INTRODUCTION
Despite significant improvements to health care delivery, health information technology, and the availability of new medicines, medication-related problems persistently and detrimentally affect patient safety, quality of life, affordability and quality of care provided throughout the United States. Unfortunately, little has changed since the Agency for Healthcare Research and Quality reported more than a decade ago that roughly 770,000 injuries or deaths result annually from adverse drug events, including an estimated USD 1.6 - USD 5.6 billion annual financial burden on U.S. hospitals.1
Even so, feasible solutions to these problems remain elusive. Investment in interprofessional education and training for all health care providers, realization of the full potential of electronic medical records, and continued efforts to advance pharmacy practice (e.g., positioning qualified pharmacists to provide direct patient care and contribute to medication optimization) represent a promising multi-pronged approach.2However, capitalization on these investments must also align with the creation of sound policies as well as credentialing and privileging processes.
ADVANCING PHARMACY PRACTICE
Who? Trailblazing versus settling? Context is important. One might liken the historical efforts to settle the western frontier of the U.S. to current efforts aimed at advancing pharmacy practice. Much like the trailblazers that established the Oregon Trail, pioneering pharmacists have created new spaces for providing meaningful patient care that enables the evolving pharmacist workforce to not only occupy but also to expand existing territories.
What, where, and how? As with all things, it is important to define key terms. In this case, advancing pharmacy practice refers to the underlying efforts, processes, and incentives that drive changes to pharmacy practice over time. The pharmacy profession is incredibly diverse and incorporates practices in a variety of settings, including community-based pharmacies, integrated health systems, private practices, federal/government systems, and academic institutions. Furthermore, some practices are more specialized, examples of which are equally diverse and include both technically oriented (e.g., sterile compounding and nuclear pharmacy) and clinically oriented (e.g., pharmacotherapy and cardiology) specialties. These are all important factors to consider in any meaningful discussion about pharmacy practice advancement.
If advancing pharmacy practice can be represented as an equation, integral variables arguably include: 1) the scope of practice regulation; 2) interprofessionalism (i.e., interprofessional education, training, and practice); 3) remuneration for medication management services; 4) credentialing (i.e., the process of granting a credential, a designation that indicates qualifications in a subject or area, or the process by which an organization or institution obtains, verifies, and assesses an individual’s qualifications to provide patient care services); and 5) privileging (i.e., the process by which a health care organization, having reviewed an individual health care provider’s credentials and performance and found them satisfactory, authorizes that person to perform a specific scope of patient care services within that organization).
While these variables are individually important to consider, they are also interrelated in the sense that they overlap in practice. For example, the scope of practice for practitioners is generally governed by regulations in a given jurisdiction (i.e., in the U.S., this is determined by state boards of pharmacy); however, these often dovetail with a specific institution’s credentialing and privileging processes that are necessary to determine which practitioners are qualified to provide direct patient care in certain settings or conditions. Even so, the essential argument for “why” advancing pharmacy practice is important largely draws from evolving patient care demands as well as public and population health initiatives. Take, for instance, that medication use is increasingly complex and costly, necessitating enhanced knowledge, skills, and abilities from all involved health professionals to ensure optimal use. Without this, the costs to society and health systems of non-optimized medication therapy are unsustainable and, ultimately, unbearable.3
Success will be determined by the extent to which direct and indirect patient care endeavors are enhanced and medication use is optimized. While it might be challenging initially to demonstrate success, examples of meaningful leading indicators include: 1) community-based pharmacists incorporating clinical screening services and disease state-management programs into pharmacy settings; 2) health system pharmacists taking on additional direct patient care responsibilities along with clinical support responsibilities (e.g., informatics, formulary management, investigational drug services); and 3) other health professionals (i.e., physicians, nurses, physician assistants, and others) actively collaborating with pharmacists across the spectrum of care delivery.
