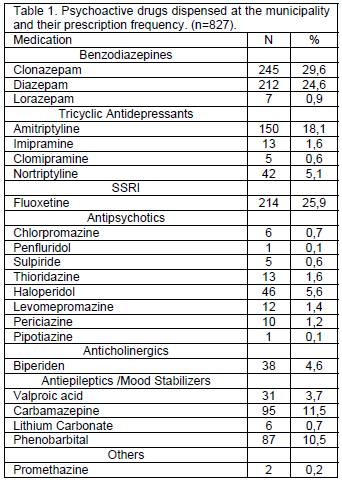
The psychoactive drugs were divided in 7 different classes regarding their clinical use, mechanism of action, chemical class, and the Anatomical Therapeutic Chemical (ATC) classification system, as: Benzodiazepines derivatives (which we will refer to only as "Benzodiazepines"), Antidepressants Non-selective monoamine reuptake inhibitors (which we will refer to as Tricyclic antidepressants due to their structural similarity), Antidepressants selective serotonin reuptake inhibitors (which we will refer to only as the abbreviation SSRIs), Antipsychotics, Anticholinergics, Antiepileptics (which we will refer to as antiepileptics and mood stabilizers, once the latter is a common clinical application for the drugs in this class) and others (Table 1). Data concerning drug dispensation were expressed as absolute number and frequency of dispensation (percentage of people to whom a specific drug has been prescribed). To analyze the trend of increase or decrease in drug prescription varying with patients' ages the chi-square test for trend was applied. The association of discrete variables (gender, marital status and education) with the dispensation of psychoactive drugs was performed only within the adult population (above 20 years) and was estimated by the chi-square test. The occurrence of polypharmacy (ie, the use of multiple medications) and the main drug associations were measured by counting and were expressed as absolute values and ratios for each age group. The statistical analyses were performed using the GraphPad Prism 5.0.
Results
The present study was based on the 21 psychoactive drugs provided by SUS database generated in Manhuaçu, Minas Gerais, Brazil. The drugs, their pharmacological classification and the frequency of each one dispensation are shown in Table 1. Initially, tabulations were carried out to estimate the patterns of psychoactive drug use according to gender, age, marital status and education. The studied population (n=827) was constituted 271 men (32.8%) and 556 women (67.2%). The most frequently prescribed drug was clonazepam, which was used by 29.51% of the patients, followed by fluoxetine (25.78%), diazepam (24.54%), amitriptyline (18.07%) and carbamazepine (11.45%).
Data analysis showed higher rates of drugs dispensation to patients older than 50 years (34.2%), followed by the age group ranging from 41 to 50 years (24.6%), 31 to 40 years (20%), 21 to 30 years (12.4%), 11 to 20 years (4.8%) and 0 to 10 years (4.0%). It was observed that in younger patients (age groups between 0 and 10 and between 11 and 20) the class of drugs most commonly prescribed was the antiepileptics and mood stabilizers, especially carbamazepine (Table 2). Patients with more than 21 years old showed an increase in the prescription of benzodiazepines, tricyclic antidepressants and selective serotonin reuptake inhibitors, especially clonazepam, diazepam, amitriptyline and fluoxetine. The use of chi-square test for trend showed a statistically significant trend of increasing in the prescription of benzodiazepines, tricyclic antidepressants and selective serotonin reuptake inhibitors and also a decreasing in the prescription of antiepileptics and antipsychotics with increasing age (Table 2).
