INTRODUCTION
Hospital readmissions are considered as the primary indicator of insufficient quality of care and are responsible of increasing annual medical costs by billions of dollars.1 In fact, a readmission is defined by the Hospital Readmissions Reduction Program (HRR) as a patient reentering the hospital within a certain time interval after discharge (around 30 days).1,2 This HRR program tends to reduce service’s costs and to ameliorate the effective role of healthcare providers as well as hospital performances in order to improve patients’ outcomes.2 Different factors contribute to this higher rate of readmissions such as: complications from inpatient treatment during hospitalization or from the illness itself, adverse drug events, patient’s own behaviors towards recommendations, lack of follow up after discharge and lack of appropriate discharge instructions.2 Not all hospital readmissions are preventable, but studies have shown that a meticulous strategic therapeutic plan to improve inpatient care in addition to valuable discharge instructions can prevent loads of unnecessary hospital readmissions.3
One of the most important educational communications between patients and healthcare professionals is the one related to discharge instructions. Those instructions are defined as any form of recommendations given to the patient or to a close family member, in an oral or written way, upon discharge home for the purpose of a continuous appropriate home care.4 Studies have shown the crucial role of discharge instructions especially when the patient is admitted through the emergency department because of a sudden event related either to his medications or to a lack of follow up in order to have a better management of his illnesses.5,6 Several studies in different countries have evaluated patient understanding of discharge instructions in the emergency department such as a study done by Hasan Sheikhet al. in Canada in 2018.7 The results of this study were as follow: 70% of the 150,000 participants presented an incomplete or poor understanding of treatment discharge instructions, 47% for the diagnosis and 55% for the follow up instructions.
In fact, effective discharge instructions are defined by their content, delivery, comprehension and implementation. The best description of discharge instructions’ content is divided into four main parts. The first part concerning the disease should contain an easy definition of the physiopathology, a quick review on all symptoms, and basic information about complications caused by the disease so that the patient is more aware and responsible of his state. Recommendations related to home medications take place in the second part: posology, duration of the treatment, side effects, administration method and major interactions. This part should be more detailed in case of poly-medication in order to minimize the risk of any confusion. The third part is related to the follow up: laboratory tests, hemorrhagic signs, precautions of use, etc. Lifestyle modifications are summarized in the last part.7 Furthermore, the delivery of the information is a main issue since it depends on the person in charge, the way of communication, the time spent and the type of recommendations that should be given. Discharge instructions are usually delivered by physicians, nurses or clinical pharmacists. In fact, strong nurse-patient relationship is easy to build since nurses are the healthcare providers in utmost contact with the patient. Therefore, nurse-patient communication sometimes do not lead to personal satisfaction since physicians are the ones in charge of taking decisions in the management of the patient’s health.8 As for clinical pharmacists, they are not always present in all hospitals. In addition, instructions may be oral or written. Oral instructions should be based on good communication skills and an adequate learner-instructor relationship. It has to be clear, unambiguous and straight to the point. Nevertheless, the main limit of oral communication remains the misunderstanding of the patient and the poor memorization. This is the reason why they should be complemented by written emergency department discharge instructions.4 Not to forget the marked difference in comprehension according to the level of education of the patients.9 Consequently, a good implementation of discharge instructions will contribute to a better patient adherence to the treatment. This adherence is defined as patient’s behavior towards recommendations of healthcare providers.10 In reality, it is much more difficult to be compliant to sophisticated treatments with highly complicated regimens and devices. Poly-medication is one of the factors that affect patient adherence: a patient taking five medications or more has an elevated risk of confusion and interaction between pills and requires a closer monitoring and follow up.11
In Lebanon, the situation in hospitals might be alarming since most of healthcare providers do not have sufficient time to appropriately educate patients at discharge. The consequences of this problem are recently more perceived with the continuous elevation of readmissions due to the lack of follow up and the absence of education. In fact, Lebanese hospitals suffer from a reduced number of nurses and clinical pharmacists as shown by a study done in 2013 by El Jardaliet al.12 This problem is becoming much more serious over the years since the number of hospitalized patients is in continuous elevation and the staff is overloaded.13 In addition, the medical field in Lebanon does not offer individual treatments ignoring the importance of the unity of the human person. As shown in the study done in 2012 by Abou Mradet al. demonstrating the diversity in the quality of care in Lebanon.14 This highlights the role of emergency individualized discharge instructions in order to ameliorate healthcare services in Lebanon and minimize damages resulting from patients’ acknowledgements.