HOW BOARD CERTIFICATION SUPPORTS ADVANCING PHARMACY PRACTICE
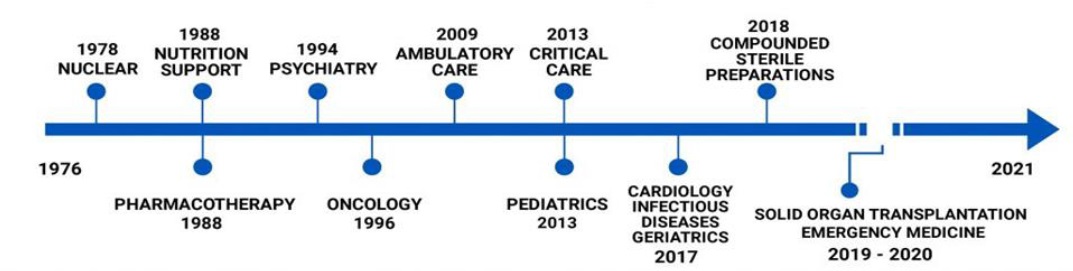
The Board of Pharmacy Specialties (BPS) was established in 1976 and certifies pharmacist specialists in 13 specialties in the U.S. and internationally, including ambulatory care, cardiology, compounded sterile preparations, critical care, geriatrics, infectious diseases, nuclear pharmacy, nutrition support, oncology, pediatrics, pharmacotherapy, psychiatric pharmacy, and solid organ transplantation (Figure 1).4As a non-governmental certifying body, BPS adheres to a board certification construct that grants credentials on a voluntary basis, meaning certification is not required for entry to practice like licensure/registration. However, it is the professional expectation for specialists to demonstrate qualifications for advanced practice. BPS certification is based upon an independent assessment of an individual’s knowledge, skills, and experience. In addition, BPS seeks national (through the National Commission of Certifying Agencies) and international (under International Standards Organization) accreditation for its certification programs to demonstrate its commitment to uphold and maintain high quality credentials.
Board certification is an intentionally rigorous process whereby an independent assessment of competency level, facilitated through a psychometrically sound and legally defensible process, establishes the competency level necessary for the “minimally proficient specialist” (i.e., as defined by bona fide subject matter experts in any given specialty or advanced practice). This is generally validated through a summative high-stakes examination, and ultimately assures patients, the public, payers, providers, and other stakeholders that those earning the credential meet the level of competency defined as the standard. As a standalone credential, BPS board certification independently validates an individual’s education, training, and accumulated post-licensure practice experience and augments other formative processes that foster professional development (e.g., postgraduate residency and fellowship training).
It is important to differentiate board certification from other types of credentials. In contrast to certificate training programs, continuing education programs, professional degrees, or postgraduate and training certificates, certifications are voluntary and issued by non-government agencies. In addition, certifications generally maintain rigorous criteria to determine who is considered eligible to sit for a board certification examination in each specialty. For BPS, each recognized specialty is governed by a specialty council, consisting of nine members (seven of whom are board-certified in that specialty, plus two non-specialist members) who are recognized and vetted as bona fide subject matter experts in that specific specialty. Each specialty council develops recommendations for board eligibility, which can typically be achieved in one of three ways: 1) ASHP-accredited PGY-2 specialty residency completion in the relevant specialty; 2) ASHP-accredited PGY-1 residency completion plus one to two years of specialized practice experience (i.e., more than 50% of an individual’s practice corresponds to one or more domains of the existing specialty certification content outline); or 3) three to four years of specialized practice experience in the absence of residency training. Additionally, specialty councils determine which examination questions will be administered with the goal of producing an independent, psychometrically validated assessment of knowledge, skills, and experience. Psychometrically sound scoring processes are employed to ensure reliability and fairness for all candidates, and examination raw scores are equated to a standardized scale before results are reported to individual candidates.
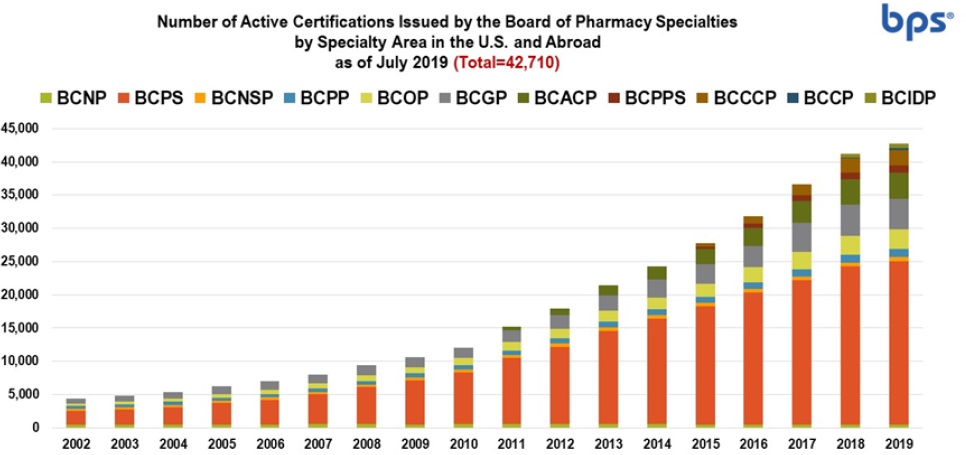
There are presently more than 35,000 pharmacist specialists who have earned more than 42,000 BPS certifications, meaning more than 7,000 pharmacist specialists have earned multiple certifications. This includes U.S. pharmacists as well as pharmacists practicing in more than 30 countries worldwide. As shown in Figure 2, the number of certifications issued has steadily increased from 2002 through 2008, with a significantly increased growth trend appearing between 2009 and 2018. Taken together, these figures illustrate growth in both number of certifications and board-certified pharmacist specialists. In addition, several new pharmacy practice specialties have been recognized recently (e.g., cardiology, infectious diseases, compounded sterile preparations, and solid organ transplant) which, arguably, reflects pharmacy practice advancement.
