INTRODUCTION
In the last decades, in line with international movements, pharmacy education in Brazil has engaged in debates about the need to redefine the profile of pharmacy graduates and to restructure the teaching-learning process.1 2 3-4Until 2002, pharmacy education was regulated by the minimum curricula, which divided pharmacy programs into two stages: the first one trained the pharmacist for community pharmacy work, and the second one was a complementary emphasis: in the pharmaceutical-industrial area or the biochemical area (including food technology, or clinical and toxicological analysis).5
In 1996, the minimum curricula were extinguished and the National Curriculum Guidelines (DCN, from the Portuguese acronym for Diretrizes Curriculares Nacionais) were established to pave the paths of higher education programs.6In the scope of pharmacy, the DCN were enacted in 2002 and changed the country's education philosophy, with a view of replacing the technicistic vision with generalist, humanistic, critical and reflexive training, preparing the pharmacist to act at all levels of health care.7,8Despite being a breakthrough in pharmacy education, generalist education, in expecting that professionals were able to perform well in all the activities described in the curriculum, ended up generating an excessive amount of hours to be fulfilled and a superficial approach, thus leading students to difficulty to connect and ascribe meaning to the new knowledge provided in the courses.9,10
Complementing the discussions about the pharmacist's social role, in 2017 new DCN were published for pharmacy programs in Brazil.11Regarding the profile of pharmacy graduates, the current DCN establish that they be health professionals with training in drugs, medicines and pharmaceutical service, and, in an integrated way, with training in clinical and toxicological analysis, cosmetics and food, for the health care of individuals, family and community.11Additionally, the DCN establish that the structuring of pharmacy undergraduate programs should have a total of about four thousand hours, which should be divided into three thematic axes: Health Care; Technology and Innovation in Health; and Health Management, making up respectively 50%, 40% and 10% of the program total hours.12
According to the DCN, the pharmacist must be trained according to competencies, and the teaching-learning process must be anchored in the four pillars of education (learning to know, learning to do, learning to live together, and learning to be) and committed with the construction and consolidation of the Brazilian National Health System (SUS, from the Portuguese acronym for Sistema Único de Saúde).4,11,13,14However, contrary to what is required by the DCN in terms of training, and despite the number of pharmacists in the SUS establishments having increased significantly in the last decade - from 12,122 to 28,271 between 2007 and 2015 -, pharmacists in Brazil operate predominantly in the private sector, being private community pharmacies the main setting (58%).15
According to Kolb, experiential learning is essential for knowledge creation, since learning occurs not only in the cognitive domain, but also in the affective domain, based on perception and action.16Therefore, the insertion of students into real-life scenarios, for example internships, represents a strategic component in the teaching-learning process. Compulsory internships, as provided for in the Political Pedagogical Projects of the pharmacy programs and required for the award of a diploma, are part of the student's training schedule. Moreover, they must be carried out in a work environment effectively monitored by a supervising teacher from the HEI and a supervisor from the host organization, who shall belong to the training staff at the internship site and be professionally qualified and experienced in the relevant area. The internship activity plan must be defined jointly by the HEI, the host organization, and the student; and it is up to the HEI to verify the facilities of the internship site and its suitability for the student's cultural and professional training, and to prepare the necessary instruments for internship assessments.17
The DCN determine that internships must correspond to a minimum of 20% of the program hours and be carried out in an articulated way, in increasing complexity throughout the program; however, each undergraduate program is free to determine the rules regarding the practical placement sites and supervision. Moreover, diversification of teaching-learning scenarios should be considered in order to allow the student to experience the professional reality. Thus, the internship hours should be distributed in the areas of pharmaceuticals, cosmetics, medicines and pharmaceutical assistance (60%), genetic and toxicological and food analyses (30%), and institutional and regional specificities (10%).11
In view of the importance of providing pharmacy undergraduates with experience in the teaching-learning process, a review of internships proves necessary in order to keep improving the profile of and the training in pharmacy programs in Brazil. Therefore, this study aims to provide an overview of pharmacy undergraduate programs in Brazil and their respective internships.
METHODS
In order to reach the proposed objective, a descriptive observational cross-sectional study was carried out. This paper is part of a larger study whose title translates to “Experiential education for pharmaceutical care: an ethnographic perspective”, which then is part of a doctoral dissertation.