Despite the aforementioned facts, no study targeted discharge instructions in Lebanon. Thus, we conducted the present study to evaluate discharge instructions given to hospitalized Lebanese patients and associated factors.
METHODS
Study design
We conducted a dual-phase study which included live observations of discharge instructions and a subsequent in person patient survey at a Lebanese University hospital in Beirut from April 1st till the end of September 2018. Participants were recruited prospectively from the emergency department of the hospital that receives approximately 150,000 patients each year. Approval for the study protocol was obtained from the ethical committee of the hospital (2018-IRB-017R).
The sample size was calculated using the Epi InfoRM software, version 7.2.2.2. We applied the statistical calculation method for cross-sectional studies in the “population survey” category. We fixed our margin of error at ± 5% and our type I error at 5%. As for our expected frequency, it was based on the results of an article by Engelet al. (2012), where the authors conducted a similar study in Boston.17 Their results were as follows: knowledge deficits were frequent in the domains of follow up (39%), medications (22%) and diagnosis (14%). Thus, we obtained a minimum sample size of 185 patients. Following this calculation, we decided to enroll 200 patients in our study.
Inclusion and exclusion criteria
We targeted all Lebanese patients, aged between 18 and 80 years, admitted to the emergency department between April and July 2018. We chose the emergency department since we considered patients entering through this department having critical situations that impose more serious discharge instructions in order to avoid later readmissions.
We excluded patients with cognitive impairments or mental disorders and patients who were not independent in their activities of daily living (such as eating, bathing, dressing, toileting, etc.). We also excluded patients who visited the emergency department for few hours and were directly discharged home. Finally, patients transferred to the intensive care unit, coronary care unit, operation room and maternity were also excluded.
Collection method
Either the doctor in charge of the patient or the chief of nurses in the service or sometimes the resident or the fellows during their shifts give discharge instructions at the hospital.
Each patient admitted to the emergency department answering our eligibility criteria was followed up during his hospitalization for potential recruitment.
The staff was informed about the study in order not to miss the patient’s discharge time, but the study objective was not completely revealed not to bias the discharge instructions and behavior of the physician/nurse. Instead, we told them that we were conducting a study about medications prescribed at discharge. We further asked the hospital committee not to unveil our study true objective since its benefits outweigh its risks.
When ready to leave, the patient was checked by the physician/nurse for the last time and was given the discharge instructions, we detected the time spent for giving the instructions and intervened to fill out a pre-established questionnaire after taking the patient’s oral consent to participate in the study. We informed the patient that data will be kept confidential and that he had the right to quit the study at any time.
We also collected some information concerning final diagnosis, past medical and medication history from the patient’s medical file.
A clinical pharmacist was in charge of filling the questionnaires and he was always a silent observer while the instructions were given.
Data collection tool
We searched the literature for similar studies, in order to prepare our data collection sheet.7,15,16 The latter included a total of 28 questions divided into 3 sections in order to cover all the correlates of patient’s understanding of discharge instructions.
The first section concerned the socio-demographic characteristics of our participants like BMI, level of education, work, medical insurance, marital status, physical activity, alcohol and smoking status. Section 2 concerned the patients’ medical history, admission to the hospital, doctor’s previous knowledge of the case and the patient in addition to new medications added at discharge.
Questions related to the instructions were presented in section 3: whether the instructions were given or not, who gave them, the time spent to achieve this task, the person who received them and if they were written or oral. Different types of instructions were defined: the ones related to the medication (posology, duration, side effects, interactions, administration method…), the follow up instructions (lab tests, precautions of use hemorrhagic signs…) and instructions about lifestyle modifications such as exercise, food habits, alcohol and smoking. We did not tackle information given about the disease.
