INTRODUCTION
Pharmacogenomic research and implementation have increased in recent years as healthcare moves towards precision medicine.1 A driving force behind pharmacogenomics are drug-gene interactions that affect the patient’s response to a medication and may inform treatment choices.2 Currently, there are several published guidelines on drug-gene interactions from the Clinical Pharmacogenetics Implementation Consortium (CPIC), which provide specific dosing recommendations with a corresponding level of evidence.3 Additionally, the Food and Drug Administration (FDA) has published a compiled table of gene-drug interactions of significance.4
As the medication expert on interdisciplinary teams, pharmacists are well positioned to drive this implementation. The American Society of Health-System Pharmacists (ASHP) has called for “pharmacists to take on a prominent role in the application of pharmacogenomics”.3 Accordingly, pharmacogenomic educational elements were recently incorporated into the accreditation standards for the didactic Doctor of Pharmacy curriculum starting in 2011 by the Accreditation Council for Pharmacy Education (ACPE). Thus, many practicing pharmacists who graduated prior to implementation of these standards may have inadequate exposure to pharmacogenomics in general, as evidenced by a recent survey showing that older pharmacists are less aware and less confident in their knowledge of pharmacogenomics.5,6 An additional survey in the Netherlands found that the biggest barrier to implementation of pharmacogenomics by pharmacists is a lack of knowledge.7
Other health care professionals have also expressed a lack of knowledge and experience with pharmacogenomics. A prior survey of primary care providers (e.g., physicians, nurse practitioners, and physician assistants) in the same large, multi-state, health system as the survey presented herein showed a lack of comfort ordering and interpreting pharmacogenomic results. This survey also demonstrated a high level of support for testing being offered through pharmacy services as well as concerns regarding cost and insurance coverage, evidence and benefits of testing, and a general lack of knowledge on pharmacogenomics testing.8
While several pharmacy organizations have expressed support of pharmacists leading implementation of pharmacogenomics, there are a lack of surveys specifically asking pharmacists their opinions of implementing pharmacogenomics and how their own knowledge and experience may impact this. Thus, the primary objective of this survey was to determine how post-graduate education and training and other factors influence pharmacist’s knowledge and attitudes of pharmacogenomic testing.
METHODS
Survey development
This survey was developed as a follow-up to a previous survey at the same institution of prescribing primary care clinicians (e.g. MDs, DOs, NPs, and PAs) to ascertain pharmacist’s attitudes and knowledge of pharmacogenomic testing.8 The thirteen-question survey was developed by the study team consisting of two pharmacists with pharmacogenomics expertise, two ambulatory care pharmacists, an acute care pharmacist, a research scientist, a study coordinator, and a pharmacy student. Questions were asked to pharmacists to determine information on their attitudes, comfort level, and knowledge regarding pharmacogenomics. Respondents self-reported gender, year of graduation with highest clinical degree, post-graduate training, board certification, primary practice site, full-time equivalent employment hours, time spent performing different pharmacy-related activities, and their prior pharmacogenomics education. This survey was developed and validated internally by the study team based on experience and expertise, as well as on the previous pharmacogenomics survey administered to prescribing clinicians. The full version of the survey can be found in the supplemental materials.
Sampling methods
This survey was sent to all pharmacists in a large, multi-state health system by pharmacy management through a pharmacy list serve. Study data were collected and managed using REDCap™ electronic data capture tools.9
The survey link was sent out by email and was open for a total of four weeks. A reminder email was sent out one week prior to the survey closing. Responses were anonymous through an automatically generated participant ID in REDCap™.
Data analysis
Survey results were compiled into data tables with frequencies for each survey question. Frequencies were stratified based on demographic parameters to determine differences between rural and urban pharmacists, year of graduation, post-graduate training, practice area, and previous education in pharmacogenomics.
Chi-squared tests were used to test statistical significance between groups analyzed. Nominal logistical regression was used to assess demographic and pharmacy training factors associated with survey responses. Statistical significance was defined as p-value <0.05 using 95% confidence intervals. JMP® Pro 14 was used for all statistical analyses.