Sampling
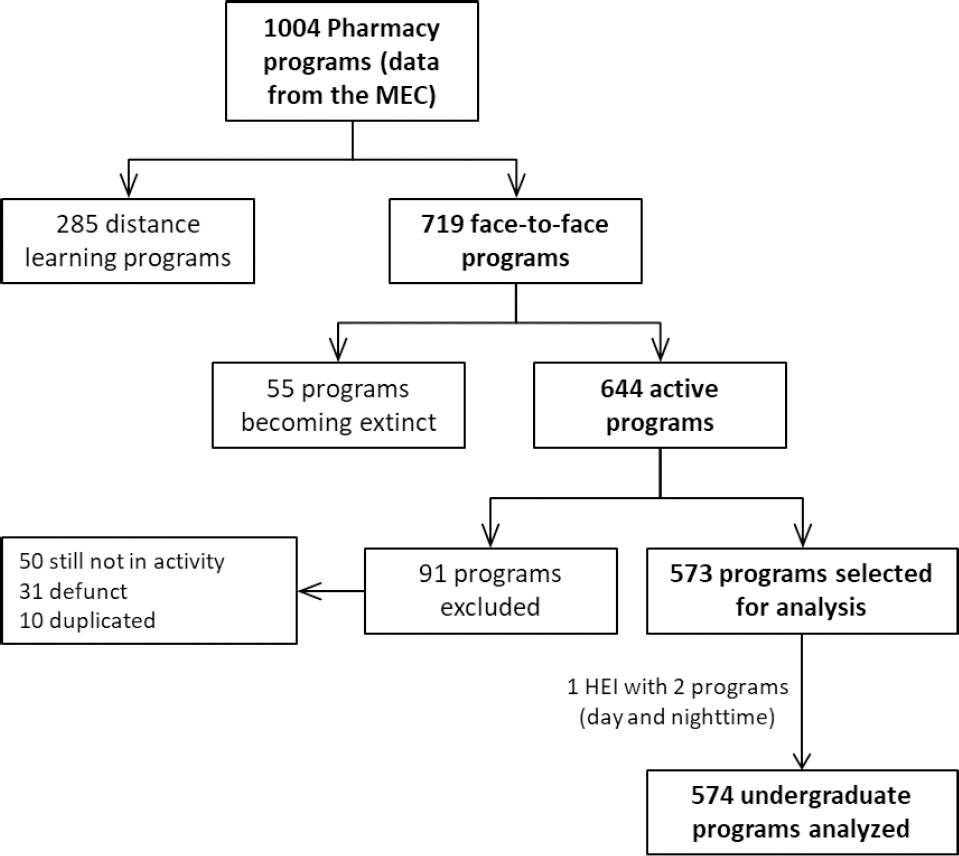
A search was conducted to identify HEIs in Brazil with a pharmacy undergraduate program, using a list of programs provided by the Ministry of Education (MEC), updated on July 24, 2018, double-checked for possible updates on the MEC website (e-Mec) in the data collection process. All face-to-face pharmacy undergraduate programs were considered eligible, whose first class had initiated prior to the data collection of this study. Exclusion criteria were e-learning programs, as well as extinct and closed programs.
Data collection
Data concerning internships were collected in January 2019 through a documentary analysis of the Political Pedagogical Projects of the pharmacy programs, curricula, course descriptions containing information on the internships, the HEIs websites, in addition to the data compiled and provided by the MEC. Specific data on the internships were collected only from the HEIs that provided such information on their websites.
Data were collected by two pharmacy students and reviewed by one of the researchers of the present study. The variables that were collected were grouped into three categories, as follows:
Data about the HEIs: geopolitical region of Brazil (north, northeast, center-west, southeast, and south); administrative category (private for-profit, private non-profit, federal public, state public, municipal public, and special); administrative dependency (public, private, or special); and whether they belong to private higher education groups (that manage higher education programs in several cities across the country).
Data about the pharmacy undergraduate programs: year of inauguration; length in semesters; number of openings offered annually; total hours - since the duration of a class varies among pharmacy programs, either 45, 50 or 60 minutes, the counting unit was converted into clock hours; class meeting times, comprising: fulltime - morning and afternoon (and occasionally evening) classes; daytime - either morning or afternoon classes; nighttime - evening classes only; daytime or nighttime - particular cases of pharmacy programs that offer two class times: daytime or nighttime, being up to the student to choose either one.