The questionnaire was filled by a face-to-face discussion with the patient. The data collection procedure was piloted on 10 patients in order to test its feasibility, objectivity and reliability. Data from the pilot study was not included in the statistical analysis.
Primary outcome measures
We first reported if the instructions related to medications, follow up plan and lifestyle modifications were “given or not”, i.e. our primary outcome. Then in case it was given, we reported if it was “appropriate or not” based on the conformity of the instructions with the discharge prescription and based on what the instructor said. Meanwhile, we checked each discharge prescription before filling the questionnaire with the patients. We intervened immediately after the instructions were given in order to limit memorization bias.
Statistical analysis
Data were entered and analyzed using SPSS software version 20.0. Descriptive statistics were first conducted in which qualitative variables were presented by proportions and percentages, while quantitative variables were described through their means and standard deviations (SD). In addition, we calculated the total percentages of the instructions given and appropriate and the percentage representing the ratio appropriate/given.
Then, a bivariate analysis was performed to study factors related to:
Medication instructions given included posology, duration, interactions, side effects and administration method instructions, which were combined into a score of five. This score was then divided based on its median: below the median represents a poor score (0), the median and above represents a good score (1).
Medication instructions appropriate included posology, duration and administration method instructions, which were combined into a score of three (and not 5 since instructions about interactions and side effects were rarely given). The score was then dichotomized as following: patients having a score of 1 or 2 were grouped as having a poor score (0) and patients having a score of 3 were considered having a good score (1).
Factors tested were socio-demographic and lifestyle characteristics, chief complaint, past medical and medication history, final diagnosis, post prescribed medications, reference by the Doctor to the emergency and instructions characteristics.
Pearson Chi-square test (or Fisher’s Exact test) and Student t-test were used for qualitative and quantitative variables respectively. A p-value <0.05 was considered statistically significant.
RESULTS
The participants of our study were aged between 21 and 79 years old and had an average body mass index (BMI) of 25 kg/m2. Males were more represented in our population (61.5%) and up to 84.0% of the participants were actually working or retired. Forty five percent have reached high school, 72.5% were married with 54.0% of children living with their parents. Most of our participants were from Mount Lebanon (46.0%) and Beirut (39.0%) having an income between 1000 and 2000 US dollars as shown inTable 1. Thirty-three percent of our participants were current smokers. Most of our participants were not alcoholic (52.0%) or drink alcohol rarely and occasionally (45.5%). The major chief complaint in the sample was pain (29.0%) including headache, chest pain, and trauma pain. Cardiology (15.0%) and gastrointestinal (14.5%) problems were the second causes of urgent hospital admissions. Hypertension was the most frequent past medical history among our participants (53.0%) followed by diabetes (30.5%). Most of our participants were under antihypertensive therapy namely beta-blockers (32.0%), angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers [ACEI/ARBs] (31.0%), diuretics (29.0%) and Calcium Chanel Blockers [CCBs] (13.0%). Statins (30.0%), antiplatelet (25.5%) and proton-pump inhibitors [PPIs] (19.5%) were also frequently present among patients’ drug history.