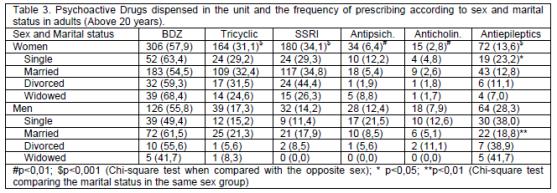
We also analyzed the profile of drugs prescription according to patients' sex and marital status within our adult (older than 20 years) sample (n=756). It was observed that the use of tricyclic antidepressants and SSRIs was more frequent in women when compared to men (chi-square p<0.001 for both drug groups). 31.1% of adult women were in use of tricyclic antidepressants, and 34.1% were in use of SSRIs. On the other hand, only 17.3% of men were using tricyclic antidepressants, and 14.2% were taking SSRIs. The trend is the exact opposite when the use of antipsychotics, anticholinergics, and antiepileptics/mood stabilizers drugs were analyzed. In this context, the referred drug classes were more frequently prescribed for men (chi-square, p <0.01, p <0.01, and p <0.001, respectively). The percentage of men using antipsychotics, anticholinergics, and antiepileptics/mood stabilizers drugs was 12.4%, 7.9%, and 28.3%, respectively. Nonetheless, 6.4% of women were taking antipsychotics drugs, 2.8% were in use of anticholinergics drugs, and 13.6% were using antiepileptics/mood stabilizers (Table 3). The marital status appeared to influence the use of the studied drugs. To perform such an analysis, chi-square test was carried out. However, the overall analysis had not shown statistical significance (chi-square p>0.05) (Table 3). The class of antiepileptics/mood stabilizers drugs was the only one to have its use associated to the patients' marital status, both in men and women. It was observed that 23.2% of single women were under treatment with this class of drugs, whereas when widows, divorced and married women were considered this value had not exceed 13% (chi-square p<0.05). For men, it has been observed that marriage was related with less antiepileptics and/or mood stabilizers prescription as only 18.8% of married men used this kind of drugs, while for other civil statuses this value was always above 38% (chi-square p<0.01) (Table 3).
Drug combination was also studied. The average number of medications used per patient was 1.52. The vast majority of patients (62.4%) were in use of only one product, and just around 10% used more than 2 drugs combined (Table 4). The most commonly observed combination of two drugs in patients younger than 20 years of age was that of carbamazepine with an antipsychotic or an antiepileptic. More specifically, the association of periciazine and carbamazepine was highly prescribed for children under 10 years old while association of valproic acid and carbamazepine was the most frequent in patients between 11 and 20 years old. For patients older than 20 years, the association of antidepressants (both tricyclic or SRRIs) with a benzodiazepine was the most commonly observed psychoactive association (Table 5).
We also collected educational data from each of the patients enrolled in this study. The adult population was divided into 5 groups of schooling with the following percentages: Illiterate (29.4%), Primary school (56.2%), High school (10.7%), Incomplete Graduate Education (2.5%) University Degree (1.1%). No influence of schooling in drug dispensation has been detected (chi-square p>0,05).
Discussion
The present study aimed to determine the profile of the psychoactive drugs dispensation by SUS in the Brazilian city of Manhuaçu, Minas Gerais state, through the development of a database containing confidential information of patients with psychiatric and/or neurological disorders. The ultimate benefit herein intended is to technically overcome a foremost Public Health issue concerning pharmaceutical care. This town is located in a Brazilian region called "Zona da Mata Mineira" and according to the latest estimates from the Brazilian Institute of Geography and Statistics (IBGE), the municipality had in 2009 about 79 thousand inhabitants.