RESULTS
The survey was distributed to a total of 161 pharmacists with 75 (47%) completing all aspects. No surveys were returned incomplete. Complete demographic information of survey respondents is listed in Table 1. Of the respondents, 60% were female and 43% graduated with their clinical degree after the year 2010. For post-graduate training and education, 36% of respondents completed a Post-Graduate Year One (PGY-1) residency and 27% were board certified. Of 19 pharmacists that are board certified, seven were Board Certified Pharmacotherapy Specialists (BCPS), six were Board Certified Ambulatory Care Pharmacists (BCACP), one was a Board Certified Cardiology Pharmacist (BCCP), two were Board Certified Oncology Pharmacists (BCOP) and three reported other board certification. Eighty percent of respondents worked a full-time equivalent (FTE) and 85% worked in an urban area.
Table 1. Demographics of respondents
| N (%) | |
|---|---|
| Gender | |
| Female | 44 (60.3) |
| Male | 29 (39.7) |
| Not Reported | 2 (2.7) |
| Year of Graduation with highest clinical degree | |
| 2010-2018 | 32 (42.7) |
| 2000-2009 | 24 (32) |
| Before 2000 | 18 (24) |
| Not Reported | 1 (1.3) |
| Did you receive post graduate training? | |
| Yes | 30 (40) |
| No | 45 (60) |
| What type of post graduate training did you receive? (select all that apply) | |
| PGY-1 | 27 (90) |
| PGY-2 | 0 (0) |
| Fellowship | 2 (6.7) |
| Other | 2 (6.7) |
| Do you have a Board Certification? | |
| Yes | 20 (26.7) |
| No | 55 (73.3) |
| Current Practice Site Based on RUCA Score* | |
| Rural | 10 (15.2) |
| Urban | 56 (84.8) |
| Not Reported | 9 (12) |
| Current FTE | |
| Full-time | 60 (80) |
| Part-time | 15 (20) |
| Primary Practice Setting (select all that apply) | |
| Ambulatory Care Clinic | 18 |
| Outpatient Pharmacy | 13 |
| Acute Care Pharmacy | 43 |
| Clinical Management | 3 |
| Operations Management | 5 |
| Other (i.e. home health/infusion pharmacies, nuclear, telephone, or mail service, etc.) | 5 |
*RUCA= Rural-Urban Commuting Area
The majority of respondents (75%) had not received any formal training or education on pharmacogenomics. Of those that had received formal training or education, the most common method was through their school curriculum. When asked about current knowledge of pharmacogenomic resources and guidelines, over half (58%) did not feel knowledgeable. Most respondents indicated they would consult drug resources (64%) and colleagues with expertise (52%) when interpreting pharmacogenomic test results.
Survey questions and responses are listed in Table 2. Nearly 20% of pharmacists recalled a patient or provider bring them a pharmacogenomic test result for consult on dosing recommendations or medication selection; however, 65% stated they were uncomfortable recommending pharmacogenomic tests to providers and patients. When asked about interpreting results of a pharmacogenomic test, 62% were uncomfortable. Furthermore, 59% of respondents felt uncomfortable providing recommendations to a provider or patient based on pharmacogenomic test results and 58% of pharmacists were unsure on where to best document pharmacogenomic test information in a patient’s electronic medical record.