Table 1. Socio-demographic and lifestyle characteristics of participants (N=200)
| Characteristics | Mean (SD) / Frequency (%) |
|---|---|
| Age (years) | 60.09 (17.24) |
| BMI (kg/m2) | 25.74 (3.02) |
| Gender | |
| Male | 123 (61.5) |
| Female | 77 (38.5) |
| Level of education | |
| Less than high school | 44 (22.0) |
| High school | 91 (45.5) |
| University/Masters/PhD | 65 (32.5) |
| Region | |
| Mount Lebanon | 92 (46.0) |
| Beirut | 78 (39.0) |
| Other | 30 (15.0) |
| Marital status | |
| Married | 145 (72.5) |
| Single | 37 (18.5) |
| Widowed | 18 (9.0) |
| Having children | 157 (78.5) |
| Children living with you | 108 (54.0) |
| Living alone | 5 (2.5) |
| Work | |
| Yes | 80 (40.0) |
| No | 120 (60.0) |
| Monthly income | |
| < 1000$ USD | 4 (2.0) |
| 1000-2000 USD | 125 (62.5) |
| 2000-3500 USD | 53 (26.5) |
| > 3500 USD | 18 (9.0) |
| Medical insurance | 90 (95.0) |
| Smoking status | |
| Non-smoker | 103 (51.5) |
| Ex-smoker | 31 (15.5) |
| Current smoker | 66 (33.0) |
| Alcohol status | |
| No alcohol | 104 (52.0) |
| Rarely | 50 (25.0) |
| Occasionally | 41 (20.5) |
| Weekly/daily | 5 (2.5) |
| Physical activity | |
| Not at all | 158 (79) |
| < 150 min/week | 35 (17.5) |
| > 150 min/week | 7 (3.5) |
Our participants’ final diagnosis was distributed as follow: 30% were admitted after a trauma or fall for surgery purposes, 8.5% because of diabetes complications, 10.0% due to urinary tract infections (UTIs), 7.5% due to gastro-intestinal infections and 6.5% due to respiratory infections. At discharge, different medications were prescribed such as antibiotics (52.0%), PPIs (26.0%), analgesics (41.5%) and anti-inflammatories (10.0%), followed by antihypertensive medications i.e. beta-blockers (8.0%), CCBs (4.0%), ACEI/ARBs (3.5%), and diuretics (7.0%), and anti-diabetic agents (4-8%). Corticosteroids (14.5%) and anticoagulants (13.0%) were also frequently prescribed at discharge. Finally, 45.0% of our patients were referred to the hospital by a physician.
Eighty-two percent of our participants left the hospital with discharge instructions given while 17.5% did not receive discharge instructions. The time dedicated to the instructions was around 1-2 min in 55.0% of the cases. Nurses gave the instructions for 52.0% of our participants while 25.5% were given by physicians. Finally, almost all of the instructions given were oral (80.5%) (Table 2).
Table 2. Instructions’ characteristics (N=200)
| Instructions characteristics | N (%) |
|---|---|
| Time given | |
| 1-2 min | 110 (55.0) |
| 3-4 min | 50 (25.0) |
| 5 min | 4 (2.0) |
| < 5 min | 1 (0.5) |
| Instructor | |
| Physician | 51 (25.5) |
| Fellow/Resident | 10 (5.0) |
| Nurse | 104 (52.0) |
| Experience of the instructor | |
| >10 years | 124 (62.0) |
| <10 years | 41 (20.5) |
| Instructions were | |
| Oral | 161 (80.5) |
| Written | 4 (2.0) |
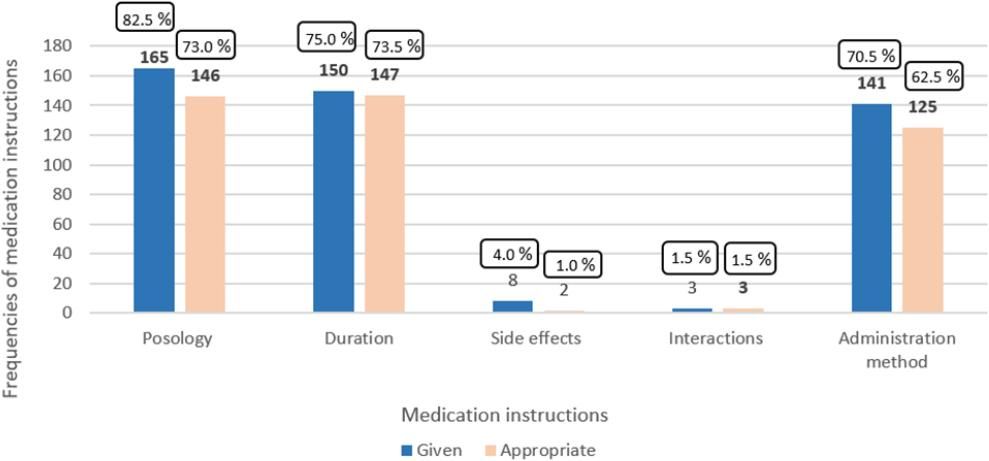
Three types of medication instructions were mostly given: posology (n=165; 82.5%), duration (n= 150; 75.0%) and administration method (n=141; 70.5%). When given, instructions were appropriate in 88.5%, 89.1% and 75.8% of the cases, respectively. Those percentages define the appropriateness of the total discharge instructions given, i.e., the medication related instructions based on the conformity with the prescription and the follow up and lifestyle instructions based on what the instructor said in the presence of the investigator. Furthermore, only 25.0% of instructions about side effects were appropriate while those about interactions were always appropriate although barely given (1.5%) (Figure 1).