Data about the internships: number of internship periods; total hours; total hours by professional area; the semester in which the first internship starts; the semester in which the first internship starts by professional area. The internships were classified by practice scenario due to the lack of information about the competencies developed during them. In addition, due to overlapping activities in the same scenario, it was not possible to categorize the internships according to the pharmaceutical areas provided in the DCN. Thus, the internships were divided into: (1) technical visit: specific observations in the different areas of professional activity; (2) pharmaceutical technology: internships in medicine industries, regulatory agencies, or compounding pharmacies, whose function is the production of medicines and cosmetics; (3) clinical analysis: internships in clinical and/or toxicology laboratories; (4) food: internships in food industries; (5) hospital pharmacy: internships in a hospital environment, including management and care activities; (6) community and outpatient pharmacy: internships in private or public pharmacies, or clinics, where the student has direct contact with the patient for medicine dispensing and/or other pharmaceutical services; (7) SUS management and planning: internships in the SUS with emphasis on territorialization, health indicators evaluation, health planning, and pharmacy logistics activities; and (8) final internship: internship required in the final semesters of the program, which is when the student can choose a specific area of activity. The internships were further classified as: (1) compulsory: all students must pass in order to meet the regulations to be eligible to graduate; (2) elective: the student can choose whether or not to do an internship in that offered area; (3) not in the curriculum: when a given area does not have an internship offer in the program curriculum; and (4) not clearly defined: when the internship area of activity is not clearly defined.
Despite being considered as an internship event by some HEIs, on-campus experience projects, scientific initiation fellowships, scientific method activities, and complementary activities were not included in the present study.
Data analysis
The data collected were organized in Microsoft Excel® spreadsheets and analyzed using the SPSS program (IBM, Armonk) for Windows version 25.0. Categorical variables were represented by absolute and relative frequency and confidence interval of the proportion. Quantitative variables were represented by median and interquartile range (median [interquartile rank (IQR)]). The proportions of the internship variables were associated between Brazilian region, administrative dependency and administrative category by the chi-square test, and only categories with more than five HEIs were analyzed to yield accurate inference. In order to verify direct local association, standardized residuals analyses were performed with values greater than 1.96. For the internship variables, the distribution of total hours was compared between Brazilian region, administrative dependency and administrative category by the Mann-Whitney or Kruskal-Wallis test; the latter, when significant, was compared by the Dunn's peer-to-peer (post-hoc) test. The level of significance was set at 0.05.
RESULTS
Of the 1004 existing pharmacy undergraduate programs in Brazil, 573 (57.1%) were considered eligible and then included in the study. It should be pointed out that one of the HEIs had two pharmacy programs, a daytime one and a nighttime one, and with a different curriculum each, so they were counted as being two separate programs, which resulted in a total of 574 undergraduate programs evaluated.Figure 1below shows a sample selection flowchart.
An expressive increase in the number of new pharmacy undergraduate programs in Brazil have occurred since year 1995. Between 1995 and 2002, when the DCN were published, 111 new programs were opened; then 203 new programs between 2003 and 2010; and another 213 programs from 2011 until mid-2018. Such an increase over the years was higher among private HEIs (p<0.001). The highest concentration of pharmacy programs can be seen in the Southeast (40.8%, n=234), followed by the Northeast (22.8%, n=131), South (15.5%, n=89) (12.4%, n=71) and North (8.5%, n=49) of Brazil.
With regard to administrative dependency, only 12.7% (n=73) of the HEIs are public, of which 67.1% (n=49) are federal institutions, 23.3% (n=17) state institutions, and 9.6% (n=7) municipal institutions. Of the private HEIs that have a pharmacy program (n=499), 63.1% (n=316) belong to for-profit institutions, 36.5% (n=183) to non-profit institutions, and 0.4% (n=2) to special institutions. It is worth noting that pharmacy programs are free of charge in only 11.5% (n=66) of the HEIs, and 35.7% (n=205) of the HEIs analyzed belong to educational groups, being the following the main ones: Universidade Paulista (UNIP) (n=47), Kroton (n=55), Ser Educacional (n=35), and Estácio (n=12).