For pharmacy and other health professions, board certification is considered a sufficient, if not sole, criterion for demonstrating qualifications for direct patient care practice or for highly specialized technical services, such as preparation of sterile compounds or radiopharmaceuticals, as part of institutional credentialing and privileging processes (which are generally tailored to the complexity of the care provided to patients in a given setting). Board certification of pharmacist specialists is also woven into the credentialing framework articulated by the Council on Credentialing in Pharmacy in its 2014 resource paper.5Developed by a national coalition of pharmacy professional societies and organizations with a stake in credentialing for pharmacists and pharmacy technicians, this article describes how post-licensure scope of practice for pharmacists relates to education, training, and post-licensure credentials, including BPS board certification. Figure 3provides a framework to illustrate the alignment between a pharmacist’s scope of practice (ranging from broad to narrow focus along with increasing level of knowledge, skills, and experience required) and available post-licensure credentials. In other words, advancing pharmacy practice requires one to possess a commensurate level of knowledge, skills, and experience, which are provided through training (e.g., postgraduate residency training) and practice experience, and validated through independent assessment (e.g., board certification).
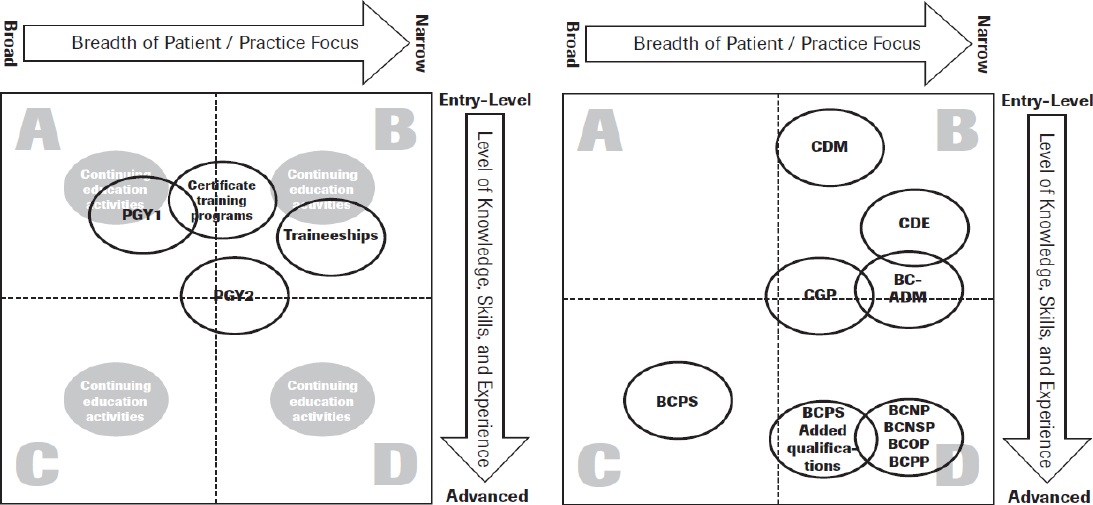
PGY1 = Post Graduate Year One (Residency), PGY2 = Post Graduate Year Two (Residency), BC-ADM = Board Certified-Advanced Diabetes Management, BCNP = Board Certified Nuclear Pharmacist, BCNSP = Board Certified Nutrition Support Pharmacist, BCOP = Board Certified Oncology Pharmacist, BCPP = Board Certified Psychiatric Pharmacist, BCPS = Board Certified Pharmacotherapy Specialist, CDE = Certified Diabetes Educator, CDM = Certified Disease Manager, CGP = Certified Geriatric Pharmacist
Figure 3. Council on Credentialing in Pharmacy (CCP) 2009 paper: Scope of contemporary pharmacy practice: Roles, responsibilities, and functions of pharmacists and pharmacy technicians [Reproduced with permission].
CONCLUSIONS
As pharmacy practice continues to advance to meet the evolving needs of our society, board certification remains the most rigorous credential to demonstrate competency for specialist practice. As a key component of professional self-regulation, it demonstrates the pharmacy profession’s commitment to uphold the covenantal relationship with patients and, by extension, the social contract with the public required to preserve the trust in pharmacists’ ability to optimize medication use in collaboration with other health care providers.