Table 2. Survey questions and responses
| N (%) | |
|---|---|
| 1. Have you received any formal training or education on pharmacogenomics? | |
| Yes | 18 (24) |
| Unsure | 1 (1.3) |
| No | 56 (74.7) |
| 2. How comfortable do you feel recommending pharmacogenomic tests to providers and patients? | |
| Very comfortable | 5 (6.7) |
| Somewhat comfortable | 12 (16) |
| Neither comfortable nor uncomfortable | 9 (12) |
| Somewhat uncomfortable | 21 (28) |
| Very uncomfortable | 28 (37.3) |
| 3. How comfortable are you interpreting the results of a pharmacogenomic test? | |
| Very comfortable | 4 (5.3) |
| Somewhat comfortable | 15 (20) |
| Neither comfortable nor uncomfortable | 10 (13.3) |
| Somewhat uncomfortable | 16 (21.3) |
| Very uncomfortable | 30 (40) |
| 4. How comfortable do you feel providing recommendations to a provider or patient based on pharmacogenomic results? | |
| Very comfortable | 4 (5.3) |
| Somewhat comfortable | 12 (16) |
| Neither comfortable nor uncomfortable | 15 (20) |
| Somewhat uncomfortable | 18 (24) |
| Very uncomfortable | 26 (34.7) |
| 5. How would you assess your current knowledge of pharmacogenomic resources and guidelines? | |
| Knowledgeable | 5 (6.7) |
| Somewhat knowledgeable | 23 (30.7) |
| Not knowledgeable | 44 (58.7) |
| Unsure | 2 (2.7) |
| Not reported | 1 (1.3) |
| 6. Which sources would you consult when interpreting pharmacogenetic test results? | |
| Medical Association meetings/Guidelines/Recommendations | 29 (38.7) |
| Scientific Literature | 35 (46.7) |
| Drug Resources (e.g. Micromedex, Lexicomp, etc.) | 48 (64) |
| Internet | 21 (28) |
| Drug Labeling/FDA website | 22 (29.3) |
| Colleague with expertise | 39 (52) |
| Other | 6 (8) |
| 7. Has a patient or provider brought a pharmacogenomic test result to you for guidance in medication dosing or selection or to explain previous medication experiences? | |
| Yes | 12 (16) |
| Unsure | 2 (2.7) |
| No | 61 (81.3) |
| 8. How significant of an impact do you believe pharmacogenomics has on current practice? | |
| Very significant | 12 (16) |
| Somewhat significant | 31 (41.3) |
| Neither significant nor insignificant | 10 (13.3) |
| Somewhat insignificant | 14 (18.7) |
| Very insignificant | 8 (10.7) |
| 9. How would (have) you document(ed) pharmacogenomic test results in a patient’s electronic medical record? (Check all that apply) | |
| Enter notes into electronic health record | 25 (33.3) |
| Scan test results into the electronic health record | 24 (32) |
| List major findings as an allergy | 14 (18.7) |
| List major findings in the problem list | 13 (17.3) |
| Flagging a medication that has CPIC guidance | 10 (13.3) |
| Unsure | 44 (58.7) |
| Other | 5 (6.7) |
| If other, please describe: | |
| • Add a flag to the header in the patient chart along with allergies, ht, wt, CrCl, etc. | |
| • Ivent of recommendations, did not scan information into chart | |
| • Kept out of chart due to current protocol issues | |
| • Lab results | |
| • Near microbiology section in results | |
| 10. Do you support offering pharmacogenomic testing and interpretation though Pharmacy Services? | |
| Yes | 54 (72) |
| Unsure | 19 (25.3) |
| No | 2 (2.7) |
| 11. Would you want a decision support tool to alert you to potential drug-gene interactions in patients with pharmacogenomic results? | |
| Yes | 67 (89.3) |
| Unsure | 8 (10.7) |
| 12. What barriers do you think are preventing/slowing the implementation of pharmacogenomic services? | |
| Insurance | 44 (58.7) |
| Willingness to take on a new task | 23 (30.7) |
| Education | 66 (88) |
| Process of ordering to putting in the medical record | 32 (42.7) |
| Limited resources for interpretation and application of pharmacogenomic test results | 58 (77.3) |
| 13. Do you agree with the following statement: Pharmacists are the best suited clinicians to implement pharmacogenomic testing. | |
| Yes | 44 (58.7) |
| Unsure | 29 (38.7) |
| No | 2 (2.7) |
| If yes, where within the practice of pharmacy is pharmacogenomics the best suited? | |
| Acute and Ambulatory | 2 (5.4) |
| Ambulatory Care | 17 (45.9) |
| Clinical Pharmacists | 7 (18.9) |
| Multiple areas of pharmacy | 3 (8.1) |
| Specialists that achieved certification | 1 (2.7) |
| Specialty Clinics (behavioral health, oncology, neurology, cardiovascular) | 6 (16.2) |
| Unsure | 1 (2.7) |
Fifty-seven percent of pharmacists felt that pharmacogenomics does have a significant impact on current practice. Additionally, 89% of respondents supported a clinical decision support tool to alert them to potential drug-gene interactions while the other 11% were unsure. When asked about barriers to implementation of pharmacogenomic testing, education (88%) and limited resources (77%) were the two biggest factors noted.