The distribution of pharmacy programs in the different regions of the country did not show a significant difference between private and public institutions. However, there was a significant difference between administrative categories and regions, with the South region having the lowest proportion (47.2%, n=42) of pharmacy programs in private non-profit HEIs; the greatest proportion being the Southeast region (40%; n=94). In addition, the Northeast region showed the highest proportion (71%; n=93) of private for-profit HEIs (Table 1).
Table 1. Comparison of the pharmacy programs distribution in Brazil by administrative category in the different regions of the country (N=572)
| Region of Brazil | p-value | |||||
|---|---|---|---|---|---|---|
| South | Southeast | Center-west | North | Northeast | ||
| Administrative category. n (%) | <0.001 | |||||
| Private non-profit | 42 (47.2) | 94 (40) | 16 (23.5) | 12 (24.5) | 19 (14.5) | |
| Private for profit | 32 (36) | 118 (50.2) | 43 (63.2) | 30 (61.2) | 93 (71) | |
| Federal public | 7 (7.9) | 16 (6.8) | 6 (8.8) | 5 (10.2) | 15 (11.5) | |
| State public | 5 (5.6) | 5 (2.1) | 2 (2.9) | 1 (2) | 4 (3.1) | |
| Municipal public | 3 (3.4) | 2 (0.9) | 1 (1.5) | 1 (2) | 0 | |
| Total | 89 (100) | 235 (100) | 68 (100) | 49 (100) | 131 (100) | |
*Comparison by Fisher's Exact Test; in bold, analysis of adjusted standardized residuals greater than 1.96
The programs have a median of 4099 total hours [4000.0; 4554.3], a median of 10 semesters [10.0:10.0], and a median of 102.5 [87.0; 200.0] openings offered annually. Most HEIs offer full-time pharmacy programs (20.6%, n=118), followed by nighttime programs (20.2%, n=116), and daytime programs (13.8%, n=79), and nighttime or daytime programs (12.9%, n=74). Only 51.2% (n=294) provide curriculum matrix, 16.6% (n=95) Political Pedagogical Projects and 18,6% (n=107) course descriptions on their websites.
Pharmacy internships
Of the 574 programs, 89 were excluded from the internship analysis because no information on such curricular component was found on their respective websites; however, the programs that provided some (even if not all) data were included, which generated different N throughout the analysis. The programs analyzed have a median of six internships, allocated from the 6th semester on, with a median of 826 hours in total. Regarding the 20% reserve of the total program hours to internships, as recommended by the DCN, 51 programs do not comply with that requirement.Table 2shows the general characteristics of the pharmacy internships.
Table 2. Internships in face-to-face pharmacy undergraduate programs in Brazil
| Median [IQR] | Min-Max | |
|---|---|---|
| Number of internships required (N=485) | 6 [4;7] | 1 - 17 |
| Semester when internships start (N=350) | 6 [4;7] | 1 - 10 |
| Total internship hours (N=455) | 826.0 [800.0; 940.0] | 216 - 1520 |
IQR: Inter quartile range
Not all programs provided information on the distribution of internships by area of professional activity; therefore, the data presented below comprise 326 programs (56.8%). In terms of mandatory requirements, internships are compulsory in pharmacy undergraduate programs, to a greater extent, in the areas of community and outpatient pharmacy (92.4%, n=291); clinical analysis (86.4%; n=273); pharmaceutical technology (83.5%, n=222), and, with the lowest proportion, food (37.4%, n=116) (Table 3). In 35 of the HEIs analyzed, there are compulsory internships in all those areas of professional activity. The HEIs whose curricula require a final internship correspond to 26.1% (n=85).