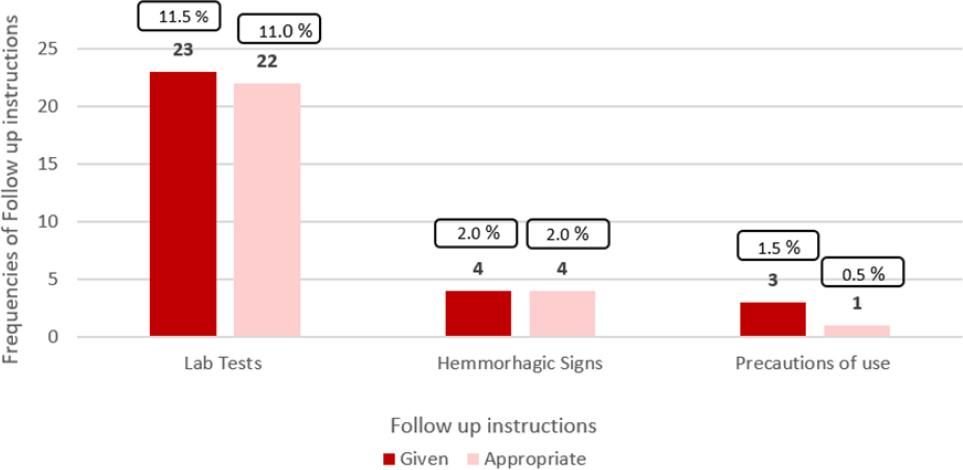
Follow up instructions were divided into lab tests, hemorrhagic signs and precaution of use instructions. The percentages of the following instructions given were respectively 11.5% (n=23), 2.0% (n=4) and 1.5% (n=3) and were almost appropriate for all the population. Ninety-six percent of the lab tests instructions given were appropriate and all of the hemorrhagic signs instructions too while only 33.3% of the precautions of use instructions were appropriate (Figure 2).
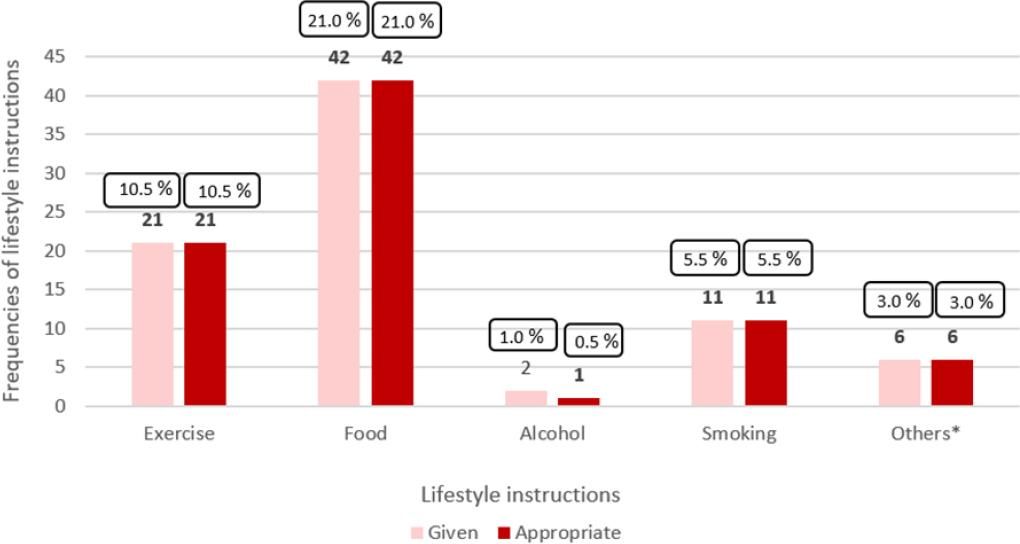
Exercise, food, alcohol and smoking lifestyle instructions were estimated in our study. The percentages of these instructions given were: 10.5% (n=21) for the exercise instructions, 21.0% (n=42) for the food, 1.0% (n=2) for the alcohol, 5.5% (n=11) for the smoking and 3.0% (n=6) for other lifestyle instructions such as sun exposure and water baths. Most of the instructions given were appropriate (Figure 3).