The analysis of data collected between the months of April and May, 2009 showed that most of the prescribed psychoactive drugs were clonazepam, fluoxetine, diazepam, amitriptyline, carbamazepine and phenobarbital (Table 1). Within the group of the most prescribed drugs, there were two benzodiazepines, agreeing with other epidemiological studies conducted in Brazil, which have stated that benzodiazepines are among the most used psychoactive drugs in the country.7-10 Two antidepressant drugs - a tricyclic antidepressant and a SSRI - were also on the list of the most frequently prescribed drugs in our study. Indeed, these antidepressant drugs have been listed, along with benzodiazepines, as one of the most widely used drugs in the previous cited literature studies.7-10 Official American estimates of drug use released in 2008 by the CDC (Centers for Disease Control, USA), place antidepressants as the third class of most commonly prescribed drugs, accounting for 4.2% of the overall prescriptions behind painkillers and lipid modifying drugs. Anxiolytics, sedatives and hypnotics - class that includes benzodiazepines - are behind the antidepressants drugs, corresponding to 3.8% of the prescriptions.11 Obviously, the profile of psychoactive drugs prescription in different localities worldwide is influenced by factors such as health policy, social conditions and even the local culture. Thus the results shown here reflect the municipality of Manhuaçu, and, although it agrees with much of the data collected in other Brazilian cities7-10, it may be in conflict with data collected in different regions. An interesting example that illustrates this fact comes from data reported in 1999 addressing the analysis of psychoactive drugs prescriptions in the region of Al-Qassam, Saudi Arabia.12 In this study, the class of benzodiazepines was the least prescribed psychoactive drugs, reflecting the political recommendations and local laws towards the restriction of the rampant prescription of such drugs observed during the 1980s.12
Another interesting finding of our study was the gender segregation of psychoactive drug prescription profile in Manhuaçu: women take more psychoactive drugs then men. This observation agrees with literature data collected in different regions of Brazil.7-9 It has been anticipated that, in general, women are more perceptive to the symptoms, seek medical help earlier and are less resistant to drugs than man.13,14 Moreover, it is a consensus that common psychiatric disorders - as anxiety and depression - are more frequent diagnosed in women than in men.15
We have also found significant differences in the types of drugs used by men and women. The female sex was associated with a far greater use of antidepressants, both tricyclic and SSRIs. According to epidemiological studies, depression is nearly twice as common in women than in men16 and this disparity is considered as a fact by the World Health Organization (WHO).17,18 Therefore, the prevalent dispensation of antidepressants drugs for women over men found in the city of Manuhuaçu corroborated with national and international statistics concerning depression care. Even though there have not been published data, at least to our knowledge, reporting gender differences regarding the overall prevalence of less common mental illnesses, such as schizophrenia and bipolar disorder, we have observed a higher frequency of antiepileptic and mood stabilizer drugs dispensation to men than to women in Manhuaçu. It is possible that the observed profile reflects a peculiarity of the studied region or might even be a result of the extensive use of antidepressants by women, which could influence the overall statistical analysis. Concerning the higher prescription of biperiden to men when compared to women in Manhuaçu, one might predict that this fact results from the higher risk of male to develop Parkinson's disease, as well as the earlier development of the pathology symptoms.19 Finally, regarding the marital status, the only statistically significant result in our study was the lower use of antiepileptics and mood stabilizers by married men when compared to other civil statuses, and also the higher use of these classes of medications by single women when compared to women who were married at the time of the questionnaire application or before it. It is noteworthy that the epidemiological literature often identifies a lower prevalence of mental disorders among married individuals as well as greater use of psychoactive drugs in single, divorced or widowed subjects.20,21
We have also observed that the number of patients receiving psychotherapy is directly influenced by patients' age, which is consistent with the literature. According to some statistical studies, the use of such drugs increases dramatically with aging, and this trend is also observed specifically for psychoactive drugs, with a slight drop after 75 or 80 years of life.7,9,22 These observations raise a relevant but yet controversial discussion. Despite the higher use of psychoactive drugs by the elderly, epidemiological data indicate a lower prevalence of mental disorders in these patients, and they are generally more prone to adverse reactions due to changes in drug pharmacokinetics, cognitive and visual problems, several concomitant diseases and the simultaneous use of many drugs. The extent to which the prescription of psychoactive drugs to elderly patients is relevant is polemical and raised deep discussions.19,23 The age of the patient also appeared to be associated with the class of drug prescribed. As described in the results section, there have been increases in the prescription of benzodiazepines, tricyclic antidepressants and SSRIs versus decreases in the prescription of antiepileptics and antipsychotics drugs with patients' aging (Table 2). These phenomena were expected, given the fact that benzodiazepine and SSRIs are not recommended for children. In addition, although it is not yet a consensus, anxiety disorders and depression - the diseases most widely treated with these drugs - seem to increase with age.24,25 The decrease in the percentage of patients treated with antiepileptics or antipsychotics drugs in aged patients might also be explained by the increasing cases of depression-related problems with age. Another aspect likely associated with these observations is the precocity of the first signs and symptoms of schizophrenia and other psychotic disorders26, the same being applied to the first seizure notification27, and the control of the conditions in aged individuals.