Table 3. Internships required in the curricula of pharmacy undergraduate programs in Brazil, in different areas of activity (n=326)
| Technical visit | Pharmaceutical technology | Clinical analysis | Food | Hospital pharmacy | SUS management and planning | Community and outpatient pharmacy | |
|---|---|---|---|---|---|---|---|
| Compulsory | |||||||
| n (%) | 84 (30.7) | 222 (83.5) | 273 (86.4) | 116 (37.4) | 184 (70.5) | 185 (69.3) | 291 (92.4) |
| IC[95%] | 25.4; 36.3 | 78.6; 87.6 | 82.3; 89.8 | 32.2; 42.9 | 64.8; 75.8 | 63.6; 74.6 | 89.1; 94.9 |
| Elective | |||||||
| n (%) | 0 (0) | 12 (4.5) | 8 (2.5) | 14 (4.5) | 14 (5.4) | 3 (1.1) | 9 (2.9) |
| IC[95%] | 0; 0 | 2.5; 7.5 | 1.2; 4.7 | 2.6; 7.3 | 3.1; 8.6 | 0.3; 3 | 1.4; 5.1 |
| Not in the curriculum | |||||||
| n (%) | 190 (69.3) | 32 (12) | 35 (11.1) | 180 (58.1) | 63 (24.1) | 79 (29.6) | 15 (4.8) |
| IC[95%] | 63.7; 74.6 | 8.5; 16.3 | 8; 14.9 | 52.5; 63.5 | 19.3; 29.6 | 24.4; 35.3 | 2.8; 7.5 |
| Not clearly defined | |||||||
| n (%) | 52 (16) | 60 (18.4) | 10 (3.1) | 16 (4.9) | 65 (19.9) | 59 (18.1) | 11 (3.4) |
| IC[95%] | 12.3; 20.2 | 14.5; 22.9 | 1.6; 5.4 | 2.9; 7.7 | 15.9; 24.5 | 14.2; 22.5 | 1.8; 5.8 |
Table 4displays the distribution of compulsory and elective internships by area of professional activity according to internship total hours. It should be stressed that the area with the highest internship total hours is clinical analysis.
Table 4. Internships according to the hours in the various areas of professional activity
| Overall hours | Private HEI hours | Public HEI hours | p-value | ||||
|---|---|---|---|---|---|---|---|
| median [IQR] | range | median [IQR] | range | median [IQR] | range | ||
| Technical visit (n=81) | 80 [60:80] | 25 - 128 | 80 [80:80] | 25 - 120 | 52.5 [42.5:74] | 30 - 128 | 0.142 |
| Pharmaceutical technology (n=222) | 124 [120:213] | 45 - 558 | 120 [120:210] | 50 - 558 | 150 [120:226] | 45 - 540 | 0.359 |
| Clinical analysis (n=269) | 200 [120:240] | 50 - 720 | 210 [120:240] | 60 - 550 | 180 [120:300] | 50 - 720 | 0.968 |
| Food (N=116) | 120 [99:145] | 34 - 720 | 120 [100:120] | 34 - 286 | 145 [81:250] | 50 - 720 | 0.038 |
| Hospital pharmacy (n=190) | 90 [60:120] | 40 - 270 | 90 [60:120] | 40 - 270 | 120 [90:160] | 40 - 270 | 0.016 |
| SUS management and planning (n=181) | 102 [75:200] | 20 - 320 | 109 [80:200] | 20 - 320 | 90 [61.5:120] | 30 - 235 | 0.02 |
| Community and outpatient pharmacy (n=289) | 160 [120:280] | 30 - 720 | 160 [120:300] | 40 - 720 | 160 [96:195] | 30 - 375 | 0.041 |
| Final internship (n=85) | 415 [360:523] | 67-1025 | 410 [300:495] | 67 - 600 | 466 [360:600] | 120 - 1025 | 0.018 |
*Comparison of hours between private and public HEIs, by the Mann-Whitney Test
SUS: Brazilian National Health Service
As regards the moment in the program when students are required to do internships, technical visits are held more frequently at the beginning of the program; pharmaceutical technology, hospital pharmacy, community pharmacy/outpatient pharmacy start predominantly in the second half of the program; internships in clinical analysis and food are done in the last three semesters of the program; and the internships in SUS management and planning do not follow a pattern among the pharmacy programs (Figure 2).

Figure 2. Internships by area of professional activity according to the semester in which they start, as provided for in pharmacy curricula in Brazil
There was a statistically significant difference of internships by area of professional activity between public and private HEIs, with private HEIs having higher proportions of compulsory internships in the areas of pharmaceutical technology (p<0.001), clinical analysis (p<0.001), hospital pharmacy (p=0.002), SUS management and planning (p=0.022), and community and outpatient pharmacy (p<0.001). Public HEIs showed a higher proportion only in the final internship category (p<0.001).