The median score was 3. So our dependent variable was dichotomized as follow: <3 formed the first part: medication instructions not given, 3 and above represented the second part: medication instructions given.
The results of the bivariate analysis showed that the instructor in charge of giving discharge instructions had its significant influence on medication instructions given (p=0.014). In fact, nurses gave less medications instructions in comparison with physicians, fellows and residents (Table 3).
Table 3. Results of the bivariate analysis between the dependent variable “medication instructions given” and different socio-demographic and instructions variables (N=200)
| Medication instructions not given (N=34) | Medication instructions given (N=131) | p-value | |
|---|---|---|---|
| Age (years) | 64.82 (11.25) | 60.66 (17.75) | 0.196 |
| Gender | 0.758 | ||
| Male | 22 (21.4) | 81 (78.6) | |
| Female | 12 (19.4) | 50 (80.6) | |
| Education level | 0.066 | ||
| < high school | 13 (32.5) | 27 (67.5) | |
| High school | 15 (19.5) | 62 (80.5) | |
| University/PhD | 6 (12.5) | 42 (87.5) | |
| Income per month | 0.926* | ||
| < 1000 USD | 1 (25.0) | 3 (75.0) | |
| 1000-2000 USD | 20 (19.4) | 83 (80.6) | |
| 2000-3500 USD | 10 (22.7) | 34 (77.3) | |
| > 3500 USD | 3 (21.4) | 11 (78.6) | |
| Time given | 0.156* | ||
| 1-2 min | 28 (25.5) | 82 (74.5) | |
| 3-4 min | 6 (12.0) | 44 (88.0) | |
| 5 min | 0 (0.0) | 4 (100.0) | |
| > 5 min | 0 (0.0) | 1 (100.0) | |
| Who gave? | 0.014* | ||
| Physician | 5 (9.8) | 46 (90.2) | |
| Fellow/resident | 0 (0.0) | 10 (100.0) | |
| Nurse | 29 (27.9) | 75 (72.1) | |
| Experience of the instructors | 0.806 | ||
| Experienced | 25 (20.2) | 99 (79.8) | |
| New | 9 (22.0) | 32 (78.0) | |
| Instructions were | 0.582* | ||
| Oral | 34 (21.1) | 127 (78.9) | |
| Written | 0 (0.0) | 4 (100.0) |
*Fisher exact test: cells have expected count less than 5
The score varied between 0 and 3, and was dichotomized as follow: 1 and 2 represented the medication instructions not appropriate and 3 represented the appropriate medication discharge instructions.
The bivariate analysis showed that the instructor in charge of giving the instructions (p=0.001) and the experience of the instructor (p=0.020) had a significant association with the dependent variable. This means that medication instructions given by physicians having 5 years of experience or more are more appropriate in comparison with the ones given by nurses (Table 4).