It has been well established that multiple drug prescription directly correlates with a higher incidence of medication side effects and adverse reactions.28 Therefore, not exclusively drug prescription might be rational, but should also predict patients' benefits over risks of such therapeutical strategies. We have noted that the average of psychoactive drugs dispensation in Manhuaçu was 1.52 per patient, ranging from 1 to 6 drugs dispensed per individual, and although the vast majority of patients (62.4%) were using only one medication, the prescription of multiple psychoactive drugs have been also identified in a significant percentage of patients (38.6%) (Table 4). The combination of drugs is often necessary to control some of the mental illness, and such situations require special attention from health professionals as it exposes the individuals to secondary complications due to the medication adverse reactions or ineffective treatment. Data summarized in Table 5 shows the main drug associations observed in each patients' age group prescribed by SUS health professional in Manhuaçu. In patients younger than 20 years, it has been observed a high frequency of carbamazepine prescription combined with another antiepileptics or a neuroleptic compound. In children under 10 years old, periciazine was the most prescribed drug in combination with carbamazepine, but we have also observed the prescription of carbamazepine in combination with valproic acid or phenobarbital. The association of valproic acid and carbamazepine was the most frequent drug combination regimen prescribed for patients between 11 and 20 years of age. It is known that carbamazepine induces not exclusively its own metabolism, but also the metabolism of other substances as valproate29, so that the combination of these two drugs requires special attention, especially in younger individuals. In the population over 20 years old, it have been noted that the association of an antidepressant and a benzodiazepine has become the most commonly prescribed regimen. This association is very frequently used in the treatment of depression and anxiety disorders, and, despite not having available the patients' diagnosis information, we can suppose that the patients using this drug association in Manhuaçu are under treatment for one of these diseases.30,31
Other less commonly observed drug associations in Manhuaçu deserve special attention due to potential important medication interactions, such as might be observed with the concomitant use of two benzodiazepines and in the association of phenobarbital and valproic acid. Valproic acid is known to inhibit the metabolism of phenobarbital, and concomitant use of these two drugs can cause barbiturate intoxication.32 Association of lithium carbonate and haloperidol was observed in one patient. A close monitoring of this patient is a crucial procedure to assure a good individual health being, specifically to the possible development acute neurotoxicity.33 In addition to the aforementioned requirements, other potentially dangerous therapeutical regimens have been identified in Manhuaçu Public Health Care System, such as the combination of clomipramine or fluoxetine with carbamazepine and also the association between antidepressants and clomipramine. Combination of fluoxetine and carbamazepine was shown to reduced serum carbamazepine concentrations34 and serotonin syndrome has been reported with co-administration of these drugs.35 Carbamazepine is a potent inducer of Cytochrome P450 3A4 (CYP3A4) enzyme and other oxidative enzyme system in the liver, and it may also increase glucuronyltransferase activity, which influences the metabolism of several drug classes, including tricyclic antidepressants, such as clomipramine36, and the co-administration of carbamazepine and clomipramine demands precaution.
Conclusions
We herein present an analysis of the profile of psychoactive drugs dispensation by SUS in the city of Manhuaçu, Minas Gerais, Brazil, designed through the generation of a correlated database platform. We report here some trends in prescription and use of these medications in the Brazilian region, many of them found in similar studies made in other national and international locations. Most importantly, data shown intend to technically support the rational use of psychoactive drugs, as they will to provide deeper scientific background to pharmaceutical care. It is worthwhile pointing out that the generated database will be continually updated to enable the effective monitoring of patients attended by SUS in Manhuaçu, and more broadly in the global Brazilian Health Care System.
Conflicts of interest
The authors declare no conflict of interests.