In total, 58% of pharmacists surveyed agreed that pharmacists are the best suited clinicians to implement pharmacogenomic testing, while 39% percent were unsure. Of those who felt pharmacists were best suited, most felt that it should be implemented in the ambulatory care or clinical pharmacy areas of pharmacy services.
Those that completed a PGY-1 were significantly more likely to have received formal training or education on pharmacogenomics than those who had not (p=0.02) (Figure 1A), and assessed their own knowledge of pharmacogenomic resources and guidelines higher than those without a PGY-1 (p=0.03). More recent graduates were significantly more likely to have received formal training or education on pharmacogenomics (p<0.0001) (Figure 1B). Female respondents were significantly more likely to be supportive of pharmacogenomic testing and interpretation through pharmacy services as compared to males (p=0.005) (Figure 1C), and were also more likely to have graduated after 2005 (p=0.001). Additionally, pharmacists who completed a PGY-1 residency were more likely to respond favorably to pharmacogenomics being offered through pharmacy services (p=0.01) (Figure 1D) and a decision support tool to alert them to drug-gene interactions (p=0.04) (Figure 1E) as compared to pharmacists without PGY-1 training. In the same comparison, they also agreed pharmacists are the best suited clinician to implement pharmacogenomic testing (p=0.01) (Figure 1F). Pharmacists with board certification were more comfortable interpreting results of a pharmacogenomic test than those without board certification (p=0.02).
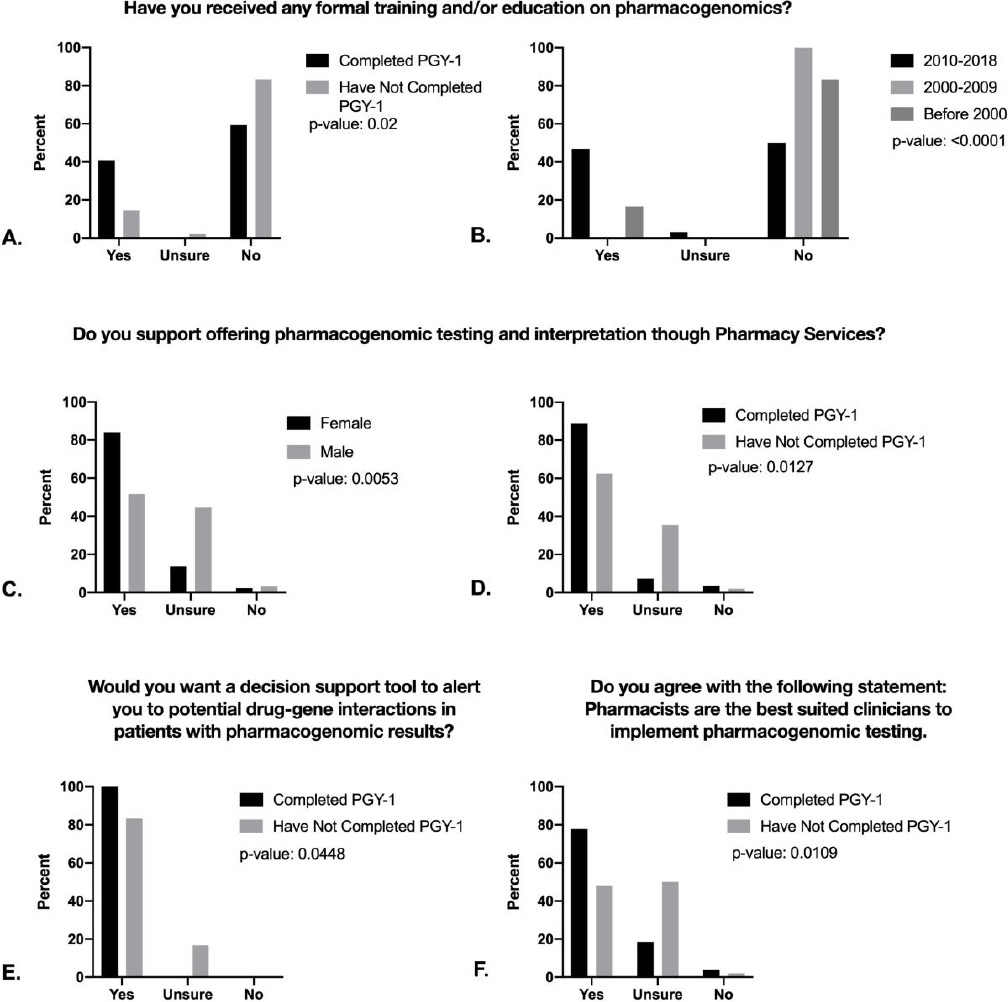
All demographics were analyzed for each question using a Fisher’sexact test with a p-value <0.05. Graphs A and B show the difference between graduation year (p <0.0001). and completion of a PGY-1 (p= 0.0222) in responses to having formal education and/or training in pharmacogenomics. Graphs C and D show the differences that gender (p=0.0053) and completion of a PGY-1 (0.0127) have on pharmacist support for pharmacogenomic testing and interpretation being offered at Pharmacy Services. Graph E depicts the difference completion of a PGY-1 (p=0.0448) has on support for a clinical decision support tool. Graph F shows how the completion of a PGY-1 (p=0.0109) leads to more agreement with the statement “pharmacists are the best-suited clinicians to implement pharmacogenomic testing.”
Figure 1. Questions stratified based on demographics