Table 4. Table showing the results of the bivariate analysis between the dependent variable “medication instructions appropriate” and socio-demographic characteristics (N=200)
| Medication instructions not appropriate (N=19) | Medication instructions appropriate (N=111) | p-value | |
|---|---|---|---|
| Age (years) | 62.32 (18.54) | 60.59 (17.62) | 0.697 |
| Gender | 0.388 | ||
| Male | 10 (12.5) | 70 (87.5) | |
| Female | 9 (18.0) | 41 (82.0) | |
| Education level | 0.220* | ||
| < high school | 2 (7.4) | 25 (92.6) | |
| High school | 10 (16.1) | 52 (83.9) | |
| University/PhD | 7 (17.1) | 34 (82.9) | |
| Income per month | 0.735* | ||
| < 1000 USD | 1 (33.3) | 2 (66.7) | |
| 1000-2000 USD | 12 (14.6) | 70 (85.4) | |
| 2000-3500 USD | 5 (14.7) | 29 (85.3) | |
| > 3500 USD | 1 (9.1) | 10 (90.9) | |
| Time given | 0.143* | ||
| 1-2 min | 10 (12.2) | 72 (87.8) | |
| 3-4 min | 8 (18.6) | 35 (81.4) | |
| 5 min | 0 (0.0) | 4 (100.0) | |
| > 5 min | 1 (100.0) | 0 (0.0) | |
| Who gave? | 0.001* | ||
| Physician | 4 (8.0) | 46 (92.0) | |
| Fellow/resident | 6 (60.0) | 4 (40.0) | |
| Nurse | 9 (12.0) | 66 (88.0) | |
| Experience of the instructors | 0.020* | ||
| Experienced | 10 (10.2) | 88 (89.8) | |
| New | 9 (28.1) | 23 (71.9) | |
| Instructions | 1* | ||
| Oral | 19 (15.1) | 107 (84.9) | |
| Written | 0 (0.0) | 4 (100.0) |
*Fisher exact test: cells have expected count less than 5
DISCUSSION
The main objective of our study was to evaluate discharge instructions in a Lebanese hospitalized population admitted through the emergency department. Our study included 200 participants aged between 21 and 79 years, among whom 61.5% males and 67% of a high school level or less. They were mainly from Mount Lebanon and Beirut (85%), married (72.5%) and having children (78.5%). The average BMI of our participants was 25.74 kg/m2, which is at the limit of being overweight. In fact, obesity is associated with additional comorbidities such as diabetes, cardiovascular disease and dyslipidemia.17 The evaluation of discharge instructions was based on whether the instructions were given or not and whether they were appropriate or not based on the conformity of the instructions with discharge prescriptions. We mainly focused on “medication” instructions including posology, duration, side effects, interactions and administration method. Eighty two percent of our participants received discharge instructions. The degree of appropriateness fluctuated between 25% and 100%. The instructor in charge of giving discharge instructions had its significant influence on medication instructions given (p=0.014). In addition, the instructor and his experience influenced the degree of “appropriate instructions”. In fact, our study showed that the instructions given by the nurses were important but significantly less effective in comparison with those given by the physicians, fellows or residents. However, nurses gave 52% of the instructions, which questions the reasons behind this difference in the quality of the instructions.
Follow up and lifestyle instructions are usually more individualized than other types of instructions which made our results difficult to interpret in this case; especially in a relatively small sample size and difficulty to stratify patients based on their clinical profiles. For example, hemorrhagic signs instructions should have been given when anticoagulants were prescribed at discharge. Moreover, no general rule to follow in case the instructions given were appropriate or no since it depends on the type of the molecule recommended. Only 15.4% of the hemorrhagic signs instructions were given and appropriate among our study population. Lab tests and precautions of use instructions should have been given for the majority of the participants. Therefore, barely 11.5% received the lab tests instructions (n=23) and 1.5% the precautions of use ones (n=3) and not all of those instructions given were appropriate. Exercise, food, alcohol and smoking instructions depended on each patient, his past lifestyle history, his age and his capacity. In fact, among past current smokers, the percentage of smoking instructions given was only 9.1% and they were all appropriate. Among past alcohol drinking participants including the ones drinking alcohol rarely, occasionally, weekly and daily, the percentage of alcohol instructions given remains 1% and there were appropriate in 50% of the cases. Food was the utmost given and appropriate lifestyle instruction (n=42; 21%) in this study.
“How well informed are patients when leaving from an admission through the emergency department?” the main question that arises as a result of this study. As we can see not all patients admitted through the emergency department leave the hospital with discharge instructions and not all discharge instructions are appropriate and well understood by the patients. Therefore, patients’ understanding of discharge instructions is still limited with low levels of comprehension and compliance to those recommendations. The reality of the situation in Lebanon is dangerous especially with adults suffering from several diseases and taking loads of medications including the ones added at discharge. In fact, poly-medication itself is a main risk factor of readmissions in the context of inaccurate and missing discharge instructions. Unfortunately, our small-sized and monocentral study limits the extrapolation of the results to other settings. However, our study is the first in Lebanon to evaluate patients’ understanding of discharge instructions and sheds light on alarming findings.