References
1. de Leon J, Becoña E, Gurpegui M, Gonzalez-Pinto A, Diaz FJ. The association between high nicotine dependence and severe mental illness may be consistent across countries. J Clin Psychiatry. 2002;63(9):812-816. [ Links ]
2. Pincus HA, Tanielian TL, Marcus SC, Olfson M, Zarin DA, Thompson J, Magno Zito J. Prescribing trends in psychotropic medications: primary care, psychiatry, and other medical specialties. JAMA. 1998;279(7):526-531. [ Links ]
3. Tajima O. Mental health care in Japan: recognition an treatment of depression and anxiety disorders. J Clin Psychiatry 2001;62 Suppl 13:39-44. [ Links ]
4. Ungvari GS, Chung YG, Chee YK, Fung-Shing N, Kwong TW, Chiu HF. The pharmacological treatment of schizophrenia in Chinese patients: a comparison of prescription patterns between 1996 and 1999. Br J Clin Pharmacol. 2002;54(4):437-444. [ Links ]
5. Sistema Nacional de Informações Tóxico Farmacológicas [Internet]. Evolução dos Casos Registrados de Intoxicação Humana por Agente Tóxico 2009. (cited 2010 Jul 14). Available from: http://www.fiocruz.br/sinitox_novo/media/tab10_brasil_2007.pdf [ Links ]
6. Yusuff KB, Tayo F, Aina BA. Pharmacists' participation in the documentation of medication history in a developing setting: An exploratory assessment with new criteria. Pharmacy Practice (Internet) 2010;8(2):139-145. [ Links ]
7. Tancredi FB. Aspectos Epidemiológicos do Consumo de Medicamentos Psicotrópicos pela População de Adultos do Distrito de São Paulo. Dissertação (Mestrado), Faculdade de Saúde Pública, Universidade de São Paulo, 1979. [ Links ]
8. Mari JJ, Almeida-Filho N, Coutinho E, Andreoli SB, Miranda CT, Streiner D. The epidemiology of psychotropic use in the city of São Paulo. Psychol Med. 1993;23(2):467-474. [ Links ]
9. Almeida LM, Coutinho ESF, Pepe VLE. Consumption of Psychotropic Drugs in an Administrative Region of the City of Rio de Janeiro: Ilha do Governador. Cad. Saúde Públ. 1994;10(1):5-16. [ Links ]
10. Noto AR, Carlini EA, Mastroianni PC, Alves VC, Galduróz JC, Kuroiwa W, Csizmar J, Costa A, Faria MA, Hidalgo SR, de Assis D, Nappo SA. Análise da prescrição e dispensação de medicamentos psicotrópicos em dois municípios do Estado de São Paulo. Rev Bras Psiquiatr. 2002;24(2):68-73. [ Links ]
11. Schappert SM, Rechtsteiner EA. Ambulatory medical care utilization estimates for 2006. Natl Health Stat Rep. 2008;6(8):1-29. [ Links ]
12. al-Ghamdy YS, Qureshi NA, Abdelghadir MH, al-Habeeb TA, Ahmad SA. Psychotropic drugs prescriptions in Al-Qassim region, Saudi Arabia. East Mediterr Health J. 1999;5(1):27-34. [ Links ]
13. Cafferata GL, Meyers SM. Pathways to psychotropic drugs: Understanding the basic of gender differences. Med Care. 1990;28:285-298. [ Links ]
14. Kroenke K, Spitzer RL. Gender differences in the reporting of physical and somatoform symptoms. Psychosom Med. 1998;60(2):150-155, [ Links ]
15. Gater R, Tansella M, Korten A, Tiemens BG, Mavreas VG, Olatawura MO. Sex differences in the prevalence and detection of depressive and anxiety disorders in general health care settings: report from the World Health Organization Collaborative Study on Psychological Problems in General Health Care. Arch Gen Psychiatry. 1998;55(5):405-413. [ Links ]
16. Bebbington P. The origins of sex differences in depressive disorder: Bridging the gap. Int Rev Psychiatry. 1996;8(4):295-332. [ Links ]