As for the number of internships by area in the different regions of Brazil, there was a significant percentage of internships in the area of community and outpatient pharmacy in all regions of the country. The South region presented a higher proportion of compulsory final internships (p<0.001) and fewer internships in the areas of pharmaceutical technology (p=0.022) and clinical analysis (p=0.002). The Southeast region presented fewer internships in the area of SUS management and planning (p=0.029) and final internships (p<0.001). The Northeast region presented the highest proportion of compulsory internships in the area of clinical analysis (p=0.002).
DISCUSSION
In the last decades, to industrialization, increased drug-related morbidity and mortality, and the expansion of health expenditures and related supplies, thus marking the beginning of a new era for pharmaceutical practice.18In view of that, the pharmacist profession has evolved from a product-oriented to a patient-oriented. These changes require pharmacy education to prepare and organize programs that develop the skills required by that new social role.19In this regard, in order to support improvements in pharmacy education, the International Federation of Pharmacists (FIP) has published the document Global Competency Framework, which contains specific competencies in pharmacy education and training.20
Based on this principle, several countries have discussed pharmacy education and implemented curriculum reforms with emphasis on competencies and training of professionals properly qualified for the fulfillment of their duty to ensure positive health outcomes by means of medicines. In some countries, this process has been faster, such as in Canada, the United States, and Australia; in others the process is recent.21 22 23 24-25In Brazil, the new DCN have pushed forward the discussion of the competencies that should be developed in pharmacy undergraduate programs. However, competency standardization for pharmacy professionals - so as to provide real support in reformulating education, as in Australia, Canada and Ireland - remains far from happening in Brazil.26 27-28
In terms of competency development, several studies have pointed out the positive impact of students' inclusion in real environments.29 30 31-32The increase in the extent and quality of experiential education and the introduction of varied teaching techniques are indispensable prerequisites for ensuring high quality standards in the teaching process of pharmacy programs.21In this sense, experiential education can be seen as fundamental to the development of professional competency.
In Brazil, the disorderly increase in pharmacy undergraduate programs in the last decades can lead students to competition for best internship places and, thus, affect the success of the teaching-learning process.33This increase in the number of pharmacy programs is possibly a worldwide phenomenon. Literature has demonstrated such growth in countries such as the United States, India, Chile, and Middle East countries.25,33,34According to the FIP, between 2006 and 2016 there was an increase in the number of pharmacists per capita in all regions of the world.35Additionally, as the data in this study point out, the increase in pharmacy programs in Brazil is strongly influenced by the model practiced by private educational groups, which use the same curriculum for all programs, regardless of regional specificities, which can be detrimental since private HEIs are rated worse than public HEIs in terms of quality.36Kheiret al. emphasize that, although the expansion of pharmacy programs in for-profit institutions may be favorable, this increase must be controlled in an attempt to ensure the quality of education.34
Furthermore, studies carried out by Carvalho and Leite (2016) and Vieira and Moyses (2017) point out that this increased number of openings offered annually in pharmacy programs in Brazil has been accompanied by the imbalance between the number of openings versus graduates - with an exponential increase in the number of unfilled openings, being 4,120 in 2001, 26,623 in 2011and 30,417 in 2015 - in addition to the relationship graduates versus dropouts - in 2015, 42.0% (10.617) of pharmacy undergraduates did not complete the program.15,37
The results of this study evince the lack of uniformity among the pharmacy undergraduate programs in Brazil, mainly concerning total hours and the semesters in which they begin. In addition, it was found that, predominantly in private HEIs, priority was given to internships with a small amount of total hours. This prevents students from developing proficiency in the competencies required for their professional practice, since practical experiences are not offered in sufficient duration and with increasing complexity throughout the program. Ultimately, internships have provided, for the most part, only experiences rather than learning per se. According to Kolb, knowledge is constructed on the basis of lived experiences, and the opportunity for students to experience and practice the profession from the beginning of the program contributes to the development of integrative consciousness - the most complex level of development of primordial human consciousness for the development of professional competencies.16