Our findings were more or less consistent with previous studies that found poor or incomplete patients’ understanding of discharge instructions. For example, the study done by Sheikhet al. in 2018 in Canada showed that almost half of patients (42%) did not receive complete discharge instructions. Seventy percent of the participants had incomplete understanding of the treatment instructions, 55% of the follow up ones while 33% had no or poor understanding of the treatment instructions and 24% for the follow up ones.7 In our study 100% of our participants did not receive complete discharge instructions which means that the situation in Lebanon is even worse. Another study done by Martyet al. in 2013 revealed that 83% of the study population received discharge instructions but not all were well assimilated. Patients correctly recalled 82% of the information received about diagnosis, 56% about examinations planned and 72% about follow up treatments. Medication instructions were most prone to forgetting or distortion.16
The results of our study highlighted the gap in the discharge instructions provided by various healthcare givers. Therefore, we expect that the presence of clinical pharmacists in Lebanese hospitals and their medication-related advice and instructions might be beneficial.18 First, they are responsible of the detection of drug-related problems (DRPs) for a better efficacy and safety in the use of drugs. The study done by Zaalet al. in 2013 showed that among 1206 medication review, 442 potential DRPs were identified, 286 (65%) DRPs were considered relevant and 247 (56%) of the proposed interventions were accepted.19 Another study done by Reiset al. in Brazil in 2013 revealed that among 6438 drug order assessed, 933 pharmacists’ intervention were performed.20 Those studies assured that the interventions of clinical pharmacists promote positive changes in the patient’s health. In addition, a reduction of annual costs due to drug related readmissions can be avoided by clinical pharmacists. The study done by Gallagheret al. in Europe in 2014 revealed this evidence. A total cost avoidance of 708 euros was generated because of clinical pharmacists’ interventions. Input costs were resumed by 82 euros what made a 626 euros cost benefit.21 Not to forget their imperative role in giving excellent discharge instructions since they are the drug experts of all healthcare professionals.
The study also pinpoints the lacking role of nurses, mainly due to the reduced number of nurses in Lebanese hospitals. Solutions should be found to promote nursing among university students and improve the socio-economic conditions of nurses in hospitals. This way, nurses would have more time for each patient and better discharge instructions would be given.
There were several limitations in this study. We assessed patients’ understanding at discharge immediately after their contact with their physician or nurse in order to limit the recall bias as much as possible. However, long term understanding of instructions and its impact on medications adherence, patients’ quality of life, wellbeing or readmission to hospital was not tackled in this study. Scores were created to conduct comparative analyses and cannot be objectively used to classify patients between good or poor levels of understanding. One investigator was in charge of data collection thus controlling for investigator bias. However, we believe that the face to face interview might have slightly improved the quality of the instructions and that a self-administered questionnaire would have been more close to reality.
Finally, healthcare providers (physicians and nurses) were not fully aware of the study objective not to influence their behavior towards discharge instructions. Thus, we consider that instructions were not intentionally given or explained and results were not positively affected.
Furthermore, the long-term understanding of the instructions should be taken into consideration especially with polypharmacy adults who need particular attention. This recall could be ensured by a good coordination between physicians, nurses, clinical and community pharmacists for the purpose of a better patient health. Individual pharmaceutical files are considered as an effective solution to ensure a better communication between healthcare providers themselves and the patients.
CONCLUSIONS
In conclusion, our observational study showed that in a Lebanese university hospital, patients’ understanding of discharge instructions is poor. Careful attention should be drawn to other hospitals as well and interventions should be considered to improve instructions quality and limit later complications and readmissions. The education of the patients should be more valuable, healthcare providers especially physicians should give more time and values for discharge instructions, and hospitals should enhance the role of clinical pharmacists and nurses in this matter. More work will be needed to define the major pillars of valuable discharge instructions.