Year of graduation was independently associated with receipt of formal PGx training (p<0.01), while gender (p=0.99) and PGY1 training (p=0.61) was not. Female gender was independently associated (p=0.02) with supporting PGx service through pharmacy services and those with PGY-1 training were also more likely to be supportive; however, this did not meet significance (p=0.12). Year of graduation, gender and PGY-1 training was not associated with agreement that pharmacists are the best suited clinicians to implement PGx testing.
DISCUSSION
In general, pharmacists surveyed reported pharmacogenomic testing to have a somewhat or very significant impact on current practice. In spite of this, only 58% thought pharmacists were the best suited clinician to implement pharmacogenomic testing into practice. Consistent with prior surveys, the biggest barriers to implementation were identified as limited resources and education, supported by the finding that most pharmacists do not feel comfortable ordering or interpreting a pharmacogenomic test and would need additional education.6,7 Most notably, pharmacists with more post-graduate training (e.g. residency or board certification) were more comfortable in interpreting and recommending results as compared to those without, while no respondents were against a clinical decision support tool to aid in identifying drug-gene interactions. Post-graduate education and training was also associated with more knowledge and comfort in pharmacogenomics testing. To the best of our knowledge, this is the first survey to assess the impact of post-graduate education and training on attitudes and knowledge of pharmacogenomic testing amongst pharmacists.
Although most pharmacists surveyed felt that they are the best suited clinicians to implement pharmacogenomic testing, a surprisingly high number (39%) were unsure. In our previous survey, 73% of primary care clinicians were interested in pharmacogenomics testing being available through the Medication Therapy Management Program, which is consistent with the responses of pharmacists herein.8 The uncertainty pharmacists have in implementing pharmacogenomics in their own practice may be due to inadequate education and will need to be further discussed to ensure that pharmacists are confident in this field prior to implementation. Of note, acute care pharmacists, a number of whom completed this survey, may recognize the importance of pharmacogenomics but not feel that it should be emphasized in their setting as much as ambulatory care. Additionally, pharmacists working as generalists, who made up the majority of the respondents herein, may not see as great of an impact as a specialist on the need to be knowledgeable in pharmacogenomics.