In the United States, Canada, Australia and New Zealand, experiential education is generally focused on developing competencies for patient care process in hospital and community practice settings, with increasing levels of responsibility from beginning to end of the program and with learning outcomes clearly defined in the curriculum.23,24,38In Europe, according to the Bologna Declaration, experiential education is offered during or at the end of theoretical and practical training, at a pharmacy open to the public or at a hospital under the supervision of the pharmacy professionals of the area.39Although in some countries it is possible for students to do internships in other areas of interest, health care settings, mainly community pharmacies and hospitals, are still the priority places for experiential learning.24
In Brazil, the settings where internships are usually carried out, to a greater extent comprise, respectively, the areas of community and outpatient pharmacy, clinical analysis, and pharmaceutical technology, being clinical analysis internships more extensive in terms of total hours. It is also worth noting that, unlike in other countries, internships in the food area are still a part of some curricula in Brazil, and with a high amount of hours.23,24,38,39This form of structuring the internships - by areas according to old areas of emphasis in the curricula - is still supported by the DCN.11This fact reinforces the influence of the professors, who graduated under that model, on the making of new curricula. Consequently, this scenario may point to a long curriculum reform process permeated by tensions, similar to what is happening in Argentina.40
Thus, the low number of hours of internships in possible scenarios of clinical practice and its late onset, which does not allow for increasing skills development, could be contributing to a small number of pharmacists who are skilled and knowledgeable of clinical practice, as most are disconnected from patient needs and health services, hence the lack of recognition of the pharmacist's potential and professional value in the health team.18,41Thus, despite the advances in education, pharmacy schools in Brazil have also trained pharmacists with a profile that is far from what the FIP recommends and from what many countries have adopted.1,20
According to a survey by the Brazilian Federal Council of Pharmacy (2015), 81.1% of pharmacists in Brazil work in pharmacies or drugstores, of which 64.1% perform management services such as inventory control and drug procurement, while only 17.8% perform clinical services.42This reinforces the results of other studies that argue that clinical practice in Brazil is still incipient and characterized by the professionals' personal effort and improvisation, contrasting with the scenario of some European countries and the USA, with well-structured services covered by health insurance plans.41,43 44-45
Pharmacy undergraduate programs in Brazil should prioritize the training of well-qualified graduates to work in the areas that concentrate most of the pharmacist workforce - i.e. community pharmacies - and make efforts to ensure that education is in line with international recommendations, providing training in the field of care pharmaceutical. In this way, Brazil, as well as other countries experiencing a delayed implementation of pharmaceutical care services, should prioritize the creation of experiential education programs in settings that favor the qualification of professionals to work in this area. This should also include an adequate amount of course hours and structures that guarantee the growing development of their skills and competencies, to act efficiently for the well-being of patients and society.
The major challenge of the present study was to collect data from the HEIs websites, many of which were out of date, incomplete or inaccurate, and very usually provided no information. This scenario makes it difficult to compare these data with those of other studies, such as Nunes-da Cunha.46This problem is not exclusive to pharmacy programs in Brazil, as it was also reported in a study that evaluated pharmacy education in Middle East countries.34The obligation of this transparency should be assumed as a priority agenda by the Ministry of Education as a way to contribute to the improvement in the quality of higher education in Brazil. In addition, Brazilian HEIs do not follow a syllabus template for their curriculum presentation, which if so, according to literature, would make them improve on quality.47The pharmacy undergraduate curricula in Brazil do not fully describe educational objectives, competencies to be achieved, assessment and teaching methods, thus making it difficult to carry out educational studies, which are extremely relevant to evaluate education itself and the impacts of the DCN implementation.
CONCLUSIONS
This study points to heterogeneity among internships pharmacy undergraduate programs in Brazil. There is a significant number of internships in community and outpatient pharmacies in all pharmacy undergraduate programs in Brazil, which may reflect the trends in the pharmacist workforce in Brazil. In addition, there is still a strong influence of the old areas of emphasis in the curricula, evinced by the presence of internships in the area of clinical analysis and food. In general, too few course hours are dedicated to the internships and they are undertaken predominantly at the end of the pharmacy program, that is, there is no experiential education program that envisions the acquisition of professional competencies throughout the pharmacy program.
In view of the importance of experiential education for the development of professional competencies, and given the difficulty in obtaining information on pharmacy programs in Brazil via the HEIs website, there is a need for further studies that encompass other methodological approaches for an in-depth scrutiny of the internships, in a way to understand the interface of this curricular component with the program itself and to analyze how the teaching-learning-assessment process takes place.