17. Murray JL, Lopez AD. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Boston: Harvard School of Public Health, World Health Organization; 1996. [ Links ]
18. Piccinelli M, Homen FG; Gender differences in the epidemiology of affective disorders and schizophrenia. Geneva: World Health Organization; 1997. [ Links ]
19. Haaxma CA, Bloem BR, Borm GF, Oyen WJ, Leenders KL, Eshuis S, Booij J, Dluzen DE, Horstink MW. Gender differences in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2007;78(8):819-824. [ Links ]
20. Voyer P, Cohen D, Lauzon S, Collin J. Factors associated with psychotropic drug use among community-dwelling older persons: A review of empirical studies. BMC Nursing. 2004;3(1):3. [ Links ]
21. Cotten SR. Marital Status and Mental Health Revisited: Examining the Importance of Risk Factors and Resources. Fam Relat. 1999;48:225-233. [ Links ]
22. Stolker JJ, Heerdink ER, Leufkens HG, Clerkx MG, Nolen WA. Determinants of multiple psychotropic drug use in patients with mild intellectual disabilities or borderline intellectual functioning and psychiatric or behavioral disorders. Gen Hosp Psychiatry. 2001;23(6):345-349. [ Links ]
23. Blazer D, Hybels C, Simonsick E, Hanlon JT. Sedative, hypnotic, and antianxiety medication use in an aging cohort over ten years: a racial comparison. J Am Geriatr Soc. 2000;48:1073-1079. [ Links ]
24. Berg S, Dellasega C. The use of psychoactive medications and cognitive function in older adults. J Aging Health. 1996;8:136-149. [ Links ]
25. Beekman AT, Deeg DJ, van Tilburg T, Smit JH, Hooijer C, van Tilburg W. Major and minor depression in later life: a study of prevalence and risk factors. J Affect Disord. 1995;36:65-75. [ Links ]
26. Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med. 2000;30(1):11-22. [ Links ]
27. Munk-Jørgensen P. First-admission rates and marital status of schizophrenics. Acta Psychiatr Scand. 1987;76(2):210-216. [ Links ]
28. Sridharan R. Epidemiology of epilepsy. Curr Sci India. 2002;82(6):664-670. [ Links ]
29. Sovner R. A clinically significant interaction between carbamazepine and valproic acid. J Clin Psychopharmacol. 1998;8:448-449. [ Links ]
30. Dunlop BW, Davis PG. Combination Treatment With Benzodiazepines and SSRIs for Comorbid Anxiety and Depression: A Review. Prim Care Companion J Clin Psychiatry. 2008:10(3):222-228. [ Links ]
31. Smith WT, Londborg PD, Glaudin V, Painter JR. Short-term augmentation of fluoxetine with clonazepam in the treatment of depression: a double-blind study. Am J Psychiatry. 1998;155:1339-1345. [ Links ]
32. Patel IH, Levy RH, Cutler RE. Phenobarbital--valporic acid interaction. Clin Pharmacol Ther. 1980;27:515-521. [ Links ]
33. Keitner GI, Rahman S. Reversible neurotoxicity with combined lithium-haloperidol administration. J Clin Psychopharmacol. 1984;4(2):104-105. [ Links ]
34. Pearson HJ. Interaction of fluoxetine with carbamazepine. J Clin Psychiatry. 1990;51:126. [ Links ]
35. Broesen K. Kragh-Soerensen P. Concomitant intake of nortriptyline and carbamazepine.Ther Drug Monit. 1993;15:258-260. [ Links ]
36. Spina E, Pisani F, Perucca E. Clinically significant pharmacokinetic drug interactions with carbamazepine. An update. Clin Pharmacokinet. 1996;31(3):198-214. [ Links ]
Received: 21-Sep-2010
Accepted: 15-Oct-2011












 Curriculum ScienTI
Curriculum ScienTI