According to AACP in 2017, 62% of PharmD graduates were female, which was consistent with the demographics seen in this survey.10 Interestingly, female respondents were more likely than males to be supportive of pharmacogenomic testing and interpretation through pharmacy services.
The results of this survey are similar to previous findings amongst hospital pharmacists regarding pharmacogenomic testing. Previous surveys found that most pharmacists believed that pharmacogenomics will benefit their patients. Those pharmacists were also interested in continuing education, as they lacked confidence in their ability to use pharmacogenomic information. The variable most likely predict a pharmacist’s adoption of pharmacogenomics into their practice was confidence in their ability to counsel patients on their test results.6
Similar to the reported survey, primary care clinicians have also reported that pharmacy services should take on the role of implementing pharmacogenomics, specifically in the ambulatory care setting. They similarly supported a clinical decision support tool and more education regarding pharmacogenomic testing.8 An additional study in the Netherlands found that despite having a clinical decision support tool containing the nationwide guidelines, implementation of pharmacogenomics was less than expected because pharmacists did not feel adequately informed on pharmacogenomics.7 Although clinical decision support impacts usability of pharmacogenomic information in the medical record, without basic education on pharmacogenomics it may not have a meaningful impact on implementing testing.
More recent graduates reported more education in pharmacogenomics than more experienced pharmacists, possibly as a result of recent requirements to include didactic pharmacogenomic educational elements within pharmacy school curriculums. However, survey participants who had completed a PGY-1 noted greater comfort with pharmacogenomics, while no differences were seen with year of graduation and level of comfort with pharmacogenomics. Per the most recent accreditation standards set by ASHP for PGY-1 Residencies, there are no specific requirements for education on pharmacogenomic testing.11 The increased comfort seen with pharmacists that completed a PGY-1 may be due to other factors associated with completing a residency such as experience in specialty areas and not the residency itself, suggesting that more practice-based experiences may be needed to increase pharmacists comfort level with pharmacogenomics.
For pharmacists already in practice, there are numerous pharmacogenomics certificate programs administered by pharmacy associations, health systems and colleges of pharmacy to help pharmacists increase their knowledge in this area. Other continuing education and site-specific trainings can also aid in pharmacists obtaining competencies in pharmacogenomics. For example, a pharmacogenomics educational program developed at the Mayo Clinic to educate their pharmacists was well received, showed a positive influence in pharmacy practice, and a significant increase in competency based on a pre and post-test on pharmacogenomics.12
Perhaps the most effective method of retaining pharmacogenomics education is practice-based application of pharmacogenomic concepts.13 Pharmacogenomic certificate training programs have been shown to raise pharmacist’s perceived competence related to specific drug-gene interactions in simulated patient encounters.14 Traditional continuing education methods have proved to not be as effective since it has been shown that pharmacists don’t change their behaviors afterwards.13
This study was limited by several factors. First, the distribution of pharmacists responding to the survey was not uniform, as the majority came from more urban areas and not all pharmacies in the health-system were represented. Second, the survey was localized to one health-system and not externally validated. Finally, while there were respondents representing several practice areas of pharmacy, the majority of respondents practiced in the acute care setting.
CONCLUSIONS
In summary, pharmacists with more post-graduate education and training responded more favorably to taking on pharmacogenomic testing. In order to best implement wide-spread testing, pharmacists with post-graduate training could be utilized first as a basis of knowledge for adoption of pharmacogenomics programs. Increased visibility and usage of educational resources will be needed for the majority of pharmacists to have a baseline knowledge of pharmacogenomic testing.














